Orthopaedic Research and Surgery
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2994-8738 | Journal DOI: 10.61148/2994-8738/JORS
Brent C. Reider* and Warwick A. J. Reider
Director, Relevium Labs, Inc., 4663 Katie Lane, Oxford, Ohio, 45056, USA. yarlap.com
*Corresponding Author: Brent C. Reider, Director, Relevium Labs, Inc., 4663 Katie Lane, Oxford, Ohio, 45056, USA.
Received date: March 15, 2021
Accepted date: March 27, 2021
Published date: March 30, 2021
Citation: Brent C. Reider and Warwick A. J. Reider. “Female Pelvic Floor Muscle Tone Role in Exercise Performance Protocol.’’. J Orthopaedic Research and Surgery, 2(1); DOI: http;//doi.org/03.2021/1.1009.
Copyright: © 2021 Luiz Cláudio Lacerda Rodrigues. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Staying active throughout life is important. Since the musculoskeletal system is interactive the activities one chooses to stay active can have wide-ranging effect. Repetitive impact during exercise can reduce tone in the muscles of the pelvic floor. Symptoms resulting from loss in pelvic floor muscle tone, like urinary incontinence and organ decent may reveal an individual’s predisposition(s) to pelvic floor muscle tone loss. Exercise and muscle reeducation programs to maintain pelvic floor muscle tone, are non-narcotic, non-surgical pathways to maintaining continence and addressing organ decent. Incorporating pelvic floor muscle tone in a woman’s exercise regimen can have broad positive outcomes; including treating female urinary incontinence, maintaining continence and indications suggest improved freedom of movement, improved intimacy, reduced lower back pain and improved performance of the lower extremities.
Introduction
General exercise training throughout life is important for health and wellbeing. Because the musculoskeletal structure is interactive, exercise protocols should include activities to improve pelvic floor muscle tone. Forces that are exerted on the pelvic floor can strengthen the pelvic floor, or overload, stretch and weaken the pelvic floor (Bø, 2004). Loss of pelvic floor muscle tone can cause urinary incontinence. A number of studies suggest female athletes may be as much as three times the risk of experiencing urinary incontinence as among the general population (Teixeira et al., 2018). While the risk of incontinence appears to be patient specific indications suggest repetitive impact and the intensity of a training program may trigger an individual’s predisposition to incontinence (de Mattos Lourenco et al., 2018). The authors believe there is evidence these indicative prompts exist and that the symptoms can appear, before, during and after the loss of tone in the female pelvic floor muscles.
Kegel exercise protocols are an effective non-narcotic, non-surgical way to improve muscle pelvic floor muscle tone, and to treat incontinence (Bø, 2004) and pelvic organ decent (Bø, 2006). For women who do not have the time, confidence or ability to performing pelvic floor exercises, electronic stimulation of the pelvic floor muscles electroceuticals, can restore and maintain pelvic floor muscle control. Electroceuticals, are capable of effectively reeducating the muscles of the female pelvic floor even when injury or atrophy are severe (e.g., AutoKegel). Visual cues and the ability of artificial intelligence to learn for patient specific gaming can stimulate patient motivation for increasingly effective therapies, including muscle re-education therapies for the pelvic floor (Reider, 2019; Reider, 2020).
Background
The muscles of the female pelvic floor are inside the pelvis and run along the floor of the abdominal cavity creating the pelvic and urogenital diaphragm. The primary function of the pelvic floor muscles, including the pubococcygeus muscle, is postural. The muscles of the pelvic floor keep the visceral organs in their natural position. The muscles of the pelvic floor working in concert with the skeleton; bones, ligaments, tendons and joints and the muscle of the lower back and thighs to move the weight of the body to the heals.
The musculoskeletal structure moves the weight of the upper body from the base of the spine through the pelvis in an arch to the heels. As a structural component the pointed Gothic arch (figure 1)
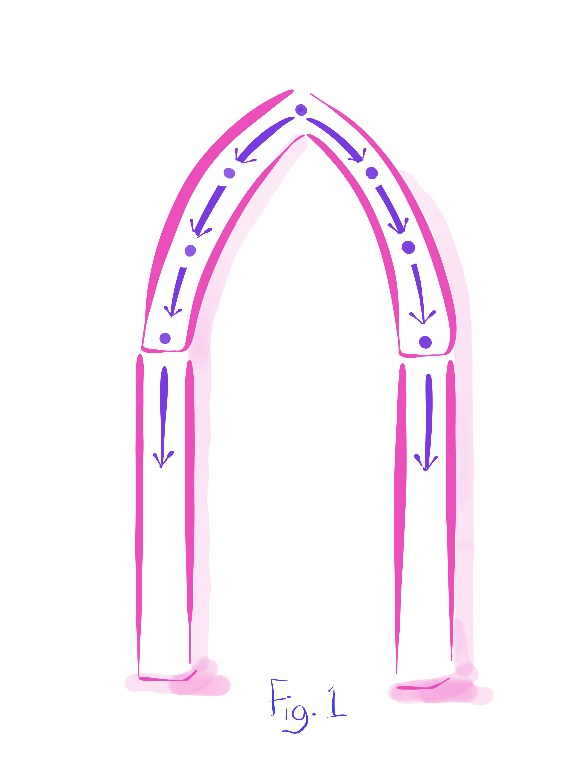
Is more efficient in this application than a semicircular arch (figure 2)
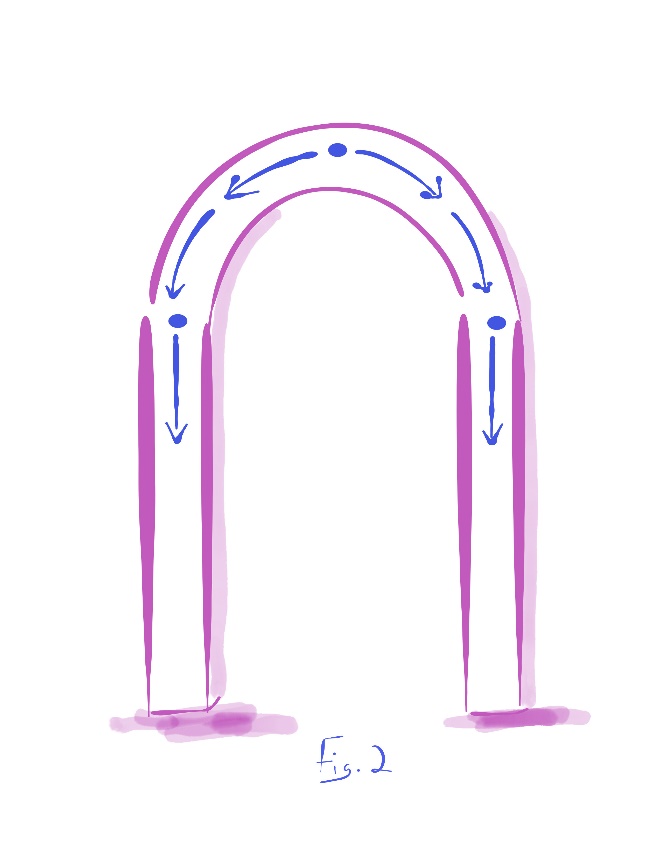
Because a Gothic arch transfers weight with a smaller horizontal component and a larger vertical component (Huber, 2009). In quantitative terms L in figure 3
Represents the load placed on the pelvic arch by the weight of the upper body. Alpha (α) represents the angle where the load transfers downward at both points in the arch (for simplification we assume musculoskeletal symmetry and omit tracery functions that would potentially exit for each individual) (Phillips, 1926) and H represents the horizontal component of the thrust that is generated outward. Since the outward thrust are concentrated where the arch converges with the horizontal supports, the thrust can be countered. In architecture, these forces can be countered using Flying buttresses (Figure 4).

Thrust is a force governed by Newton’s second and third laws of motion (Newton, 1687). When a system exerts a mass (load) in one direction, the accelerated mass will cause a proportional but opposite force (thrust) on that system. For the human body, the thrust (T) that the arch generates (figure 5)

Passes through the femoral neck where the load transfers downward to the heals (figure 6).

Given the location of the pelvic floor muscles inside the pelvis and their close connection to other muscle groups and their inclusion in the abdominal cavity, it is proven difficult to differentiate between opposing forces occurring during physical activity. Unquestionably, the muscle of the pelvic floor working with the muscles of the lower back and thighs aid in the skeletal alignment to effectively manage the load to the heals (Pel et al., 2006). Because the outward thrust is more easily contained in the configuration of a Gothic arch the weight of the body is more easily transmitted down through the skeleton with the muscles of the lower back, pelvis and thighs working in concert to transfer the body weight downward effectively. Assuming musculoskeletal symmetry and omitting tracery in the pelvic arch created by the musculoskeletal structed and visceral the horizontal and thrust is quantitatively:
H ≈ T ≈
T ≈ L2 tangent α
L2 tangent α
A simple change in load can have a significant increase in the outward forces.
If the load running down through the arch increases or the span of the arc increases, the vertical components must be able to bear the increased compression forces downward at the piers of the arch (i.e., legs). Mechanisms must be capable of managing the increasing outward thrust at the point of convergence (i.e., hips) or the arch will fail. Additional weight in the legs of the arch can help manage escalation in the increasing outward thrust. However, an increase in the transverse dimension of the pelvic Gothic arch results in a significant surge in the lines of force outward as well. Formulaically, figure 7

Demonstrates the problematic issue where d is the half the span of the arch and h is the height and H represents the horizontal component of the thrust that is generated at the point of convergence (Huber, 2009) – across the perineal area outward to the femoral neck:
H ≈ T ≈
T ≈ d1+d2h2
d1+d2h2
A simple change in the span of the arch can have a significant increase in the outward forces – thrust is inversely proportional to the rise-to-span ratio.
When the horizontal component of the outward thrust that is generated at the point of convergence (hips) is greater than the piers can manage, the arch begins to deflect (outward at the hip and inward at the knees). Deflection may occur for some time prior to the catastrophic failure of the arch. Repairs to the arch can be made to save the structure. At the Amiens Cathedral in France, chains were placed in strategic locations to counter the outward forces to prevent imminent structural failure indicated by cracks in the main arches of the church’s choir. The outward forces at the hip (H) push the top of the pier outward. When the top of the pier is thrust outward, the pier’s midpoint caves inward (K). Deflection at the point of collapse is represented in figure 8.

These load-distribution features counter outward forces that can cause structural failure represented in Figure 9;

Including joint pain and erosion (Pel et al., 2006). As such, pelvic muscle tone affects continence (Dumoulin et al., 2014; Pandey et al., 2019) play a critical role in childbirth (Hilde et al., 2013), sexual expression and sexual performance (Whipple et al., 2007; Gianotten et al., 2007), including the eurythmic pelvic muscle contractions experienced during orgasm (Bartlik et al., 2010).
The point of convergence in the pelvic arch is the femoral neck. The most common location for femoral fractures in women is at the femoral neck and fractures at this point of convergence are not uncommon among young female athletes (Kazley & Bagchi, 2020). The outward thrust would increase with age if the female pelvis widens. One study suggests that on average pelvic width can be an inch wider for a septuagenarian than a 20 year-old regardless of height or body fat (Berger et al., 2011). So, incremental changes in weight and weight distribution can have significant effect in the pelvic floor and wellness of the patient.
In addition to an essential role in the dynamic stability of the musculoskeletal structure the pelvic floor muscles directly support a woman’s organs, including the bladder, uterus, bowel, and intestines (Figure 10).

The pelvic floor consists of muscles and connective tissues (ligaments and fascia) that need to work together to form a structural support for the pelvic organs to prevent urinary leakage or protrusion (Bump & Norton, 1998). The pelvic floor extends from the pubic bone at the anterior to the sacrum/coccyx region at the back, and from the inner side from the obturator internus to the outer aspect of the greater trochanter. These muscles form a hammock-like structure supporting the bladder, rectum, and uterus, and ensure the correct functioning of the organs by assisting with the closing of the bladder and bowel passageways to prevent leakage (Kegel & Powell, 1950; Peters, 2000). When the muscles relax with control, their relaxation facilitates efficient emptying of the bladder and bowels, and sexual intromission. Urinary incontinence is the involuntary voiding of urine (Haylen et al., 2010).
Muscle tone is the ability to contract and relax the muscles with control. If the pelvic floor muscles cannot relax, voiding of the bladder and bowels can be difficult and sexual intromission painful. If the pelvic muscles lose their tone from strain, injury or atrophy, the organs shift from their natural position. Pelvic organ prolapse happens when the muscles of the pelvic floor weaken and cannot hold the organs in place firmly. Studies indicate leading causes for loss the of female pelvic floor muscle tone include; pregnancy and prolonged labor (Masenga et al., 2019), obesity (Greer et al., 2008), pelvic surgery (Bø & Sundgot-Borgen, 2001) and perhaps age or menopausal status (Kołodyńska et al., 2019; Simeone et al., 2010). The development of the urinary tract suggest a potential genetic predisposition for some (Aoki et al., 2017) (Conway et al., 2010). Most studies, but not all (Bø & Sundgot-Borgen, 2001; Dockter et al., 2020), indicate women who exercise have three times the risk of experiencing urinary incontinence (Teixeira et al., 2018; de Mattos Lourenco et al., 2018) and vaginal prolapse (Eliasson et al., 2002; Poswiata et al., 2014).
The prevalence of urinary incontinence and stress urinary incontinence is high especially among young, nulliparous elite athletes (Bø, 2014). As the visceral organs incrementally shift, they increasingly put their weight on top of the bladder and pelvic floor. The increasing pressure on the bladder can gradually overwhelm the muscles that control the release of urine. These muscles include the trigonal muscles at the bladder neck and the striated slow-twitch fiber muscles of the urogenital sphincter of the urethra. When the pressure from the weight bearing down on the bladder is greater than the strengths of these muscles to hold the urine, the muscles give way and the body leaks urine. When the body leaks urine from this type of strain on the muscles it is called stress urinary incontinence (i.e., the complaint of involuntary loss of urine during effort or physical exertion, or during sneezing or coughing) ((Haylen et al., 2010). This is the most common symptom. Less common, subtypes of these incontinence symptoms in women include postural incontinence (the loss of urine when moving) and coital incontinence (the loss of urine during sexual intercourse). Interestingly, coughing generates higher pelvic floor muscle strain, measured in intra-abdominal pressure (IAP), than most exercises (Bø & Nygaard, 2020) and as such, repetitive incremental strain can contribute to pelvic floor muscle strain and the involuntary loss of urine (Miller et al., 1998).
The muscles of the pelvic floor work in concert with a number of muscles of the bladder to hold and empty urine. These muscles respond to intra-abdominal (urinary voiding) cues. When these muscles contract spasmodically, the voiding is called urge incontinence (U.S. National Library of Medicine, 2016) or over active bladder. The urge to void can be sudden or with little warning. ‘Functional incontinence’ may be used to describe voiding that results from limited mobility (e.g., hip fracture limiting the patient’s ability to get to the toilet) or dementia - the ability to process information about bladder fullness (Sinclair & Ramsay, 2011). The symptoms of stress and urge incontinence often coexist. The combination of these symptoms is termed mixed incontinence. There appears to be a high risk of mixed, urge and stress incontinence and vaginal prolapse across multiparous and nonporous women who exercise.
Since the musculoskeletal structure is interactive and unique to the individual the type of exercise, intensity of training and the predisposition of an individual to incontinence or prolapse is significant in the risk of a woman experiencing urinary leaks or organ decent. Studies show the ability of women to tolerate significant increased pressure and the corresponding downward pressure without causing urinary leaks or organ decent depends on the individual (Constantinou, C. & Govan, D., 1982). While the range of reported prevalence for urinary incontinence of adult women ranges from 40 to 50% (Manassian et al., 2003), female athletes, of all ages, have a significant risk of developing female urinary incontinence over the general population. The prevalence of urinary incontinence among female athletes in different sports increases with age and long training hours (Simeone et al., 2018).
A prevalence study of urinary incontinence in female athletes ranked sports into three categories of impact; high, medium and low. Involuntary leaks experienced while training and during formal competition are included. The categorization method across a number of sports; including equestrian (Alanee et al., 2010) and cross fit (Sherman et al., 2997) appears below:

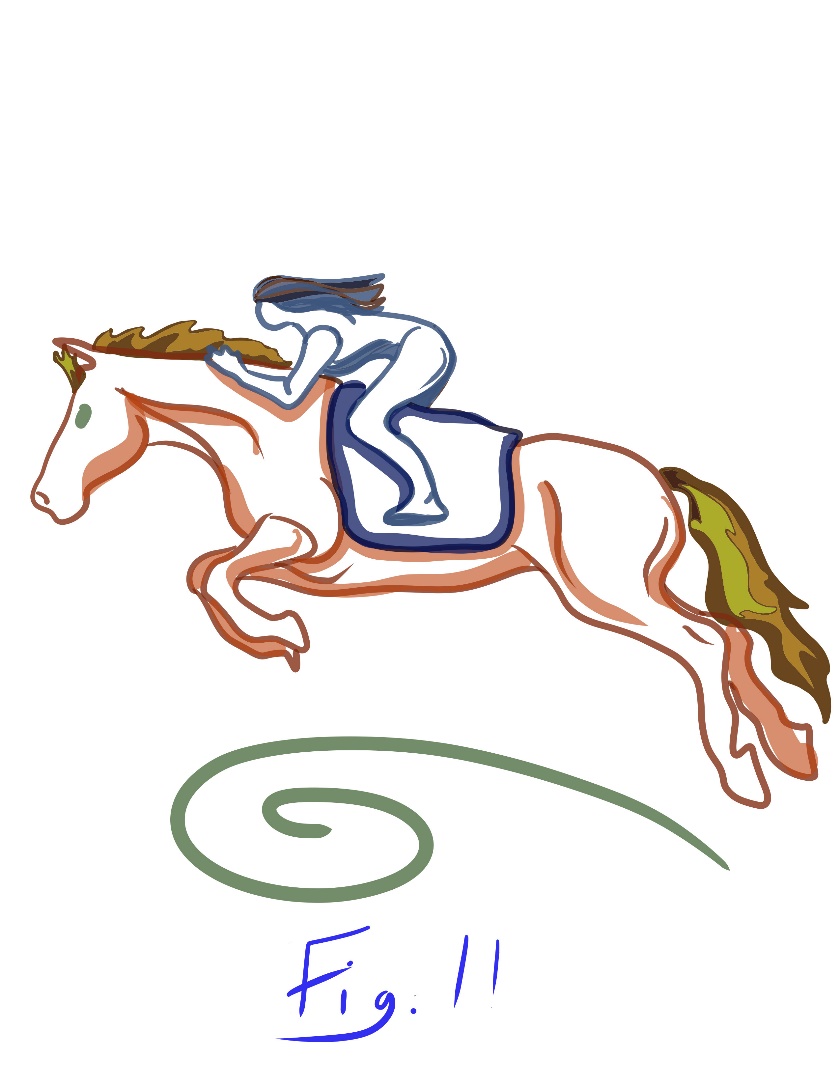
Most elite female athletes are collegiate and nulliparous. 12.5-80% of nulliparous athletes (sans childbirth life experience) suffer from urinary incontinence, clearly suggest the female athletic population at all adult ages are at higher risk for pelvic floor dysfunction (Ward, 2020; Carls, 2007). While female equestrians of all ages manage significant Newtonian forces in training and competition, experienced equestrians learn to carry their weight in the stirrups and the rider’s body is at an acute angel to the horizontal (see image #11). This relief of relieve pressure on the perineal area at the point of convergence – across the perineal area outward to the femoral neck may decrease the risk incontinence and organ decent (Alanee et al., 2009) – perhaps explains why the risk for experienced female equestrians of all ages appears concordant with the general population. This relief of relieve pressure on the perineal area at the point of convergence may explain why 38% of women trampoliners who stopped training reported a cessation of symptoms (Eliasson, 2008).
Parous women who exercise long term (e.g., 30 or more minutes a day more than three times a week for over 37 weeks) have a larger cross-sectional area of the pelvic floor muscles and a wider and stiffer levator hiatus (Bø et al., 2018). This would be concordant with the horizontal and thrust components of the forces in the gothic pelvic arch. Simply, women who exercise regularly do not automatically have better pelvic floor muscle control (Nygaard, 2013). Since most elite female athletes are collegiate and nulliparous, strain to ligaments, fascia, muscle fibers and nerves may be minimal and the intensity of their training could be higher than that in the general population. Figure 10
shows the levator hiatus in the pelvic floor where it is traversed by three different important organ systems: the urethra for voiding urine, the anorectum for elimination of solid waste, and the vagina for intromission and reproduction. The enlargement and stiffening of the levator hiatus may be associated with substantial disturbance of the function of these organ systems and appears to correlate strongly with pelvic organ descent (Dietz, 2017). This widening may also suggest why, when placed under stress, athletes and mothers may experience incontinence and organ prolapse.
Pelvic floor muscle training has shown to increase the thickness of the muscles, reduce muscle length, reduce the levator hiatus area, and lift the levator plate to a more cranial level inside the pelvis in women with pelvic organ prolapse (Bø, 2014) suggesting exercise is not exclusively why female athletes may have high risk for incontinence and organ prolapse.
Staying active throughout life is important. Physical activity is associated with reduced risk of premature death, coronary heart disease, stroke, hypertension, type 2 diabetes, metabolic syndrome, colon cancer, breast cancer, and depression (Galson, 2009). Exercise helps to build muscular fitness and bone density. Pelvic floor muscle re-education can treat female urinary incontinence (Newman et al., 2009) and indications suggest improved pelvic floor muscle tone has positive effect in the treatment of organ prolapse (Bø, 2006). Indeed, pelvic floor muscle training during pregnancy appears to have no negative effect on length of labor or mode of delivery. Pregnant women who do pelvic floor exercises are 62% less likely to experience urinary incontinence in late pregnancy and 3–6 months postpartum have a 29% lower risk of urinary incontinence postpartum (Woodley et al., 2017). Training the pelvic floor muscles with exercise reduces the risk of urinary incontinence by 50% when performed prenatally, and 35% when performed postnatally (Lee et al., 2008). It also results in a 4.6% reduction in cases of established pelvic organ prolapse. So, regular muscle training is a very real prevention measure as well as a cause.
Studies suggest 11% to 20% of incontinent athletes will discontinue the activity because of incontinence, 11% to 18% will modify their performance to limit leaks and 5% choosing to change from training in a gym to home-based exercise (Coyne et al., 2013). 55% will wear an absorbent pad. Because urinary incontinence is considered a stigmatizing condition in most cultures, acknowledging the condition is difficult for the individual. Most all athletes will discuss joint and muscle pain, a majority of women but will not address their urinary incontinence with a licensed healthcare professional (Helfand, 2010) even though treating the symptoms instead of the cause can be expensive (Subak et al., 2008; Chong et al., 2011) and performance limiting (e.g., limit performance to minimize leaks in competition). For older female athletes a break at the femoral neck can be more than expensive. So, lack of pelvic floor training in female athletes affects performance and cost.
Young, nulliparous women in general, and athletes in particular, have low level of knowledge about the pelvic floor and little knowledge about how to train the muscles of the pelvic floor (Cardoso, 2018). For most females it has been generations since women in families and sociopolitical groups shared their skills of pelvic floor muscle control (Hughes, 2005). For a significant number of women who try to tone their pelvic floor muscles with patient-initiated Kegel exercises, as many as 60%, find it difficult to determine if their pelvic muscle exercises have been performed correctly, even when guided by a licensed healthcare professional (Bump et al., 1991). As with any exercise, the benefit gained is significantly diminished if the Kegel exercise protocol is poorly executed. This may be at the core of understand why women how perform muscle training of their pelvic floor are still at risk. Women who have accurate perception of their body and understand function have much better performance capabilities than women who do not and many women do not perform Kegels correctly.
To overcome this limitation and significantly increase patient compliance, a medical device can be used to transmit a mild electronic impulse to the muscles. These mild impulses instruct the muscles to work and rest. The electronic muscle instruction technology is termed neuromuscular stimulation. For pelvic floor muscle tone, the technology is sometimes termed AutoKegel, a registered trademark. The work-rest action of the electronic stimulation mimics self-initiated exercise with safe and reliable outcomes that are comfortable as well as clinically proven. Neuromuscular stimulation is not bio-feedback technology. Bio-feedback devices do not instruct the muscles to work and test. Biofeedback technology only measures the mild neuroelectric signals from self-initiated muscle action.
Pelvic floor muscle tone has significant impact on quality of life and musculoskeletal performance. The literature suggests a convincing comorbidity in adult women between pelvic floor muscle tone performance is sport, sexual dysfunctions and an increased incidence of depression. Even after adjusting for comorbidities and the physical discomfort there are financial burdens (Ganz et al., 2010) and social burdens (Newman et al., 2009).
Subjects, Methoods & Materials
Eligible participants were adult females who owned a specific Over-The-Counter medical device for toning the female pelvic floor (www.yarlap.com) (Relevium, 2016). The device is FDA Cleared for use in a non-clinical environment by a lay-person without active oversight by a healthcare practitioner. Each eligible participant had purchased the medical device online. Some purchased the device directly while others purchased the devices indirectly through a medical device distributor at the recommendation of a licensed healthcare professional. No information on the race, age, ethnicity, resident mailing address or country of national origin of any candidate participant in the study was requested to be known. An independent polling firm used a proprietary anonymized hierarchal randomization scheme to select 3,000 e-mail addresses from a pool of 6,500 potential candidate participants addresses. Invitation to participate in the study occurred via email only. While in person and mail surveys respectively have superior response rates (Sheedan & Hoy, 1999), e-mail surveys have demonstrated superiority over postal surveys in terms of response speed and cost efficiency (Asch et al., 1997). The sensitivity of the subject matter was a significant factor in selecting a survey by e-mail. Since for pelvic floor muscle issues can be intensely personal, some eligible participants may have purchased the device as a surrogate and did not respond because they could not or wished not to report outcomes. Other eligible participants may have elected not to participate in the survey not trusting a pledge of digital anonymity. Some eligible participants may not have responded because their e-mail address had changed and the survey was not electronically forwarded. Finally, the survey may have been filtered by server or security software in such a way that the eligible participant did not see the survey in time to respond. The extent to which any of these potential scenarios influenced the overall participant response rate is unknown.
The study instrument was a nine-point questionnaire. The survey reading level was advanced (i.e., U.S. eighth-grade) by means of the Flesch-Kincaid Grade Level Formula (Flesch et al., 1975). Three questions were closed-ended. Six questions were open-ended. Responses for open-ended questions were limited to 250 characters. The 250 character response allowance was adequate. The 250 character allotment for each open-ended response allowed each of the respondents to elaborate on the outcome without prejudicial prompts which a closed end scale might direct. No respondent used all 250 characters.
One open-ended question asked respondents to describe any outcomes that differed from the device’s stated indications for use and then use a Likert Scale to provide a personal hierarchy for any off-label outcome(s). The Likert Scale ranged from 0 to 4; 0 denoting no outcome, 1 suggesting slight improvement, 2 reporting moderate improvement, 3 indicating significant improvement and 4 signifying an excellent outcome.
The survey was designed to be completed within 5 minutes. The survey was sent on a Thursday afternoon (14:00 Hrs GMT), in a week neither preceded or followed by a holiday or extended (e.g., 3 day weekend). Eligible participants were given a window of 100 hours to respond to the survey. A survey reminder was sent at 72 hours. A survey minimum of 100 responses was deemed acceptable for analysis (Van Bennekom, 2002). Two hundred and twenty-eight randomly selected users of the device responded. While the response rate is low (4.3%), it is not discordant with email surveys on other patient sensitive clinical issues (Sliverman et al., 2018). We believe it reflects the sensitive nature of pelvic floor issues. Among the respondents only 6% answered all of the questions in the survey. The survey was designed by the authors of this article. The questionnaire was not formally evaluated for reliability or validity. No adverse events or potentially hazardous situations were reported from completing the survey nor from use of the device itself.
Measures
Newtonian horizontal thrust components of the forces in the pelvic gothic arch in the musculoskeletal structure did appear when survey participants related their unexpected quality of life outcomes from improved pelvic floor muscle tone. Forty-six percent of the respondents reported improved freedom of movement as an unexpected outcome from improved pelvic floor muscle tone. Textual responses corroborated the outcome confirming range of motion to greater ease in movement. While freedom of movement is a component of sexual expression (Reider, 2020) (e.g., flexibility adequate to achieve desired intromission) the textual component of the response allowed the appropriate categorization of the outcome (see below).
Thirty-eight percent reported reduced lower back pain (Postpartum Symphysis Diastasis is a different diagnosis and treated differently, see Notes). This number correlates well with the 31% that reported improved thigh and knee performance as an unexpected outcome from improved pelvic floor muscle tone. The former included reduced thigh muscle fatigue and the later included reduced knee pain. These unexpected outcomes in relative proportion manifest the
interactive nature of the musculoskeletal structure and the importance of pelvic floor muscle to it. The authors believe, As the pelvic gothic arch deflects from the loss of muscle tone in the pelvic floor, symptoms of incontinence may be preceded for some women, by unexplained lower back pain, then pain in the outer sides of the knees (Reider, 2016).
Twenty-three percent reported improved intimacy; including sexual performance and sexual expression. Sexual performance is the ability to experience tangible muscle performance like orgasmic intensity and eurythmic frequency. Women with muscle tone have the ability to willfully change the symmetry of the spatiotemporal pressure distribution in the vaginal canal (Cacciari et al., 2017). The ability of the woman to clench, release and sustain waveform pelvic floor muscle contractions is known across many cultures by many names, such as Pompoir, Kabazza and Yin-yang Butterfly. Sexual expression is the ability to experience intimacy with confidence and comfort. Emotionally, sexual activity lowers the incident of depression and stress and supports self-esteem and intimacy. Physically, sexual activity can reduce the risk of heart disease and stroke, bolster the immune system, help manage the body posture and pain, improve sleep and can even help individuals appear more youthful.

Newtonian horizontal thrust components of the forces in the pelvic gothic arch in the musculoskeletal structure did appear when survey participants related their unexpected outcomes from improved pelvic floor muscle tone on a Likert scale. Respondents reported outcomes were “Significant” for improved intimacy (2.8) and freedom of movement (3.2). Survey participants reported outcomes were “Moderate to Significant” for reduced lower back pain (2.7) and improved thigh and knee performance (2.5).
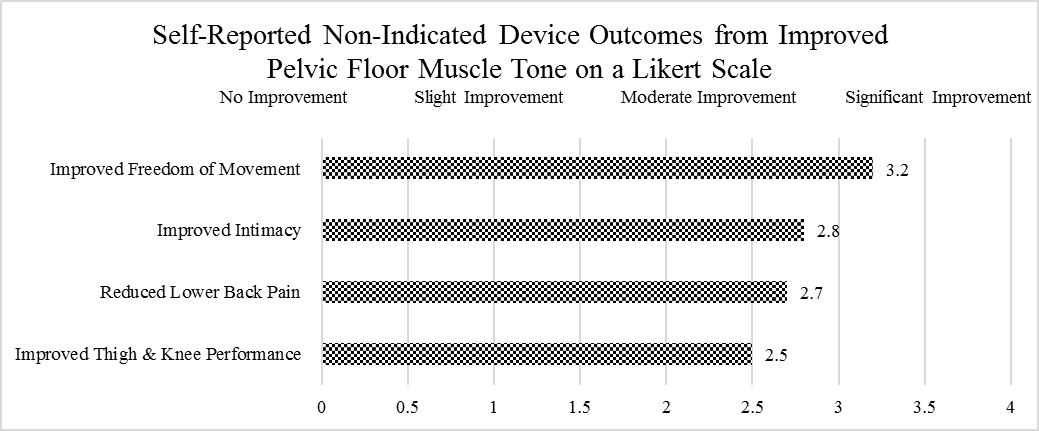
The location (i.e., lower back and lower extremities) is concordant with the musculoskeletal gothic arch concept. The percentage reporting (over one-third) suggest Newtonian horizontal thrust components do impact musculoskeletal performance in many women. The Likert Scale suggest that for those reporting the non-indicated device outcomes are moderate to significant.
The reproductive primacy perspectives widely associated with pelvic floor exercise [and sometimes obsessively] recognized in this study as improved intimacy is only a small part of the therapeutic value of female pelvic floor muscle tone.
Dr. Kegel recognized female pelvic floor muscle tone improves sexual performance and sexual expression. Improved female pelvic floor muscle tone is explicitly recognized as a non-pharmaceutical non-surgical protocol for treating female urinary incontinence. It is proven to correct organ decent and an effective method to maintain urinary control. The authors believe the reduction in pain and improved freedom of movement as a percentage of respondence and the level of self-reported Likert Scale suggest pelvic floor muscle tone may be a direct, simple and highly effective method to manage the Newtonian horizontal thrust components in the musculoskeletal gothic to optimally distribute the forces down through the base of the spine across the pelvis, down through the thighs –minimizing outward forces the hips, transversely at the knees to the heals. Improved musculoskeletal alignment may help address pain women experience when the pelvic floor muscle experience injury, strain or atrophy including post-partum lower back pain. But the data and the math indicate pelvic floor muscle tone should be a part of all in sports training programs. The Newtonian arch math indicates the more intensive the training program, the more important pelvic floor muscle tone is the female athletes for managing the horizontal thrust components in the musculoskeletal structure.
The data reveals the importance of exercise and demonstrates that pelvic floor muscle tone should be a part of all exercise regimes for all women; non-athletes and athletes. While patient specific, the impact level of the training may emphasize importance; never-the-less, pelvic floor muscle tone should be a part of all exercise regimes for all women.
The safety and efficacy of any exercise program is only as good as the protocol. Unfortunately, significant number of women who try to tone their pelvic floor muscles with patient-initiated exercises–as many as 60%–find it difficult to determine if their pelvic muscle exercises have been performed correctly, even when guided by a licensed healthcare professional (Bump et al., 1991). Patient initiated Kegels tends to focus on the contraction of muscle groups when proper muscle tone is the ability to contract and relax the muscles with control. The ability to relax the muscle with control and not to work the muscles to a point of fatigue is important. Biofeedback devices register muscle activity, but patient-initiated muscle contractions (i.e., “true exercise”) of the wrong muscles groups will still register activity. Neuromuscular stimulation can be used as a guide for exercise to improve compliance. Patented predetermined security rules in the firmware permits gaming to be safely incorporated into the therapy protocol (Reider, 2019) The goal of this security feature is give the lay-use user access to the most up-to-date play with purpose (McGonigal, 2015). It provides a clear and secure path to state-of-the-art gaming design for flow and self-expansive outcome(s) (see notes). Research indicates these attributes of purposeful play build self-confidence and real-world problem-solving skills (Primack, 2012). As such enables for the benefit of the user two conjoining leadership projects in academia and medicine.
In addition, patented technology monitors the muscle status to prevent injury to the muscles. If the muscle(s) is unable to perform specific template driven low level contraction challenges and/or exhibits any indications of spasm then the next stimulation cycle is modified so that muscle or muscle group always performs withing safety threshold that changes as the status of the patient changes in real time. Neuromuscular stimulation with biofeedback gaming can be used across the musculoskeletal structure using the proprietary security system that monitors and controls the incoming and outgoing electronic traffic based on predetermined security rules exists; MyoSecure. The authors hope by bring awareness to the importance of female pelvic health as a component of personal and Public Health, gaming design can be used to encourage female software engineers to enter the engineering field by engaging prospective engineers in positive socially relevant engineering projects in software design to help tone the female pelvic floor. For athletes training at a high level or recovering from muscle injury the technology can be coupled with protocols which enable the athlete to fine-tune their muscle control to increasingly higher levels of precision. In effect, artificial intelligence in muscle tone for athletes and non-athletes is real and effective for the female pelvic floor and across the musculoskeletal structure.
Conclusion
Exercise training throughout life is important for health and wellbeing, however, forces that are exerted on the pelvic floor during exercise can strain the pelvic floor resulting in urinary incontinence and organ decent. Kegel exercise protocols are an effective non-narcotic, non-surgical way to improve muscle pelvic floor muscle tone, treat incontinence and organ decent. Researchers conducted a study through a questionnaire with participants who experienced female urinary incontinence and a specific Over-the-Counter medical device for female pelvic floor toning (Yarlap). Results of the study suggested participants improved thigh and knee performance as an outcome from improved pelvic floor muscle tone, reduced thigh muscle fatigue, reduced knee pain, improved intimacy including sexual performance and sexual expression. The results of the study indicate incorporating pelvic floor muscle tone in a woman’s exercise regimen can have broad positive outcomes; including treating female urinary incontinence, maintaining continence and indications suggest improved freedom of movement, improved intimacy, reduced lower back pain and improved performance of the lower extremities. The data suggests exercise and muscle reeducation programs to maintain pelvic floor muscle tone are particularly important for adult female athletes.
Notes
Back Pain: Postpartum back pain is different from Postpartum Symphysis Diastasis. The recommended treatment is not the same. A patient diagnose with Postpartum Symphysis Diastasis would know the difference and not report accordingly (Katonis et al., 2011).
Flow in Gaming: is the state of being completely cogitatively absorbed in an activity (McGonigal, 2015).
Newton’s Second Law of Motion: Also known as the Law of Force and Acceleration, a force upon an object causes it to accelerate according to the formula net force = mass x acceleration. Simply, the acceleration of the object is directly proportional to the force and inversely proportional to the mass (Newton, 1687).
Newton’s Third Law of Motion: For every action (force) in nature there is an equal and opposite reaction. In other words, Forces always come in pairs. When one object exerts a force on a second object, that second object exerts a force that is equal in magnitude and opposite in direction on the first object (Newton, 1687).
Self-expansive Gaming: builds positive problem-solving capabilities. It is not gaming to escape from life issues (McGonigal, 2015).
Survey Open Ended Response: Twenty-three open-ended responses are not included in the table because the outcomes were not musculoskeletal issues. Fourteen of the omitted responses include improved function of the clitourethrovaginal complex, including glandular function (e.g., paraurethral) and arousal (e.g., sensitivity sites). An additional 9 responses were not included in the table because the outcomes described fulfilling personally important socio-economic rolls the respondents valued or were important wellness outcomes that could not be indisputably defined as musculoskeletal issues, including improved appearance and sexual expression. The omitted responses in this regard were significant to the respondent and were lifechanging, but the outcomes described were not unequivocally tracible to Newtonian horizontal thrust components - the preview of this paper.
Disclosure & Conflict of Interests
Brent Reider: The President, Chief Operations Officer and shareholder for Relevium Labs, Inc., a Delaware C-Corporation, the U.S. FDA Registered Specifications developer and manufacturer of the Yarlap (www.yarlap.com). The submitter and assignee of the non-conditional U.S. Patents cited in this article.
Warwick Reider: No conflict of interest known.