International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Anwar Tahir Buta1, Abulie Takele Melku1* and Geroma Morka Donka2
1Madda Walabu University Goba Referral Hospital School of Health Science, lecturer.
1Madda Walabu University Goba Referral Hospital School of Health Science.
2Madda Walabu University Goba Referral Hospital School of Health Science.
*Corresponding authors: Abulie Takele Melku, 1Madda Walabu University Goba Referral Hospital School of Health Science, lecturer.
Received: March 31, 2021
Accepted: April 02, 2021
Published: April 06, 2021
Citation: Anwar T Buta, Abulie T Melku, Geroma M Donka,. “Uncontrolled Hypertension and Its Associated Factors Among Hypertensive Patients on Follow-Up in Bale Zone Hospitals, Southeast Ethiopia”. International Journal of Epidemiology and Public Health Research, 1(1); DOI: http;//doi.org/03.2021/1.1004.
Copyright: © 2021 Abulie Takele Melku. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background:-The prevalence of uncontrolled hypertension among hypertensive patients is high and the reason for uncontrolled hypertension is not well understood globally. It raises the risk of cardiovascular diseases, stroke, and chronic kidney disease causing morbidity and mortality.
Objective:-To assess the prevalence of uncontrolled hypertension and its associated factors among hypertensive patient on follow up in Bale Zone Hospitals, Southeast Ethiopia.
Methods:- A facility-based cross-section study was conducted in five Bale Zone Hospitals from March to April 2020 after Pretest. Systematic random sampling was used for the selection of 421 participants. Data were collected through face-to - face interviews using a semi-structured questionnaire. Data was entered in Epi data version 3.1 and analyzed in SPSS version 25. Descriptive statistics, bivariate and multivariate analysis was done and p-value < 0.05 at 95%CI was considered statistically significant.
Result:- In this study, 57% of the 412 participants had uncontrolled hypertension. The average age of respondents was 53.8±11.9 SD years. Experience with medicinal side effects (AOR=1.975, 95% CI: 1.056-3.695), Comorbidities (AOR=1.988, 95% CI, 1.026-3.85), physical inactivity (AOR=1.972, 95 % CI: 1.185-3.282), salt use (AOR=1.914, 95% CI: 1.106-3.313), fruit and vegetables not consumed (AOR=6.106, 95% CI: 1.261-29.569) were positively associated with uncontrolled hypertension. Whereas family or other care assistance (AOR=0.485, 95 % CI: 0.266-0.886) and unconsumed fat (AOR=0.249, 95 % CI: 0.135-0.459) were adversely correlated with uncontrolled hypertension.
Conclusion:- The prevalence of uncontrolled hypertension in five public hospitals in the Bale Zone was large. Experience with side-effect treatment, salt use, not eating fruit and vegetables, physical inactivity and comorbidity were positively associated with uncontrolled hypertension while relatives or other caregivers and non-consumers with fat were negatively associated with uncontrolled hypertension. Educating patients about a healthy lifestyle and the treatment of hypertension related complications is required.
Background
Uncontrolled hypertension is characterized as sustained high blood pressure (Systolic blood pressure greater than or equal to 140 mmHg and/or diastolic blood pressure greater than or equal to 90 mmHg for individuals less than 60 years of age) and systolic blood pressure greater than or equal to 150 mmHg and/or diastolic blood pressure greater than or equal to 90 mmHg for individuals 60 years of age.
According to WHO 2017 study, reducing hypertension decreases the risk of stroke by 30%, myocardial infarction by 25%, chronic kidney disease by 23% (WHO, 2017a). However, several studies in various parts of the world have shown that the prevalence of uncontrolled hypertension among hypertensive follow-up patients is large. In Thailand, 54.4% of hypertensive patients accompanied by uncontrolled hypertension(Suprawee Meelab et al., 2019). In China, the prevalence of uncontrolled hypertension among hypertensive patients was 55.4% (Li Yang et al., 2014).
Uncontrolled hypertension is becoming a health issue in developing countries, including Ethiopia. According to the WHO study on NCDs (non-communicable diseases), the leading cause of death from NCDs in Ethiopia was cardiovascular disease. Hypertension was at risk for 15.9% of the adult population, of which about 14.4% of hypertensive patients had uncontrolled hypertension in Ethiopia (Fassil shiferaw, 2019). In Ethiopia, NCDs account for 42% of morbidity, 27% of premature death (death before 70 years of age), 69% of impairment and 16% of uncontrolled hypertension in 2015 (Misganaw A et al., 2017).
52.7 % of hypertensive patients accompanied by uncontrolled hypertension at Jima Specialist Hospital. Understanding the incidence of uncontrolled hypertension and its related factors used to minimize mortality and disability due to uncontrolled hypertension (Bekele Tesfaye et al., 2017). Hypertension is a global health problem. According to WHO, 2019 Study Worldwide, 1.13 billion people have hypertension, two thirds live in low-and middle-income countries, and four in five hypertensive patients have uncontrolled hypertension (WHO, 2019). In another study, about one third of US adults or 86 million people had hypertension of this 35.8 million had uncontrolled hypertension (Somnath pal, 2018).
Uncontrolled hypertension is a risk of cardiovascular disease and stroke. This results in 24% of myocardial contravention of 23% of pulmonary edema, 16 per cent of hypertensive encephalopathy and 12 per cent of congestive heart failure (Somnath pal, 2018). According to the WHO 2017 survey, blood pressure is also rising the mortality rate due to cardiovascular disease. If blood pressure above 155/95 mm Hg, which results in a risk of death from heart failure, increases four times if usual, eight times as usual at 175/105 and 16 times as normal at 195/115 (WHO, 2017a).
According to the WHO 2017 survey, the prevalence of uncontrolled hypertension in high-income countries is lower. However, the burden of uncontrolled hypertension rises in low-and middle-income countries such as sub-Saharan Africa, South Asia and Central and Eastern Europe (WHO, 2017b). In low and middle-income countries, the health system is not well prepared to provide care for non-communicable diseases (NCDs) such as hypertension and hypertension control awareness, and the need for continuous treatment is small (WHO, 2017c).
Uncontrolled hypertension was the leading risk factor for death and the third cause of disability in low-and middle-income countries. The study found that low levels of diagnosis and hypertension management were achieved in rural areas of low to middle-income countries, primarily due to difficulties in accessing healthcare, costs in accessing health centers, distance to clinics, and the disparity in standard of care given had an effect on hypertension control (C. K. Chow et al., 2013). Sedentary lifestyle and missing appointments were associated with uncontrolled hypertension among follow-up hypertensive patients in Thailand (Suprawee Meelab et al.,2019
In Africa, the prevalence of uncontrolled hypertension varies across the country. Studies in Ghana have shown that 57.4% of patients with hypertensive follow-up have uncontrolled hypertension (Sarfo FS et al., 2018). Of the 922 hypertensive patients in Morocco, 675 (73%) had uncontrolled hypertension (Touria Essayagh et al . , 2019) and another study in South Africa found that 75.5 per cent of hypertensive patients had uncontrolled hypertension (Oladele Vincent Adeniyi et al . , 2016).
In Ethiopia, few studies have been performed on the prevalence of uncontrolled hypertension and associated factors among hypertensive patients, and prevalence also varies in different countries. According to WHO, the 2019 hypertension management study is still a concern in Ethiopia, with only 1 in 67 hypertensive adult patients having controlled hypertension (Fassil shiferaw, 2019). In other research performed in Ethiopia, the prevalence of uncontrolled hypertension ranged from 52.5% to 69.9% in Ayder Comprehensive Specialized Hospital and Zewditu Memorial Hospital, respectively.
Overweight, physical inactivity and comorbidity were found to be associated with uncontrolled hypertension (Gebrewahd Bezabh Gebremichael et al . , 2018, Yazie D et al . , 2018). Annual mean hypertension cost in Ethiopia was ETB 2510.32 ($91.72) ± 2152.80 (78.65) per patient. The direct medical costs are 60.81%, the direct non-medical costs 12.17% and the indirect costs 27.02% (Elsabet Adane et al . , 2018). In another West Showa report , the average annual cost of hypertension disease among follow-up patients was US$ 267.2 per patient. As a result, the annual average direct and indirect costs were US$ 136.6 and US$ 130.7 per patient, respectively (Addisu Bogale et al., 2019).
Managing hypertension eliminates problems due to uncontrolled hypertension. However, more than half of hypertensive patients in Ethiopia have uncontrolled hypertension (Yazie D et al . , 2018). There are limited studies that have been performed on uncontrolled hypertension in the study area. The goal of this study was therefore to assess the prevalence of uncontrolled hypertension and its associated factors among hypertensive patients undergoing follow-up in Bale Zone Hospitals, South East Ethiopia.
Hypertensive patient on follow up: - hypertensive patient on hypertension medication for at least for 1 month.
Physically active: an individual who perform physical exercise for at least 30 minutes per day for at least 5 day per week(WHO, 2014).
Physically inactive: an individual who perform physical exercise for less than 30 minutes per day for less than 5 day per week(WHO, 2014).
Methods and Materials
Study area and period
Study was conducted in five public hospitals of Bale zone namely Madda Walabu University Goba Referral, Robe General, Ginnir General, Delomena General and Madda Walabu District Hospitals. Bale Zone is found in Oromia region, 430KM far from the capital city of Ethiopia Addis Ababa. The Zone has an Eighty-Nine health Center and five public hospitals serving 1,955,198 communities. Many of these hospitals offered care to hypertensive patients in their follow-up clinic (Bale Zone Health Office, 2020). The study was conducted from March 2020 to April 2020.
Study Design and Population
A facility-based cross - sectional study design was conducted. The source population was all hypertension patients in the Bale zone hospitals. The study population was all randomly chosen adult hypertensive patients who attended follow-up in Bale Zone Hospitals in the study area. All adult hypertensive patients (> 18 years of age) on follow-up in the Bale zone hospitals and on antihypertensive drug therapy for at least 1 month were included. Patients who were extremely ill and unable to respond to the interview were excluded.
Sample size determination
Single population proportion formula was used to determine the sample size using proportion of 52.7% from previous study done 2017 in Jima University teaching and specialized hospital on uncontrolled hypertension and associated factors among adult hypertensive patients on follow-up (Bekele Tesfaye et al., 2017) at 95% confidence interval and 5% margin of error and adding 10% non-response rate the total sample size was 421 hypertensive patients on follow-up.
Sampling procedure
According to a study from five public hospitals in the Bale region, the hypertensive patient on follow-up in February 2020 was 902. Among these are Madda Walabu University Goba Referral Hospital 197 patients, Robe General Hospital 303 patients, Ginnir General Hospital 182 patients, Delomena General 131 patients and Madda Walabu District 89 hypertensive patients (Report of Five Bale Region Hospitals, 2020). Systematic random sampling was used to pick 421 participants. The first samples of the study were distributed proportionally to the hospitals on the basis of the patient flow data of the 1-month report.
Then, 421 study participants were picked 92 were from Madda Walabu University Goba Referral Hospital, 141 from Robe General Hospital, 85 from Ginnir General Hospital, 61 from Delomena General and 42 follow-up hypertensive patients from Madda Walabu District Hospital. The subjects of the analysis were chosen using a systematic random sampling method using the K=2 interval. Data were obtained by passing on each other to follow-up patients by considering the order in which they should be taken care of as a sampling frame after the first participant was selected by simple random sampling.
Study Variable
The Dependent variable for the study was uncontrolled Hypertension. And the independent variable were socio-demographic factors (age, sex, marital status, residence, religion, ethnicity, level of education, occupation and monthly income), personal factors (life style/ alcohol use, type and duration of Exercise, chewing chat, diet (fat use ,fruit and vegetables use and salt use) and BMI/ weight control/), disease and medication factors (comorbidities, duration of hypertension diagnosis, family history of hypertension, nature / type of ant hypertensive medication and duration of anti – hypertensive medication intake) and social factors (support from families and non-family members of the society).
Data collection tools
Data were collected from five qualified BSc Nurse patients on a face-to - face follow-up with a pre-tested semi-structured questionnaire (Bekele Tesfaye et al., 2017). The questionnaire was prepared in English and translated into Afan Oromo and Amharic and then translated back into English by language experts to verify its accuracy. The questionnaires contain:-socio-demographic, personal and social variables obtained by face-to - face interview and the medical record analysis was carried out using the data extraction method to be done for each research participant in order to obtain the comorbidities and the type / name of antihypertensive drugs. Blood Pressure was calculated using the standard Mercury Sphygmomanometer and stethoscope by trained data collectors, weight was measured using weighing scale by data collectors with patients standing without shoes and wearing light clothing and registered to the nearest 100 g. Height was also determined by the data collectors using the height scale, while the patients standing without shoes reported at the nearest 0.5 cm and finally the Body-Mass Index (BMI) were calculated.
Data collection Procedures
Before the actual data collection preparation was given for one day by the main investigator. Training sessions was on the objective of the study, the purpose of each question and interviewing methods, and the role of the data collector in the training. Pretest was performed on 5% of the overall sample size in the Dodola General Hospital. Then five BSC Nurse performed face-to - face interviews for socio-demographic, personal and social reasons. Comorbidities and antihypertensive drugs were obtained from medical records and blood pressure was measured twice using the regular Mercury Sphygmomanometer and stethoscope after rest for 30 minutes and an average of two measurements were used to monitor or manage hypertension. Height and weight were determined when the BMI was calculated.
Data quality control
In order to ensure the accuracy of the data , data collectors have been trained for one day on data collection procedures. Pretest was performed on 5 percent of the overall sample size in the Dodola General Hospital. Based on feedback from the pre-test, the required modifications have been made. The main investigator was monitored and checked to ensure the completeness and consistency of the data obtained. Blood pressure was measured using a pre-tested Mercury Sphygmomanometer (adult size) and a stethoscope while the patient is sitting from the left arm after the patient rests at least 30 minutes before the measurement. The study subjects' weight was measured with subjects standing without shoes and wearing light clothing, reported to the nearest 100 g and calibration was performed after each measurement. Height was also assessed with patients standing without shoes and wearing light cloths.
Data processing and analysis
The data collected was entered in Epi data version 3.1 and exported to SPSS version 25 for review. Descriptive statistics, including frequency , percentage , mean and standard deviation, were used to summarize study variables. Binary logistic regression was calculated to evaluate associations between independent variables and uncontrolled hypertension using the crude odds ratio (COR) and the modified odds ratio (AOR) at the 95 % confidence stage. Variables with p-values of less than 0.2 in bivariate logistic regression were applied to multivariate logistic regression and p-values of less than 0.05 were considered statistically significant.
The collected data were entered into Epi data version 3.1 and then exported to SPSS version 25 for analysis. Descriptive statistics including Frequencies, percentage, mean and standard deviation were used to summarize study variables. Binary logistic regression was computed to analyze the associations between independent variables and uncontrolled hypertension by using crude odds ratio (COR) and adjusted odds ratio (AOR) at 95% confidence level. Variables with p-values less than 0.2 in the bivariate logistic regression were fitted in the multivariable logistic regression and p-value of less than 0.05 was considered statistically significant. The findings of this study were presented by using tables, figures and texts.
Ethical consideration
Ethical clearance was obtained from Madda Walabu University Goba Referral Ethical Hospital; Study Review Committee. Permission letter has been written from Madda Walabu University Goba Referral Hospital Academic Office to Madda Walabu University Goba Referral Hospital, Robe General Hospital, Ginnir General Hospital, Dello Mana General Hospital and Madda Walabu District Hospital. Of hospital was given prior to the start of the actual data collection and subsequent authorisation. Verbal informed consent was obtained from each study participant. The name and other personal identifiers of the participants were not included in the questionnaires and the right of the participants to withdraw from the study at any time during the data collection was preserved without violation of any benefit that the research participant obtained from the hospital. All information received from the study participant has been kept confidential. However, patients with uncontrolled hypertension were told to physicians and nurses working in a follow-up clinic, and the appropriate care was given on a case-by - case basis.
Results
Overall, 421 participants were included in this study with a response rate of 412 (97.8%). Of the 412 participants in the sample, 228 (55.3%) were male. The average age of respondents was 53.8 ±11.9 SD years and almost half (49.5%) were between 45-59 years of age, the majority were 383 (93%) were married and 257 (62.4%) were urban. More than half (52.9%) of participants were Muslims and 145 (35.2%) did not learn formal education as shown in (Table 1).
Prevalence of Uncontrolled Hypertension
The mean systolic blood pressure was 140.57±16.75 mmHg SD and the mean diastolic blood pressure was 88.61±13.04 mm Hg SD. Overall, 235(57.04%) (95% CI, 52.3–61.8%) of the study participants had uncontrolled hypertension and the remaining 177(42.96%) had controlled hypertension (Figure 1).
Personal or Life Style Related Factors
Among participants, 149 (36.2%) added salt to their diet and 282 (68.4%) did not eat fatty food and 184 (44.7%) of participants ate fruit and vegetables 1-3 days a week and 252 (61.2%) hypertensive patients were physically inactive. The majority of participants 374 (90.8%) were not consuming alcohol and 404 (98.1%) were not smoking cigarettes, 246 (59.7%) were in the usual BMI range (Table 3)
Disease related factors and support for care
Of all the participants in the study, 81(19.7%) patients had co-morbid conditions compared to 42 (51.85%) patients with Diabetes mellitus. One hundred and thirty two (32%) of participants were diagnosed with hypertension in the last two years. The duration of hypertension diagnosis ranged from 1 month to 20 years. Three hundred five (74 %) had family or other care assistance as seen in )Table 4).
Factors associated with uncontrolled hypertension
The association of independent variables with the uncontrolled hypertension was investigated using both binary and multivariate logistic regression. In bivariate logistic regression analysis; eleven variables were p value 0.2. Age 60-74 years (COR= 3.941, 95% CI: 1.205-12.896, P=0.023) when compared to age 75-89 years, patients those have family history of hypertension (COR=1.512, 95% CI: 1.020-2.242, P=0.04) as compared to those did not have, experience of medications side effect (COR=0.521, 95% CI: 0.323-.842, p=0.008), blood pressure measurement weekly (COR=0.064(0.006-0.639, p=0.019) as compared to those measure every two month, Medication use before one day of blood pressure measurement (COR=0.505, 95% CI: 0.291-0.875, p=0.015), support for care (COR=2.53, 95% CI: 1.566-4.105, p<0.001) as compared to counterpart.
The association of independent variables with uncontrolled hypertension was investigated by binary and multivariate logistic regression. In bivariate logistic regression analysis, eleven variables had a p value of 0.2. 60-74 years of age (COR=3.941, 95% CI: 1.205-12.896, P=0.023) compared to 75-89 years of age, patients with family history of hypertension (COR=1.512, 95% CI: 1.020-2.242, P=0.04) compared to those who did not have experience of side-effect medication (COR=0.521, 95% CI: 0.323-.842, p=0.008), weekly blood pressure measurement (COR=0.064(0.006-0.639, p=0.019) as a compared to those measure every two month, medication use before one day of blood pressure.
Salt use (COR=0.391, 95% CI: 0.254-0.6, p<0.001), not consuming fatty food was negatively associated with uncontrolled hypertension (COR=3.920, 95% CI: 2.375-6.469, p<0.001) compared to those consuming fat for 1-3 days / week, not consuming fruit and vegetables was less likely to increase uncontrolled hypertension (COR=0.127, 95% CI: 0.030-0.548, p=0.006) and always consumed (COR=5). Physical inactivity (COR=0.302, 95 % CI: 0.2-0.457, p<0.001) relative to regular physical activity. And also comorbidities (COR= 0.490, 95% CI: 0.29-0.827, p=0.008) were showed association with uncontrolled hypertension and all this variables were fitted in multivariate logistics regression as shown in (Table 5).
Multivariate logistics regression analysis for uncontrolled hypertension
Multivariate logistic regression analysis showed that patients with drug side effects encountered twice (AOR=1.975, 95 % CI: 1.056-3.695, P=0.033) were more likely to have uncontrolled hypertension than those with no drug side effects. The two-fold risk of uncontrolled hypertension (AOR=1.988, 95% CI, 1.026-3.85, P=0.042) in hypertensive patients with comorbidity compared to patients without comorbidity. Hypertensive patients with relatives or other care support 52% (AOR=0.485, 95% CI: 0.266-0.886, p=0.019) less likely to have uncontrolled hypertension compared to their counterparts.
Potential for uncontrolled hypertension was two times higher (AOR=1.914, 95 % CI: 1.106-3.313, P=0.02) in hypertensive patients who added salt to their food compared to those who did not use salt. Hypertensive patients who did not consume fruit and vegetables were six times more likely to have uncontrolled hypertension (AOR=6,106, 95% CI: 1,261-29,569, p=0,025) than those who ate fruit and vegetables for 1-3 days per week. Similarly , patients who used fruit and vegetables all weekdays were 68% (AOR=0.323, 95% CI: 0.186-0.561, P=0.001) less likely to experience uncontrolled hypertension compared to patients who used fruit and vegetables for 1-3 days / week. Hypertensive patients who did not consume fat 75% (AOR=0.249, 95% CI: 0.135-0.459, P<0.001) were less likely to experience uncontrolled hypertension relative to those who used fat for 1–3 days / week. Patients who were physically inactive twice (AOR=1.972, 95 % CI: 1.185-3.282, p=0.009) were more likely to have uncontrolled hypertension relative to those who conducted regular physical activity as shown in (Table 6).
Discussion
This study showed that 57% (95% CI: 51.3-61.8%) of adult hypertensive patients had uncontrolled hypertension. This finding is almost consistent with studies in Tikur Anbessa General Specialized Hospital, which was 59.9% of hypertensive patients following uncontrolled hypertension (Adamu Tesfaye et al., 2015), 56.4% in Adama (Gete Chemeda Lichisa et al., 2014), 57.4% of hypertensive patients with uncontrolled hypertension (Sarfo FS et al . , 2018) and 53.6% in Ghana.
This result is lower than study done in Zewditu memorial hospital 69.9%(Yazie D et al., 2018), hospital based studies conducted in Zimbabwe 67.2 % (Tafadzwa Priscilla Goverwa et al., 2014) and Kenya 66.6% (Mutua E. et al., 2014). This difference could be because of discrepancies lifestyle behaviors such as feeding habits and sedentary lifestyles that increase uncontrolled hypertension and the other justification is the study done in Zewditu memorial hospital, Zimbabwe and Kenya. Classification of uncontrolled blood pressure ≥140/90 and blood pressure ≥130/80 for general hypertensive patients and for comorbid cases of chronic kidney disease and diabetes mellitus, as recommended by the Joint National Committee 7 for the Control of Blood Pressure. However, this study was conducted using Joined National Committee 8 for the management of uncontrolled hypertension of systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg for individuals below 60 years of age and systolic blood pressure ≥ 150 mmHg and diastolic blood pressure ≥ 90 mmHg with daily use of anti-hypertensive medication(s) for individuals below 60 years of age and above (Paul A. James et al.,2014). The results of this study are higher than those of the University of Gondar Reference Hospital, Ethiopia 49.6% (Animut Y et al., 2018), Southwest Ethiopia 49.7% (Asgedom SW et al . , 2016) and Malaysia 50.7% of the follow-up hypertensive patients (Cheong A et al., 2015). This discrepancy is due to the difference in population.
In this study, experience with drug side effects substantially associated with uncontrolled hypertension; experience with drug side effects was two times more likely to have uncontrolled hypertension than experience with non-medication side effects. This result is consistent with the Chicago study (Yacob G. Tedla and Bautista, 2015). This is due to the fact that hypertensive patients who experience side-effect medications decrease care and also lower adherence to drugs (Kronish IM et al . , 2011). Hypertensive patients with family or other care support were 52% less likely to experience uncontrolled hypertension compared to their counterparts. This result is consistent with studies conducted in Nigeria (Oluwaseun S. Ojo1 et al., 2017) and the USA (Flynn SJ et al., 2013). This could be due to decreased family support or other personal support that may lead to unhealthy habits impacting a healthier lifestyle. A healthy social network can also reduce blood pressure by reducing stress (Flynn SJ et al., 2013).
In this study , patients with comorbidities are twice as likely to have uncontrolled hypertension. This finding is similar to a study in Thailand (Boonsub Sakboonyarat et al., 2019). This indicates that it is difficult to control blood pressure in patients with comorbidities. Patients who have applied salt to their diet are two times more likely to have uncontrolled hypertension than those who have not used salt. The results are consistent with the findings of studies conducted at the Jimma University Specialized Hospital (Solomon Woldegebriel Asgedom et al . , 2016) and in China (Li Yang et al . , 2014). This is due to the effect of salt on the body's sodium balance, which induces fluid retention that improves preservation. This is due to the effect of salt on the body's sodium balance, which causes fluid retention that increases blood pressure on the walls of the blood vessels (Whelton PK et al . , 2018).
Patients that did not consume fat 75% less often decreased the risk of uncontrolled hypertension compared to those who consumed fat for 1-3 days per week. This is similar to the study in Ghana (Sarfo FS et al . , 2018). This could be due to the fact that excess accumulation of fat in the blood vessels leads to atherosclerosis and also saturated fat obtained commonly found from animals, is the risk of cardiovascular disorders (Sabour H et al . , 2016).
This study found that patients who did not have any physical activity were twice as likely to have uncontrolled hypertension compared to patients who did regular physical activity. This finding is supported by studies conducted at the Jimma University Specialized Hospital (Solomon Woldegebriel Asgedom et al . , 2016), studies conducted at the Tikur Anbess General Specialized Hospital (Adamu Tesfaye et al . , 2015) and studies conducted in China (Li Yang et al., 2014). This may be due to regular physical activity that makes the heart stronger and can pump more blood with less effort. If the heart works less to pump, the strength of the arteries decreases, lowering blood pressure. Exercise also has an effect on the reduction of systemic vascular resistance, plasma norepinephrine and renin activity (Diaz KM and D., 2013)
Patients who did not eat fruit and vegetables were six times more likely to have uncontrolled hypertension than those who ate fruit and vegetables for 1-3 days per week. Similarly , patients who ate vegetables for all days of the week were 68% less likely to have uncontrolled hypertension compared to those who consumed fruit and vegetables for 1-3 days a week. This finding is consistent with studies in Spain (Pienovi L et al., 2015) and China (Li G et al., 2015). Fruit and vegetables are low in cholesterol and saturated fat and high in dietary fiber, potassium , calcium and magnesium, which lowers blood pressure (Whelton PK).
Conclussion
The prevalence of uncontrolled hypertension was high and more than half of the adult hypertensive follow-up patients had uncontrolled hypertension in five public hospitals in the Bale zone. Experience with side-effect treatment, salt use, not eating fruit and vegetables, physical inactivity and comorbidity were factors positively associated with uncontrolled hypertension while family or other caregivers and non-consumers of fat were negatively associated with uncontrolled hypertension. Education on substance usage, lifestyle modification and ongoing follow-up is therefore crucial to control hypertension in patients with uncontrolled hypertension.
Limitation of the study
The research was performed in hypertensive patients who attended follow-up at Hospitals and did not recognize hypertensive patients who did not follow-up. This limits the generalizability of the results to the whole population. Since this research was a cross-sectional study design, the essence of the analysis could be difficult to establish the causal relationship between the study variables. The results of this study were based on self-reported knowledge that did not reflect their actual experience in hypertension management.
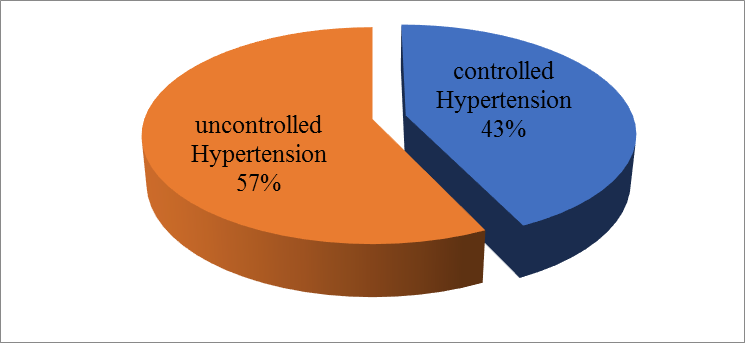
Figure 1: Hypertension status of adult hypertensive patients on follow up in Bale Zone Hospitals, Southeast Ethiopia, 2020 (n=412)
List of tables
|
Variables |
Category |
Frequency |
Percent |
|
Age |
<30 years 30-44 years 45-59 years 60-74 years 75-89 years |
6 81 204 104 17 |
1.5 19.7 49.5 25.2 4.1 |
|
Sex |
Male Female |
228 184 |
55.3 44.7 |
|
Marital status |
Single Married Separate/divorced Widowed |
6 383 5 18 |
1.4 93.0 1.2 4.4 |
|
Place of Residence |
Urban Rural |
257 155 |
62.4 37.6 |
|
Religion |
Muslim Orthodox Protestant Wakefata |
218 169 19 6 |
52.9 41.0 4.6 1.5 |
|
Ethnicity |
Oromo Amhara Tigre Gurage |
284 102 18 8 |
68.9 24.8 4.4 1.9 |
|
Educational status |
Unable to read and Write Read and Write Primary School Secondary School Diploma/Level IV Frist degree and above |
145 58 87 58 50 14 |
35.2 14.1 21.1 14.1 12.1 3.4 |
|
Occupation |
House Wife Farmer Government employee |
124 98 48 |
30.1 23.8 11.7 |
|
|
Merchant Self employed Non employed Others |
74 53 3 12 |
18.0 12.9 0.7 2.9 |
|
Monthly income |
1500-3500 3501-5500 5501-10000 10000-20000 >=20000 |
81 99 141 64 27 |
19.7 24.0 34.2 15.5 6.6 |
Table 1: Socio demographic characteristics of adult hypertensive patients on follow up in Bale Zone Hospitals, Southeast Ethiopia, 2020 (n=412)
|
Variables Category |
Frequency |
Percent |
|
|
Duration of management
|
<2 years 2-5 years 5-10 years >10 years |
132 120 115 45 |
32.0 29.1 28.0 10.9 |
|
Experienced medication side effects |
Yes No |
99 313 |
24.0 76.0 |
|
Types medication of side effect (n=99)
|
Erectile dysfunction Headache Weakness Dry mouth |
13 54 31 1 |
13.13 54.54 31.31 1.01 |
|
Is there any days when you did not take your medicine? |
Yes No |
98 314 |
23.8 76.2 |
|
Reason for not using anti hypertension medicine(n=98)
|
I forgot Due to fear of side effect Symptoms of high blood pressure controlled I take traditional drug |
85 6 5 2 |
86.73 6.12 5.11 2.04 |
|
Medication use one day before Blood pressure measured |
Yes No |
351 61 |
85.2 14.8 |
|
Frequency of Blood pressure measured
|
Weekly Every two week Monthly Every two month |
49 12 346 5 |
11.9 2.9 84.0 1.2 |
|
Current Antihypertensive patients use
|
Mono therapy Two drug therapy Three drug therapy |
122 280 10 |
29.6 68.0 2.4 |
|
Name of drugs patient use
|
Hydrochlorothiazide Nevidipine + Hydrochlorothiazide ACHI + Hydrochlorothiazide Beta blocker + Hydrochlorothiazide Amlodipine + Hydrochlorothiazide ACHI + Amlodipine + Hydrochlorothiazide |
122 27 153 4 96 10 |
29.6 6.6 37.1 1.0 23.3 2.4 |
Table 2: Medication factors of adult hypertensive patients on follow up in Bale Zone Hospitals, Southeast Ethiopia, 2020 (n=412)
|
Variable category |
Frequency |
Percent |
||
|
Drinking alcohol
|
Yes No |
38 374 |
9.2 90.8 |
|
|
Use of salt in food
|
Yes No |
149 263 |
36.2 63.8 |
|
|
Consuming fruit or vegetables
|
not eat fruit and vegetables always 4-6 days/week 1-3 days/week |
37 144 47 184 |
9.0 35.0 11.4 44.7 |
|
|
Consuming fat
|
not eat fat always 4-6 days/week 1-3 days/week |
282 3 12 115 |
68.4 0.7 2.9 27.9 |
|
|
Smoking cigarettes
|
Yes No |
8 404 |
1.9 98.1 |
|
|
Chewing chat
|
Yes No |
46 366 |
11.2 88.8 |
|
|
Regular physical activity
|
Yes No |
307 105 |
74.51 25.49 |
|
|
Duration of regular physical exercise per day(n=307)
|
walking for less than 30 minutes walking for more than 30 minutes Any types of walking without classification Go to work place on foot |
147 95 63 2 |
47.88 30.94 20.52 0.65 |
|
|
Physical activity
|
Physically inactive Physically active |
252 160 |
61.2 38.8 |
|
|
BMI
|
Underweight (<18.5 kg/m2) |
1 |
0.2 |
|
|
Normal (18.5-24.9 kg/m2) |
246 |
59.7 |
||
|
Over weight (25-29.9 kg/m2) |
156 |
37.9 |
||
Table 3: Personal or Life style related factors of adult hypertensive patients on follow up in Bale Zone Hospitals, Southeast Ethiopia, 2020 (n=412)
|
Variable category |
Frequency |
Percent |
||
|
Comorbidities
|
Yes No |
81 331 |
19.7 80.3 |
|
|
Types of comorbidities(n=81)
|
Chronic Kidney diseases (CKD) Diabetes mellitus (DM) Heart failure Gouty arthritis Both CKD and DM |
18 42 13 2 6 |
22.22 51.85 16.04 2.4 7.4 |
|
|
Duration of hypertension diagnosis
|
<2 years 2-5 years 5-10 years >10 years |
132 120 115 45 |
32.0 29.1 28.0 10.9 |
|
|
Family history of hypertension |
Yes No |
218 194 |
52.9 47.1 |
|
|
Family/other person support for care |
Yes No |
305 107 |
74 26 |
|
Table 4: Disease related factors and support for care of adult hypertensive patients on follow up in Bale Zone Hospitals, Southeast Ethiopia, 2020 (n=412)
|
Variables |
Category |
Hypertension status |
COR (95% CI) |
P value |
|
|
Uncontrolled n(%) |
Controlled n(%) |
||||
|
Age |
<30 years 30-44years 45-59 years 60-74 years 75-89 years |
2(33.3) 46(56.8) 127(62.3) 47(45.2) 13(76.5) |
4(66.7) 35(43.2) 77(37.7) 57(54.8) 4(23.5) |
6.5(0.85-49.687) 2.473(0.742-8.241) 1.97(0.62-6.26) 3.941(1.205-12.89)* 1 |
0.071 0.140 0.250 0.023
|
|
Family history of hypertension |
Yes No |
114(52.3) 121(62.4) |
104(47.7) 73(37.6) |
1.512(1.020-2.242)* 1 |
0.04
|
|
Experienced side effects of medications |
Yes No |
68(68.7) 167(53.4) |
31(31.3) 146(46.6) |
0.521 (.323-.842)* 1 |
0.008 |
|
Medication use before one days of blood pressure measured |
Yes No |
209(59.5) 26(42.6) |
142(40.5) 35(57.4) |
0.505(0.291-0.875)* 1 |
0.015 |
|
Blood pressure measurement |
Weekly every 2 week monthly every 2 month |
39(79.6) 7(58.3) 188(54.3) 1(20) |
10(20.4) 5(41.7) 158(45.7) 4(80) |
0.064(0.006-0.639)* 0.179(0.015- 2.119) 0.210(0.023- 1.899) 1 |
0.019 0.172 0.165 |
|
Use of salt in food |
Yes No |
106(71) 129(49) |
43(29) 134(51) |
0.391(.254-0.6) 1 |
<0.001 |
|
Consuming fruit or vegetables |
not consumed always 4-6 days/week 1-3 days/week |
35(94.6) 44(30.6) 29(61.7) 127(69) |
2(5.4) 100(69.4) 18(38.3) 57(31) |
0.127(.030-0.548)* 5.064(3.157-8.123)* 1.383(0.711- 2.692) 1 |
0.006 <0.001 0.340 |
|
Consuming Fat |
not consume always 4-6 days/week 1-3 days/week |
135(47.9) 3(100) 7(58.3) 90(78.3) |
147(52.1) 0 5(41.7) 25(21.7) |
3.92(2.375-6.469)*
2.571(0.751-8.799) 1 |
<0.001 <0.001 0.132 |
|
physical activity |
Inactive Active |
172(68.3) 63(39.4) |
80(31.7) 97(60.6) |
0.302(0.2-0.457)* 1 |
<0.001
|
|
Having support for care |
Yes No |
157(51.5) 78(72.9) |
148(48.5) 29(27.1) |
2.535(1.566-4.105)* 1 |
<0.001 |
|
Comorbidities |
Yes No |
57(70.4) 178(53.8) |
24(29.6) 153(46.2) |
0.490(0.29-0.827)* 1 |
0.008 |
Table 5: Bivariate logistic regression of adult hypertensive patients on follow up in Bale Zone Hospitals, Southeast Ethiopia, 2020 (n=412)
|
Variables
|
Category |
Hypertension status |
COR (95% CI) |
AOR (95% CI) |
P value |
|
|
Uncontrolled n (%) |
Controlled n(%) |
|||||
|
Age |
<30 years 30-44years 45-59 years 60-74 years 75-89 years |
2(33.3) 46(56.8) 127(62.3) 47(45.2) 13(76.5) |
4(66.7) 35(43.2) 77(37.7) 57(54.8) 4(23.5) |
6.5(0.85-49.687) 2.473(0.742-8.241) 1.97(0.62-6.26) 3.941(1.205-12.89) 1 |
0.219(0.016-2.975) 0.649(0.15-2.813) 0.756(0.185-3.083) 0.384(0.091-1.62) 1 |
0.254 0.564 0.697 0.193 |
|
Family history of hypertension |
Yes No |
114(52.3) 121(62.4) |
104(47.7)73(37.6) |
1.512(1.020-2.242) 1 |
0.771(0.466-1.277) |
.312 |
|
Experienced side effects of medications |
Yes No |
68(68.7) 167(53.4) |
31(31.3) 146(46.6) |
0.521 (.323-.842) 1 |
1.975(1.056-3.695) 1 |
0.033 |
|
Medication use before one days of blood pressure measured |
Yes No |
209(59.5) 26(42.6) |
142(40.5)35(57.4) |
0.505(0.291-0.875) 1 |
2.083(1.048-4.141) 1 |
0.036 |
|
Blood pressure measurement |
Weekly every 2 week monthly every 2 month |
39(79.6) 7(58.3) 188(54.3) 1(20) |
10(20.4) 5(41.7) 158(45.7) 4(80) |
0.064(0.006-0.639)
1 |
5.632(0.39-81.298) 2.253(0.122-41.288) 3.546(0.283-44.431) 1 |
0.204 0.585 0.326 |
|
Use of salt in food |
Yes No |
106(71) 129(49) |
43(29) 134(51) |
0.391(.254-0.6) 1 |
1.914(1.106-3.313) 1 |
0.020 |
|
Consuming fruit or vegetables |
not consumed always 4-6 days/week 1-3 days/week |
35(94.6) 44(30.6) 29(61.7) 127(69) |
2(5.4) 100(69.4) 18(38.3) 57(31) |
0.127(.030-0.548) 5.064(3.157-8.123)
1 |
6.106(1.261-29.569) 0.323(0.186-0.561) 0.898(0.415-1.943) 1 |
0.025 0.001 0.786 |
|
Consuming Fat |
not consume always 4-6 days/week 1-3 days/week |
135(47.9) 3(100) 7(58.3) 90(78.3) |
147(52.1) 0 5(41.7) 25(21.7) |
3.92(2.375-6.469)
1 |
0.249(0.135-0.459)
0.794(0.175-3.598) 1 |
<0.001
0.765 |
|
physical activity |
Inactive Active |
172(68.3) 63(39.4) |
80(31.7) 97(60.6) |
0.302(0.2-0.457) 1 |
1.972(1.185-3.282) 1 |
0.009 |
|
Support for care |
Yes No |
157(51.5) 78(72.9) |
148(48.5) 29(27.1) |
2.535(1.566-4.105) 1 |
0.485(0.266-0.886) 1 |
0.019 |
|
Comorbidities |
Yes No |
57(70.4) 178(53.8) |
24(29.6) 153(46.2) |
0.490(0.29-0.827) 1 |
1.988(1.026-3.85) 1 |
0.042 |
Table 6: Multivariate logistics regression of adult hypertensive patients on follow up in Bale Zone Hospitals, Southeast Ethiopia, 2020 (n=412)
|
AOR |
Adjusted Odd Ratio |
|
BMI |
Body Mass Index |
|
CI |
Confidence Interval |
|
CKD |
Chronic Kidney Diseases |
|
COR |
Crude Odd Ratio |
|
DM |
Diabetes Mellitus |
|
FMOH |
Federal Ministry of Health |
|
JNC |
Joint National Committee |
|
MWU |
Madda Walabu University |
|
NCDs |
Non Communicable Diseases |
|
SD |
Standard Deviation |
|
SPSS |
Statistical Package for Social Sciences |
|
SSA |
Sub-Sahara Africa |
|
WHO |
World Health Organization |
Ethical considerations
Ethical clearance was obtained from Madda Walabu University Goba Referral Ethical Hospital; Study Review Committee. Permission letter has been written from Madda Walabu University Goba Referral Hospital Academic Office to Madda Walabu University Goba Referral Hospital, Robe General Hospital, Ginnir General Hospital, Dello Mana General Hospital and Madda Walabu District Hospital. Of hospital was given prior to the start of the actual data collection and subsequent authorisation. Verbal informed consent was obtained from each study participant. The name and other personal identifiers of the participants were not included in the questionnaires and the right of the participants to withdraw from the study at any time during the data collection was preserved without violation of any benefit that the research participant obtained from the hospital. All information received from the study participant has been kept confidential. However, patients with uncontrolled hypertension were told to physicians and nurses working in a follow-up clinic, and the appropriate care was given on a case-by - case basis.
Consent for publication
All the information used for this study was collected with the consent of participates of the study. And all the authors have read the manuscript and have consented to publish it this journal.
Data availability
The data for this study is available with the authors and can be accessed based on the request from the concerned body.
Funding
Funding agencies do not have role in the publication of the paper.
Competing interest
The authors declare that they do not have conflict of interest.
Authors’ contribution
Anwar Tahir have conceived and designed the study, performed the data analysis and write up of the final result. Abulie Takele participated in designing the study, performed the statistical analysis, writing the results and discussion and prepared the manuscript. And Geroma Morka participated in designing the study, performed the statistical analysis and writing the results
Acknowledgements
First of all, we would like to express our sincere gratitude to the study participants for their time and the information they provided. We would like to thank the data collectors, administrative bodies and health professionals of the five Bale Zone Public Hospitals for their help during data