Ophthalmology and Vision Care
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Feliciana Menna *, Alex Casanova, Andrea Consigli and Moreno Menghini
Department of Ophthalmology, Ospedale regionale di Lugano, Switzerland.
*Corresponding Author: Feliciana Menna, Department of Ophthalmology, Ospedale regionale di Lugano, Switzerland.
Received Date: September 24, 2022
Accepted Date: September 28, 2022
Published Date: October 04, 2022
Citation: Feliciana Menna, Alex Casanova, Andrea Consigli and Moreno Menghini. (2022) “Uncommon Presentation of Punctate Inner Choroidopathy (PIC)”, Ophthalmology and Vision Care, 2(3); DOI: http;//doi.org/09.2022/1.10234
Copyright: © 2022 Feliciana Menna. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Purpose:
To report an uncommon case of a 44-year-old healthy and myopic male diagnosed with unilateral neuroepithelial detachment and subfoveal RPE/Bruch membrane interruption secondary to punctate inner choroidopathy.
Methods:
The case report is based on data from clinical records, patient observation and analysis of ancillary diagnostic tests.
Results:
A 44-year-old healthy and myopic male presented to our emergency service with complaints of a paracentral scotoma in the right eye noticed several weeks prior, and that now was becoming larger and darker. Past medical and family history were unremarkable. Visual acuity was 1.0 with correction in the right and 1.0 with correction in the left eye, respectively. Dilated fundus exam showed a small yellowish spot inferior to the fovea in the right eye (fig. 1); dilated fundoscopy in the left eye was unremarkable. There were no signs of inflammation in the anterior chamber or vitreous cavity bilaterally.
Spectral-domain optical coherence tomography (SD-OCT) revealed a neurosensory retinal detachment associated with a focal disruption of the RPE/Bruch’s membrane layer giving the impression of a choroidal excavation. In addition the OCT showed accumulation of subretinal hyperreflective material (SRHM) at the area of RPE disruption(Fig 2a, 2b).
Fluorescein angiography (FA) performed at presentation revealed a ring shaped area of mild dye leakage foveally with a few hyperfluorescent spots spread at the posterior pole. There were no signs of retinal vasculitis nor papillitis (Fig. 3).
Indocyanine green angiography (ICG) showed hypofluorescent spots corresponding to the hyperfluorescent lesions seen in the FA, and a large hypofluorescent lesion foveally. There were no unambiguous signs of choroidal neovascularization in both angiographic modes (Fig. 3).
Ancillary tests done for typical infectious and autoimmune chorioretinopathies and uveitis were all negative.
A diagnosis of punctate inner choroidopathy was established based on the clinical presentation, and the multimodal imaging. The differential diagnosis of a secondary CNV was abondoned as a result of the missing unambiguous angiographic signs. Systemic corticosteroid treatment was initiated at a dose of 1 mg/Kg/body weight for 4 weeks.
At one month follow up the OCT showed almost complete resolution of the subretinal fluid and SRHM (Fig. 4,5). Visual acuity was 0.3 with correction in the right eye. At the area of presumed RPE/Bruch’s membrane disruption, the follow up OCT showed a choroidal excavation with hyperreflective material filling the trough. The fluorescence angiography revealed multiple hyperfluorescent spots at the posterior pole with a hyperfluoresent foveal lesion corresponding to the area of choroidal excavation. Leakage of fluorescein dye was not evident anymore. The area of foveal hypofluorescence in the ICG showed a significant reduction. No pathological changes were seen in the partner eye.
Conclusion:
Our report presents an unusual case of PIC in a middle aged male patient with a large foveal chorioretinal lesion and absence of the typical multiple small yellowish spots at the posterior pole.

Figure 1: Fundus of the righe eye showing a small yellowish spot inferior to the fovea.
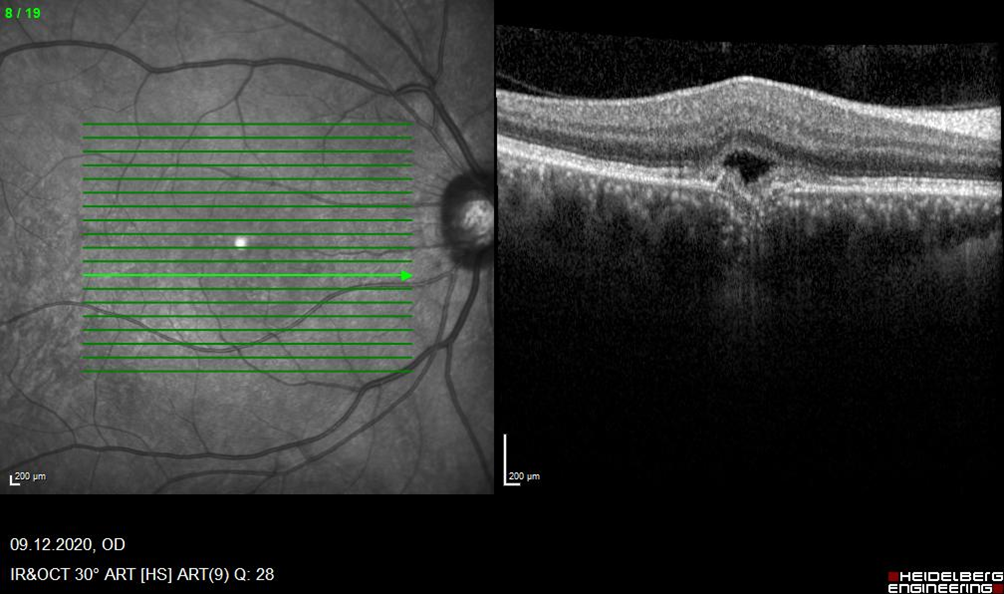
Figure 2a
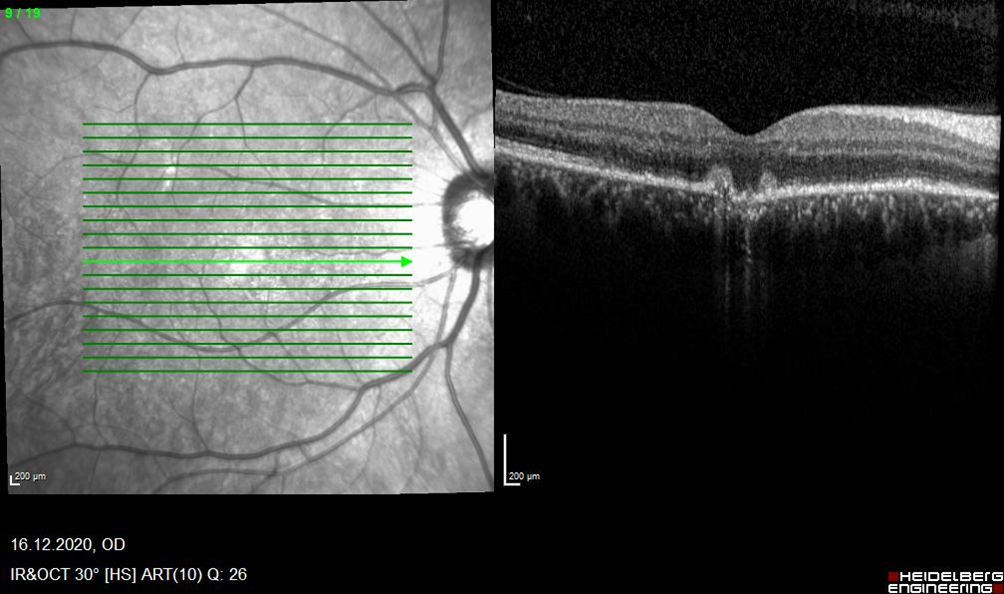
Figure 2b
Figure 2a, 2b: OCT shows neuroepithelial detachment in correspondence with the lesion, with RPE/Bruch membrane interruption.

Figure 3: Fluorescein angiography (FA) performed on 09.12.2020 showing the presence of a hyperfluorescence in the area of the lesion in the later stages of the angiogram in the right eye . Indocyanine green angiography (ICG) shows the presence of a punctiform hyperfluorescence in the area of the lesion, four rounded hypofluorescence in the superior macula.

Figure 4: Fluorescein angiography (FA) performed on 22.01.2021 showing the presence of multiple spot-hyperfluorescences in the in the early stages of the angiogram in the right eye.
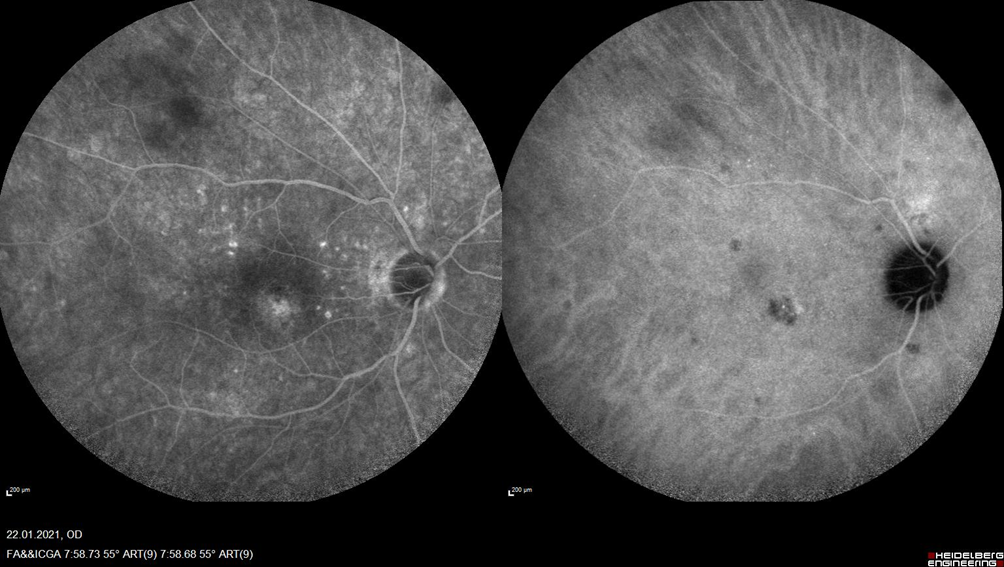
Figure 5: Fluorescein angiography (FA) performed on 22.01.2021 showing the presence of multiple spot-hyperfluorescences also in the later stages of the angiogram in the right eye . Indocyanine green angiography (ICG) shows the presence of a punctiform hyperfluorescence in the area of the lesion and multiple rounded hypofluorescence.
,