Allen Dang 1, Akshay Jakkidi Reddy 2*
1 Department of Anesthesia, California Northstate University, Rancho Cordova, United States of America.
2 Department of Ophthalmology, California Northstate University, Rancho Cordova, United States of America.
*Corresponding author: Akshay Jakkidi Reddy, Department of Anesthesia, California Northstate University, Rancho Cordova, United States of America.
Received date: February 08, 2021
Accepted date: February 16, 2021
published date: February 18, 2021
Citation: Dang A, Akshay J Reddy. “The Application and Usage of Anesthetics in the Surgical Treatment of Diabetic Macular Edema.’’. Ophthalmology and Vision Care, 1(1); DOI: http;//doi.org/03.2021/1.1001.
Copyright: © 2021 Akshay Jakkidi Reddy. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Diabetic macular edema is a rapidly proliferating disease that has affected the lives of many individuals in the world. Current development of the integration of subthreshold micropulse laser has suggested the prioritization of laser therapy in diabetic macular edema treatment; however, vitreoretinal surgery in conjunction with anesthetics is seen to correlate with earlier mitigation of damage to the fovea. Surgery is a delicate process that requires substantial consideration of the types of anesthetic used and where they are being used. Different medications and protocols may be required depending on the individual being treated. For instance, some individuals may be allergic to traditional anesthetic medicine and would end up with more severe complications. The literature reviewed suggested that topical lidocaine was the most used anesthetic for vitreoretinal surgery. However, alternatives to lidocaine exist, and their effects should be explored. Therefore, we wish to highlight the effects of each of the different surgical drugs and anesthetics used in the treatment of diabetic macular edema.
Introduction
Diabetic macular edema (DME), described as the leakage of fluids from blood vessels in the retina, is an increasingly prevalent diabetic eye disease and the leading cause of vision loss in developed countries [1]. In Americans with diabetic retinopathy alone, over 750,000 cases were reported in 2019 [1]. When DME is left untreated, excess fluid in the retina causes swelling in the surrounding tissue of the macula and, as a result, permanent damage to the fovea of the eye [2]. Symptoms of DME can range from blurred vision and loss of contrast to complete loss of vision. Due to the widespread presence of DME, many new and innovative treatment procedures have been developed. The most predominant advancement in treating DME has been the integration of subthreshold micropulse lasers (SML) to laser therapy [2]. SML performs the same function as conventional continuous-wave lasers but avoids the adverse side effects attached [2]. Although laser therapy is widely popular and new developments have been made in the field, the use of advanced anesthetics in vitreoretinal surgery has been seen to correlate with more prompt intervention in DME treatment [2]. In the case of DME, earlier surgery can help mitigate damage to the macula and prevent further deterioration to the fovea. It is important to consider the anesthetics used in these surgeries as reducing harm to the patients is one of the primary goals of healthcare professionals. We wish to view different studies and analyze the usage and location of anesthetics during DME surgical processes.
Methods
A literature search of articles published between 1978 and 2021 using PubMed was performed using the keywords "anesthesia" and "diabetic macular edema." Cases that focused on non-diabetic macular edema, diabetic retinopathy, cataracts, or did not mention anesthetic medication being utilized were not included in the study. Abstracts and titles were assessed to ensure that anesthetics were being discussed in the context of surgery to treat diabetic macular edema. Only articles in either English or Spanish were adopted into our analysis.
Results
The database search using the stated parameters yielded a total of 32 publications. A total of 17 articles describing surgical procedures that involved anesthetics and patients with diabetic macular edema met our search criteria. Information extracted from each report were sample size, the areas of applied anesthetic usage, the type of drugs that were injected, and the type of anesthetic that was used.
The studies that were analyzed in the review had an average sample size of 59.4, saw lidocaine (70.58%) as the most common anesthetic being used, most prominently applied topical anesthesia (64.71%), and had triamcinolone acetonide (88.24%) being used as the most commonly injected drug (Table 1).
|
Table 1 - Summary of previous clinical studies of surgical procedures to treat diabetic macular edema [7,17 ] |
||||
|
Author (year) |
Area(s) of applied Anesthetic |
Type(s) of anesthetic |
Drug(s) in injection |
Sample Size (Eyes) |
|
Besirli (2020) |
Subconjunctival, Topical |
CA, LC |
AVEGF |
44 |
|
Diaz-Llopis (2008) |
Topical |
TC |
APE |
18 |
|
Diaz-Llopis (2009) |
Topical |
TC |
APE |
16 |
|
Jonas (2004) |
Topical |
LC |
TA |
24 |
|
Jonas (2001) |
Topical |
LC |
CC |
2 (case report) |
|
Kaderli (2006) |
Subconjunctival, Topical |
LC |
TA |
56 |
|
Karacorlu (2004) |
Topical |
LC |
TA |
2 (case report) |
|
Koga (2005) |
Topical |
LC |
TA |
20 |
|
Kyto (2005) |
Subconjunctival |
LC |
TA |
2 (case report) |
|
Lin (2007) |
Topical |
LC |
TA |
18 |
|
Mansour (2020) |
N/A |
N/A |
N/A |
N/A |
|
Massin (2004) |
Subconjunctival |
LC |
TA |
15 |
|
Ozkurt (2015) |
Topical |
LC |
TA |
42 |
|
Rifkin (2012) |
Topical |
TV, TC, PR |
AVEGF |
120 |
|
Shirohima (2014) |
Topical |
LC |
AVEGF |
260 |
|
Song (2011) |
Topical |
BC |
TA |
58 |
|
Sutter (2004) |
Subconjunctival, Topical |
LC |
TA |
69 |
|
Xing (2014) |
Subconjunctival, Topical |
PR, LC, TC |
TA |
75 |
Table 1: Summary of previous clinical studies of surgical procedures to treat diabetic macular edema [7,17 ]
Abbreviations
TA triamcinolone acetonide, BC bevacizumab, LC lidocaine, N/A Not Applicable, PR proparacaine, TV tetravisc, TC tetracaine, CA cooling anesthetic, APE autologous plasmin enzymes, AVEGF anti-vascular endothelial growth factor, CC crystalline cortisone, DME diabetic macular edema
Discussion
Various patients who have had the condition known as diabetic macular edema over the past 20 years have had surgical treatment in order to eliminate the disease. The surgery is an invasive procedure that removes the vitreous adjacent to the detachment of the posterior hyaloid. Additionally, any epiretinal and internal limiting membranes are removed through peeling. The detachment of the posterior vitreous has previously been associated with greater resolution of DME. Furthermore, vitrectomy has been stated to improve DME conditions through several biological mechanisms [2]. Examples of these mechanisms include improved retinal oxygenation, greater removal of VEGF loads, and liberation of abnormal vitreomacular adhesions [2]. As the data shows, surgery is a very effective method of treating diabetic macular edema. As such, it is important to consider the application and usage of anesthesia during these procedures in order to minimize patient harm. When surgery is performed to rid the patient of this ailment, there are two main areas of the eye where anesthetics are utilized. Generally, during DME surgery, the surgeon applies the anesthetic topically or subconjunctivally [3]. Although some physicians use anesthesia both topically and subconjunctivally [3-6], the majority of healthcare practitioners solely utilize topical anesthesia [7-17]. While applying anesthesia subconjunctivally is known to reduce patient harm more than topical anesthetics, it has been shown to potentially cause subconjunctival hemorrhages [4]. It is most likely for this reason that most surgical procedures involving DME only apply anesthesia topically and not subconjunctivally.
The surgery for treating diabetic macular edema involves injections of drugs that counteract the symptoms caused by the disease. Specifically, drug implementation targets the swelling of the macula in an attempt to protect the patient's fovea from damage [2]. Additionally, surgical injections seek to correct the disruption of the blood-retinal barrier and upregulation of retinal vessel leukostasis [18]. The most popular pharmaceutical that ocular surgeons utilize for this procedure is TA. This is most likely due to the fact that TA is a well-established anti-inflammatory in medical procedures [19]. Due to the fact that TA causes anti-inflammatory effects on the macula, it is one of the best treatment options to use in order to alleviate the previously aforementioned complications caused by DME. The majority of studies analyzed in Table 1. have shown that TA is the most used intravitreal drug used in DME surgical procedures. Although TA is the most commonly used drug for this procedure, it is not the standard pharmaceutical that is utilized. The medically standard drug for this procedure is AVEGF. This is most likely due to TA being a relatively newer drug in the pharmaceutical market [20]. While both TA and AVEGF are anti-inflammatory agents, TA has proven to be better at reducing the central thickness and improving best-corrected visual acuity [19]. In post-clinical studies, TA has also been proven to have more long-term beneficial effects on patients' vision in comparison to AVEGF [19]. As more clinical and post-clinical studies are performed, perhaps TA will replace AVEGF as the new standard of care. In order for surgeons to inject TA into patients with DME, the patients must first be given anesthetics to prevent the pain that they may feel during surgery. Therefore, the consideration of the type of anesthetics is vital when discussing DME treatment.
The most common anesthetic used for DME surgical treatments is LC. LC is an amino acid derivative local anesthetic that blocks the signal transmissions between nerves. Since LC is an antiarrhythmic molecule, it also reduces sodium channel transportation and thus the patient's heart rate [21]. This is an effective method in reducing the blood leakage in the macula as it decreases the overall blood flow to the eyes. LC has been widely utilized in various eye surgeries such as cataract removal, LASIK, and DMEK [22-24]. This is because LC is extremely versatile and can be applied both directly to the skin or in the mucous membranes. Although LC typically takes between several minutes to three hours to take effect, its effect as an anesthetic is profound [21]. The majority of studies analyzed in Table 1. have shown that LC is the most used anesthetic in DME surgical procedures. However, in some of the earlier studies, TC is used as opposed to LC. This is most likely due to the fact that TC has been used in the medical field for a longer period of time than LC, but after analyzing clinical studies, it has been shown that LC is more effective at relieving pain felt by the patient than TC [25-27]. The comparison of relative pain experienced by patients exposed to LC or TC during surgery is displayed in Figure 1.
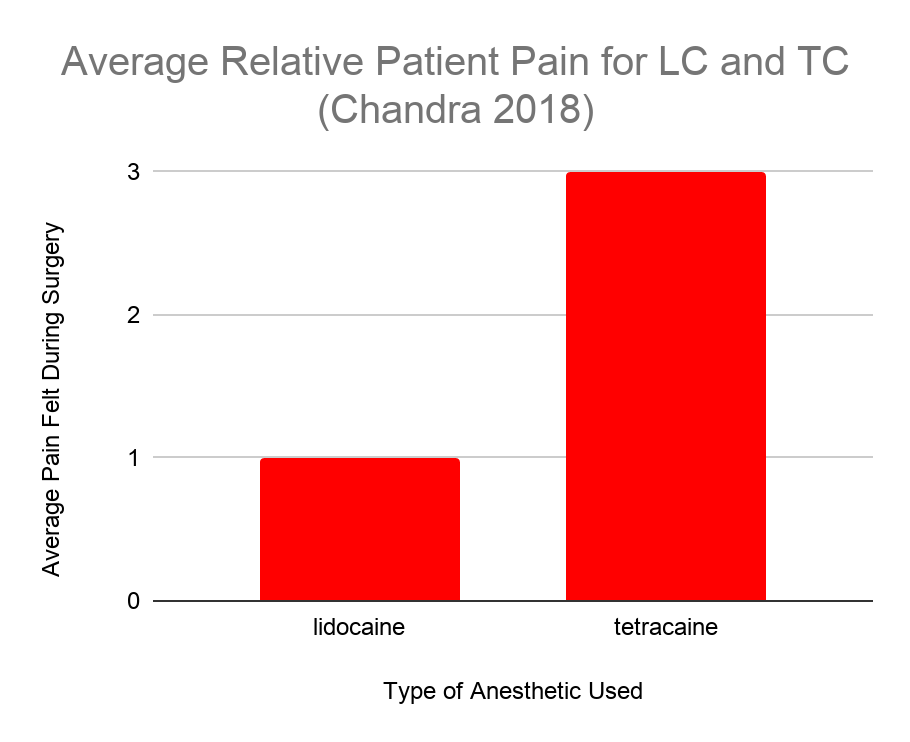
Figure 1: Comparing Average Relative Pain Felt By Patients When Using Lidocaine and Tetracaine Based off of data Compiled from Chandra (2018).
So, although TC has been used by physicians for a longer period of time, LC is predominantly used by surgeons for the treatment of DME as it has been shown to be a more successful anesthetic.
As we have previously discussed, LC is most likely one of the best anesthetics used for DME surgery. However, it is not a one size fits all solution. There are many individuals who exhibit allergic reactions when exposed to LC and other anesthetics [3]. Therefore, LC, in some instances, can further exacerbate the conditions of DME by proliferating further inflammation in the macula. Thus, alternative anesthetic measures are currently being developed and studied in order to provide treatment to those who are hypersensitive to traditional anesthesia. CA is one such method that has been developed to meet these demands. When eye tissue is exposed to extremely cold temperatures, it causes the body to produce opioid-mediated stress-produced analgesia [28]. CA is a treatment that essentially involves cooling the patient's eyes to very low temperatures in order to increase the pain threshold so that the surgeon can perform the procedure successfully while minimizing patient harm. CA is a form of anesthesia that does not rely on synthetically produced chemicals. As a result, CA does not result in as many treatment complications as traditional anesthetics. In fact, recent research has shown the CA results in a 12% reduction in transient adverse effects when compared to the typical standard of care [3]. The comparison of transient adverse effects experienced when patients are exposed to LC or CA during treatment is displayed in Figure 2.
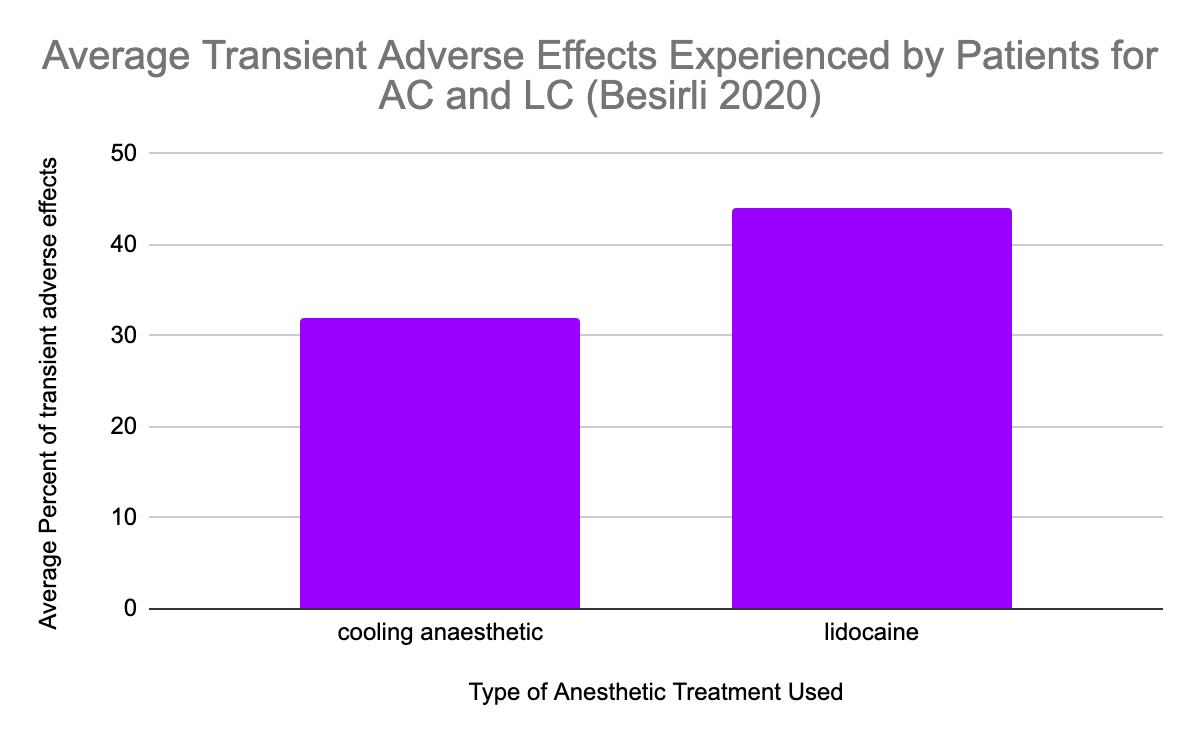
Figure 2: Comparing the Average Percent of Transient Adverse Effects Experienced by Patients When Using Lidocaine and Cooling Anesthetic Based off of data Compiled from Besirli (2020).
Although CA is a very promising form of alternative anesthesia, it should be used with great caution. CA is known to cause the desired anesthetic effect when the temperature of human tissue reaches -10°C. However, permanent cell damage could occur if temperatures reach below -20°C [3]. This review analyzes and reports the data that is collected from numerous different sources regarding the usage of anesthesia in the surgical treatment of diabetic macular edema. As a result, the conclusions presented in this study are limited by the current scope of the literature regarding this topic.
Conclusion
Diabetic macular edema may become a more prominent disease in the future, given how many patients currently suffer from diabetes. Therefore, it is essential to consider the various treatment options and their long- and short-term effects on individuals when fighting this disease. One of the types of treatments for DME is surgery, and its effects can vary according to the type of anesthetic that is used during the procedure. Although lidocaine is the most predominantly used anesthetic in DME surgery, it may not be the most effective and safe anesthetic in the future, given the promising research and results of cooling anesthesia. The literature seems to support the notion that the inaesthetic for this procedure should be applied topically and that triamcinolone acetonide should be the primary pharmaceutical injection for standard care of DME. Perhaps future research could prove other non-medicated anesthetic techniques can be more effective than the current traditional standard of care.