Ophthalmology and Vision Care
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Isiaka Oluwasegun Sanni
Benin City, Edo State, Nigeria Doctor of Optometry, University of Benin
Clinical Optometrist at Makkah Specialist Eye Hospital, Bauchi (Al basar International Foundation), Nigeria.
*Corresponding Author: Isiaka Oluwasegun Sanni, Clinical Optometrist at Makkah Specialist Eye Hospital, Bauchi (Al basar International Foundation), Nigeria.
Received: November 17, 2021
Accepted: December 13, 2021
Published: December 27, 2021
Citation: Isiaka Oluwasegun Sanni. (2021) “Subjective Refractions Determined by Dyop® and Snellen Chart as Optotypes”, Ophthalmology and Vision Care, 1(4); DOI: http;//doi.org/11.2021/1.1022
Copyright: © 2021 O. Isiaka Oluwasegun Sanni. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Purpose:
Compare refractive error and visual acuity measurement by Dyop® acuity chart and Snellen chart.
Methods:
Forty subjects aged 24.48 ± 2.01 years with visual acuity better than 6/12 were recruited at University of Benin Optometry Clinic. Refractive error and corrected visual acuity were measured by subjective refraction method with Dyop® acuity chart and Snellen chart. The assessment sequence between the two acuity charts formats was alternated for every other patient to reduce potential refractionist bias. The duration of measurements was compared. Thibo’s notation was used to represent the refractive error findings to enhance easy analysis.
Results:
There was no significant difference in terms of spherical equivalent (M), component J0 and J45 measured by Dyop® acuity chart and Snellen chart (even age and gender consideration) but there was disparity in the mean acuity of about 0.25 diopters with Dyop (1.17 ± 0.14 decimal units) and Snellen chart (1.60 ± 0.21 decimal units). The subjective refraction measurement with Dyop (339 ± 122 seconds) took half the duration for Snellen’s (680 ± 281 seconds).
Introduction
Purpose:
Compare refractive error and visual acuity measurement by Dyop® acuity chart and Snellen chart.
Methods:
Forty subjects aged 24.48 ± 2.01 years with visual acuity better than 6/12 were recruited at University of Benin Optometry Clinic. Refractive error and corrected visual acuity were measured by subjective refraction method with Dyop® acuity chart and Snellen chart. The assessment sequence between the two acuity charts formats was alternated for every other patient to reduce potential refractionist bias. The duration of measurements was compared. Thibo’s notation was used to represent the refractive error findings to enhance easy analysis.
Results:
There was no significant difference in terms of spherical equivalent (M), component J0 and J45 measured by Dyop® acuity chart and Snellen chart (even age and gender consideration) but there was disparity in the mean acuity of about 0.25 diopters with Dyop (1.17 ± 0.14 decimal units) and Snellen chart (1.60 ± 0.21 decimal units). The subjective refraction measurement with Dyop (339 ± 122 seconds) took half the duration for Snellen’s (680 ± 281 seconds).
Conclusions:
Refractive error measured by a Dyop® was comparable with Snellen chart. Dyop® refractive error was twice as efficient, with a narrower variance in visual acuity measurements, compared to the subjective refraction done with Snellen charts as optotype.
Despite the global use of the 1862 Snellen test, it is widely realized that a more efficient method of refractive error and/or visual acuity measurement is needed to enhance better care for vision impaired people, estimated to be 285 million globally [1]. Uncorrected refractive error is the leading cause of vision impairment, estimated 42%, followed by Cataract which amount to 33% of the population with vision impairment [2]. Vision is a dynamic process in which the vibratory motion of the visual saccades refreshes the response of the photoreceptors. That photoreceptor stimulus is sent to the neural ganglia in the inner surface of the retina which functions much as a biological circuit board and allowing the images we see to be dynamic and autonomic [3].
A Dyop® (short for dynamic optotype) is a spinning segmented ring with contrasting (typically Black/White) segments and gaps which provide a strobic stimulus to the photoreceptors. The Dyop® diameter is used as an indicator and visual target for measuring acuity and refractions. It uses dynamic and/or resonance acuity where the motion of the gaps and segments synchronizes with the inherent refresh rate of the photoreceptors (0.33 arc minutes squared per second). That dynamic visual acuity explains the increased precision and reduced variance of a Dyop® refraction versus Snellen refraction. The smallest Dyop® angular arc width diameter where the direction of spin can be detected is the visual acuity and refraction endpoint [3].
The net advantage of Dyop® acuity and refractions is that it is up to six times as precise as Snellen testing, with one-sixth the variance, with about three to four times the efficiency of Snellen testing as to acuity and refraction measurement because of the new Dyop® test algorithm. A Dyop® retains those advantages regardless of the age, culture, or relative lack of literacy of the subject being evaluated. A Dyop® can be used to measure acuity in color, and a Dyop® can be used for measurement of less developed acuity systems such as that of an infant.
The Adult Dyop Test has two identical diameter Dyop® rings near the center of the display with only one ring as spinning. The Children’s Dyop® Test has two peripheral Dyops with only one ring as spinning. The ring diameters are identical, and the visual acuity endpoint is the diameter of the smallest Dyop® ring which was detected as spinning. To detect false positives the subject is asked whether the spinning ring was the left ring or the right ring, or whether that ring was spinning clockwise or counterclockwise.
The Infant Dyop® Test has only ONE peripheral Black segmented Dyop on a White background which alternates its peripheral location as the Dyop® diameter, or spin direction, changes. Because of the preferential tendency for motion detection, the Infant Test and the Children’s Test can both use the motion of the subject’s head and/or eyes to track the far right side or the far left side of the monitor as the peripheral location of the spinning Dyop®.
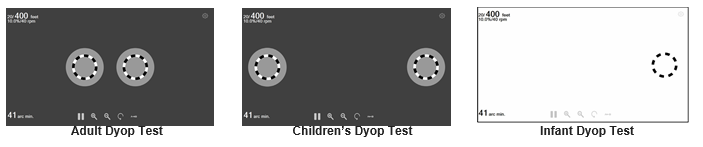
Figure 1: Basic Chart2020 Dyop® for all age categories
Using remote access software such as AnyDesk also allows acuity testing to be done successfully regardless of the differences in the computer operating system or distance between the subject and the examiner. Color acuity testing may also be done to detect the potential for symptoms of dyslexia, migraines, or epilepsy. [3]
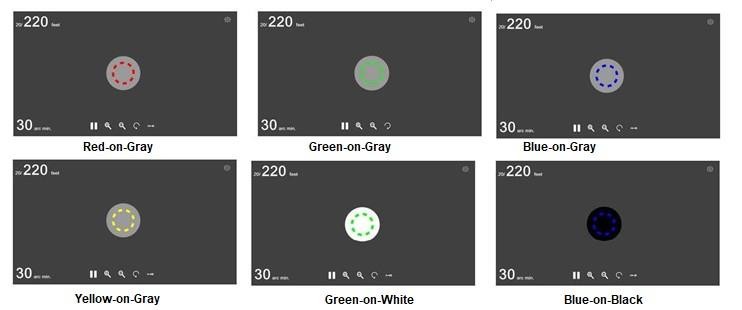
Figure 2: Simplified Chart2020 Dyop® Colors Test on a digital display. [4]
However, in this study, Thibo’s notation [5] (M, J0 and J45) was used to represent the refractive error measured. There was insignificant mean difference in the spherical equivalence (M); 0.01 ± 0.12D: p = 0.77, as well as 0.00 ± 0.03D: p = 0.27, and 0.00 ± 0.01D: p = 0.47 in the cross cylinder (J0 andJ45 respectively). Spectacle or contact lenses are prescribed or dispensed in 0.25D step in optometry practice. Hence, the bias of the refractive error measured with Dyop® and Snellen chart was both statistically and clinically insignificant [6].
On the contrary, visual acuity difference between Dyop® and Snellen chart was 0.43 ± 0.19 decimal units. This represents more than a two-line difference between the two optotypes (p = 0.00) or Dyop® improve level of acuity of 0.25 diopters [6]. This was observed in the study [8] which stated that measuring recognition acuity by reading letters may lead to an overestimation of visual ability and inclusion of top-down cognitive processes that are unavailable for resolution tasks. Because of the consistent Snellen overminus 0.25 diopter disparity versus a Dyop®, refractionists may need to anticipate that inherent Snellen overminus by having patients do a proper binocular balancing to verify the Dyop® acuity measure with enhanced level of visual clarity, legibility and comfortable vision for patients. As literacy and digital sources of literacy became more prevalent in the past 50 years, the slight 0.25 diopter Snellen overminus has become more significant due to the Stiles-Crawford Effect and the habituation towards crisp images [9]. The Snellen overminus may encourage eye elongation and the propagation of myopia. Future research may also indicate that the 0.25 diopter Snellen overminus is a factor in the global epidemic of myopia.
Furthermore, this study also recorded the time of subjective refraction measurement with Dyop® and Snellen chart. The time of measurement with Dyop® (339 ± 122 seconds) was typically half the time of measurement using Snellen chart (680 ± 281 seconds). The subjects had just two possible response options with Dyop® (rotating or not rotating) but had to figure out all the letters (unequal legibility) in a row which increases in number down chart for Snellen as the optotype [7]. With Snellen as the fixation target, the refractionist would assess if the subject responded correctly to each letter seen on the chart and would also need time to obtain the best acuity for the subject by carefully adjusting the lens power combination. However, the refractionist would only adjust the lens power to reach the point that the subject perceived non-rotating target with Dyop® which explains why the endpoint of subjective refraction could be reached faster with Dyop®.[6]
Moreover, to compensate for the selection difference and also maintain credibility of tests, the Dyop®/Snellen sequence of the two comparative tests was alternated with each subject and the tests were conducted by the same investigator. [6]
Conclusively, this study validated the potentials of Dyop® as to subjective refractive measurement (since it is comparable to Snellen’s chart subjective refractive measurement) with greater efficiency, improve level of acuity of 0.25 diopter and narrower variance in visual acuity measurements. [6]