Natasha Kesav1*, Martha E. Couce2, Ahmed Omar1, Shree Kurup1
1Department of Ophthalmology and Visual Sciences, University Hospitals Cleveland Medical Center, Case Western Reserve University School of Medicine, 11100 Euclid Avenue Cleveland, Ohio 44106.
2Department of Pathology, University Hospitals Cleveland Medical Center, Case Western Reserve University School of Medicine, 11100 Euclid Avenue Cleveland, Ohio 44106.
*Corresponding Author: Natasha Kesav, Department of Ophthalmology and Visual Sciences, University Hospitals Cleveland Medical Center, Case Western Reserve University School of Medicine, 11100 Euclid Avenue Cleveland, Ohio 44106.
Received Date: July 15, 2023
Accepted Date: July 28, 2023
Published Date: August 04, 2023
Citation: Natasha Kesav, Martha E. Couce, Ahmed Omar, Shree Kurup. (2023) “Case Report: Conjunctival Lymphangiectasia Masquerading as Pseudoscleritis”, Ophthalmology and Vision Care, 4(1); DOI: http;//doi.org/08.2023/1.1041.
Copyright: © 2023 Natasha Kesav. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is a case of bilateral, recurrent conjunctival swelling and redness of the right eye, initially managed as non-necrotizing scleritis without resolution. Conjunctival biopsy and subsequent histopathology confirmed conjunctival lymphangiectasia, surgical resection was completed, and patient’s symptoms subsided. We highlight the clinical course of conjunctival lymphangiectasia, accompanied by pathology, management, and an update on current literature. This conjunctival lesion is helpful for ophthalmologists to consider with sectoral nonrevolving conjunctival erythema and edema.
Introduction:
Conjunctival lymphangiectasias are a rare and challenging ocular disorder characterized by dilated lymphatic channels. Proposed mechanisms encompass congenital malformations, primary lymphatic dysfunction, or acquired cases. Little is reported demonstrating pathology and management in the existing literature. An accurate diagnosis is challenging given its variable clinical presentation and initially, the appearance may resemble other disorders. This middle aged caucasian patient had several years of recurrent conjunctival erythema managed as scleritis. Lubrication and topical steroids provided temporary relief, but excision of the affected conjunctival tissue alleviated all symptoms. This is a rare but important differential to keep in mind.
Case Report:
A 51-year-old Caucasian male was referred for second opinion of blurry vision of the right eye, previously diagnosed as recurrent non necrotizing scleritis. He complained of decreased vision on and off for several years but in the last three months, symptoms have become more frequent, only to self-resolve after 1-3 days. He endorsed no pattern to the symptoms, no time of day, exacerbating factors nor dietary changes. During these flare-ups, the right eye becomes erythematous and edematous, with mild discomfort and eye pressure. These episodes are followed by abdominal bloating, loose bowel movements, and nausea which then also self-resolve. He was prescribed several rounds of oral and topical corticosteroids which infrequently resolved symptoms. Past medical history includes a 20-year history of right sided sinus issues, eczema, gastroparesis, and chronic GERD. He had no ocular history, oncological history, previous surgeries, or family history of gastrointestinal disease. Review of systems were noncontributory.
On ophthalmic examination, best-corrected visual acuity was 20/20 for both eyes (LogMAR of 0). Intraocular pressures were within the normal limits. Slit lamp biomicroscopy of the right eye revealed conjunctival swelling and mild hyperemia of the inferotemporal bulbar conjunctiva (Figure 1). The anterior segment examination and dilated fundus examination of both eyes was unremarkable. Autoimmune workup was initiated including HSV, Lupus, syphilis serology, serum autoantibody screen (including antinuclear antibodies, anti-DNA antibodies, rheumatoid factor, antineutrophil cytoplasmic antibodies). These tests did not support an underlying immune disease. Fluorescein angiography was obtained and revealed an absence of optic nerve hyper fluorescence or retinal vascular leakage to support posterior scleritis extending anteriorly. At this point, there was compelling evidence that this was not consistent with inflammatory scleritis, and decision was made to pursue conjunctival biopsy. A biopsy of the 2x2mm area of inferior bulbar conjunctiva was performed under local anesthesia and histopathological evaluation confirmed the diagnosis of conjunctival lymphangiectasia (Figure 2). The patient had no further recurrence of inflammation or erythema.
He was referred to a gastrointestinal specialist for further evaluation and underwent colonoscopy in 2020 that was normal except for diverticulosis, though random biopsies were not taken. He subsequently had a video capsule that suggested intestinal lymphangiectasia.
Discussion:
This case and in-depth analysis of existing literature provides a comprehensive background on conjunctival lymphagiectasias, highlighting the proposed etiology, patient presentation, diagnostic discussion, and treatment options.
The differential for recurrent sectoral erythema and edema of the conjunctiva is broad. Clinicians must consider neoplastic, infectious, and inflammatory diseases. For this reason, a stepwise approach should be taken to exclude certain conditions. In this case given clinical appearance and recurrent symptoms, the initial suspicion non-necrotizing scleritis as the initial diagnosis and pursued initial workup including detailed serologic testing with autoimmune and infectious markers, which were all negative. Furthermore, symptoms did not coincide with institution of systemic corticosteroids which would be expected to reduce the inflammatory process.
At this point, the differential of localized chemosis and swelling of the conjunctiva broadens. Conditions such as conjunctivochalasis will present with a diffuse pattern and are mostly found in elderly population. Increased vascular permeability due to vasomotor instability or allergy can also drive fluid into the interstitial compartment resulting in chemosis. Edema may also be a result of periocular surgery, trauma, or elevated hydrostatic pressure in conditions such as nephrotic syndrome, or local venous hypertension (thyroid eye disease, cavernous sinus thrombosis, etc). While these conditions should be considered, our patient did not have a history consistent with these findings and a more definitive diagnosis was pursued via biopsy.
This condition was first reported in the literature in 1880 by the name “lymphangiectasias haemorrhacica conjunctiva” describing a variant associated with hemorrhage. This is a relatively uncommon disease caused by abnormal connection or obstruction between enlarged conjunctival lymphatic and blood vessels, which gives rise to intermittent rapid filling of lymph channels with blood. Depending on chronicity of conjunctival swelling the patient may experience symptoms of tear film disruption. Characteristic manifestations include cystic lesion of the conjunctiva (which may mimic allergic chemosis), or a beaded dilatation of lymphatic vessels with a “string of pearls appearance” [1].
The diagnosis of conjunctival lymphangiectasia is made based on clinical appearance and histology, which were confirmed after biopsy in our patient with permanent resolution of symptoms. In most cases, symptoms associated with this lesion improve spontaneously but in recurrent cases direct surgical excision to the affected conjunctiva can provide permanent relief [1-3]. A case series of 11 biopsy proven lesions had no recurrence with after surgical excision with no graft (n=6), with amniotic membrane transplant (n=3), or combined with conjunctival autograft (n=2) [4]. Liquid nitrogen cryotherapy has also been formed with resolution in several cases [5].
In conclusion, conjunctival lymphangiectasias are a rare but clinically significant condition which may pose diagnostic challenges for ophthalmologists. This case offers the opportunity to shed valuable insights into the clinical presentation and management options for this condition. While the pathogenesis and risk factors remain unclear, evidence suggests an interplay of physiologic mechanisms. There is no definitive cure, however a physician-patient discussion may include options including conservative measures or surgical intervention. Collaborative efforts among clinicians will enhance our understanding of conjunctival lymphangiectasias and management of this challenging ocular condition.
Figure legends:
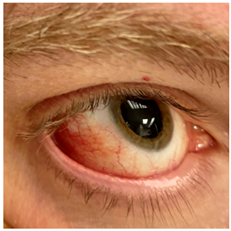
Figure 1: External image of the right eye revealing conjunctival swelling and mild hyperemia of the inferotemporal bulbar conjunctiva.
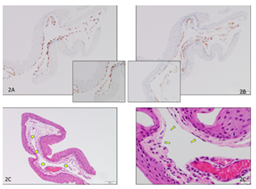
Figure 2: Figure 2a represent Hematoxylin & Eosin stains showing submucosal cystic lesion in 100x (yellow stars) and attenuated endothelial lining in 400x (arrows).
Figure 2b represent Immunohistochemical stains with ERG antibody (endothelial marker) highlighting cyst endothelial lining in brown (diaminobenzidine ) 100X and 400x
Figure 2c represent Immunohistochemical stain with D2-40 antibody (lymphatic specific marker) highlighting cyst endothelial lining in brown (diaminobenzidine ) 100X and 400x
Data availability: The data used in this current case is available from the corresponding author on reasonable request.
Conflicts of interest: No conflicts of interests exist for any author.
Ethical Approval: For this type of study, ethical approval is not required
Financial Disclosures: No authors have any proprietary interests or financial disclosures.
Consent: Consent for publication was acquired from the patient.
Funding statement: This research was supported by NIH Vision Research Core Grant P30 EY011373P30 (Case Western Reserve University) as well as internal funding of University Hospitals Eye Institute