Ophthalmology and Vision Care
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Mona Abdel kader 1*, Ayman Fawzy 2
1Professor in Mansoura Ophthalmic Center, Faculty of Medicine, Mansoura University.
2Lecture in Mansoura Ophthalmic Center, Faculty of Medicine, Mansoura University.
*Corresponding Author: Mona Abdel kader, 1Professor in Mansoura Ophthalmic Center, Faculty of Medicine, Mansoura University.
Received: November 04, 2021
Accepted: November 15, 2021
Published: November 23, 2021
Citation: Mona Abdel kader and Ayman Fawzy. (2021) “Triamacinolone Alone Versus Triamacinolone with Laser in Diabetic Macular Odema”, Ophthalmology and Vision Care, 1(4); DOI: http;//doi.org/11.2021/1.1020.
Copyright: © 2021 O. Mona Abdel kader. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Background:
Macular oedema is responsible for a significant decrease of vision in this population.
Aim of the study is to assess retinal function by multifocal electroretinography (MF-ERG) in eyes with diabetic macular edema (DME) after intravitreal triamcinolone acetonide (IVTA) injection and to compare the effect of IVTA alone and after its combination with argon laser photocoagulation.
Methods:
The study included eighty patients (120 eyes), divided into two groups. Group 1 included sixty eyes (60) of forty patients (40) with DME treated with triamcinolone acetonide injection alone, group 2 (laser group) included another sixty eyes (60) of forty patients (40) with DME treated with triamcinolone acetonide injection followed by argon laser photocoagulation (after 3 week). The response to treatment was monitored functionally by visual acuity measurement and MF-ERG and anatomically by foveal thickness measured by optical coherence tomography (OCT). The changes in functional and morphometric parameters were followed at 1 week and 1, 2, 3,6 months.
Results:
Visual acuity and MF-ERG values increased after intravitreal triamcinolone acetonide injection. There was statistically significant increase in mean P1 amplitude compared with pretreatment. The mean P1 peak latencies were shortener. There were also statistically significant decreases in the mean foveal thickness after treatment. In group 1, there was deterioration of the initial improvement that started after 2 months from IVTA while in group 2, there was more stability of the initial improvement.
Conclusion:
IVTA injection causes transient improvement of macular function and decreases of retinal thickness in diabetic patients. This study suggests the combination of IVTA, and argon laser photocoagulation causes more permanent improvement. Argon laser photocoagulation effectively maintains improvement occurring after IVTA and reduces recurrent DME after IVTA.
Introduction:
Macular oedema affects approximately 29% of diabetic patients with disease duration of 20 years or more and is responsible for a significant decrease of vision in this population. [1]
The Early Treatment Diabetic Retinopathy Study (ETDRS) demonstrated a significant benefit of focal laser photocoagulation for the treatment of clinically significant macular oedema. [2] However, eyes with diffuse diabetic macular edema carry a particularly poor prognosis despite laser photocoagulation. In the ETDRS, only 17% of the eyes had an improvement of visual acuity (V.A) and less than 3% had a visual improvement of [3] or more ETDRS lines.2 Laser photocoagulation is at best supportive rather than curative [2-3], prompting interest for alternative therapeutic approaches.
Intravitreal administration of triamcinolone acetonide has provided the ophthalmologist with an extra tool for the treatment of eyes with diabetic oedema. [4-5]
Triamcinolone acetonide, has been proposed to decrease macular oedema6, the probable mechanisms are increase in tight-junction protein, which diminish vessel leakage by a local vasoconstrictive effect, [7-8] and angiostatic properties through inhibition of vascular endothelial growth factor (VEGF).[9]
IVTA is reported to generate favorable results in the treatment of DME, however the chief limitation of IVTA is the recurrence of DME which develops after a relatively short duration of action. Although repeated administration of IVTA might be an option. Yet, repeated IVTA may potentiate the toxicity of the intraocular corticoid as elevation of intraocular pressure [10], cataractogensis [11] and endophthalmitis.[12]
The aims of this study are to assess macular function by MF-ERG and foveal thickness in eyes with diabetic macular oedema after IVTA injection and to determine whether macular argon laser photocoagulation after IVTA might be helpful in the maintenance of improvement after IVTA or not.
Patients and Methods:
This study was carried out on patients attending the outpatient's clinic of Mansoura Ophthalmic Center during the period from December 2012 to February 2014. This study included one hundred and twenty eyes of eighty patients with diabetic macular edema with no sign of vitreo-macular traction on either biomicroscopy or Optical Coherence Tomography (OCT). The patients were divided into two groups :Group 1 included sixty eyes (60) of forty patients (40) with DME treated with triamcinolone acetonide injection alone, group 2 (laser group) included another sixty eyes (60) of forty patients (40) with DME treated with triamcinolone acetonide injection followed by argon laser photocoagulation (after 3 week).The determination of group for the individual was randomized (dependent on last digit of hospital ID number .If it was an even number the patient was located in group 1, if it was an odd number ,the patient was allocated into group 2.
Macular oedema was defined by a zone or zones of retinal thickening one disc area or larger at any part within one disc diameter of the center of the macula on biomicroscopy and, by diffuse fluorescein leakage involving most of the macular area on fluoresein angiography or/ and areas of pooling of flourscein dye within two disc diameters at the center of the macula in cystoid macular edema.[13] Another criterion involved significant reduction in the reflectivity of the outer layer and/ or subfoveal collection on OCT or cavities of low reflectivity in posterior retinal layers or full retinal thickness with tiny walls in cystoid macular edema.[13] Central macular thickness had to be more than 300µm(normal 170±18µm).[13] Patients were thoroughly informed about the injection procedure, postoperative results and possible complications and written consents were taken from all patients. All tests were carried out in accordance with the tenets of the Declaration Of Helsinki(1989) of the world medical association. The study was approved by Mansoura University Hospital trust ethics committee
Exclusion Criteria: it included patients who previously received intravitreal injection either triamcinolone or bevacizumab, those with evidence of macular ischaemia, epiretinal membranes or vitreo-retinal traction, patients with past or current history of glaucoma. patients who had undergone cataract surgery or vitre-retinal surgery and patients with renal insufficiency. other ophthalmic disorders associated with macular oedema, such as uveitis and branch or central retinal vein occlusion
Pre-Injection Evaluation:
Medical history (with special stress on age of onset of diabetes mellitus (DM), condition of metabolic control and presence of associated systemic complication related to DM such as hypertension and renal impairment).
Ophthalmological examination included: best corrected visual acuity (BCVA) determined using Snellen charts in a standardized fashion ,best corrected visual acuity were transformed to logarithmic scale ( log MAR:logarithm of the minimum angle of result), pupillary reaction (direct and consensual), slit lamp examination (with special focus on: presence of any corneal opacities that may affect vision, presence of any lens opacities, intraocular pressure (IOP)(it was measured by slit lamp mounted Goldmann's applanation tonometry), fundus biomicroscopy ( it was done after maximum pupillary dilation by tropicamide 1% and phenylepherine 2.5% using both slit lamp biomicroscopy with non-contact (+90D) Volk lens and Goldman contact lens in order to detect diffuse macular oedema, to evaluate vitreo-retinal interface relationship, to check any pre-retinal membranes and previous macular laser treatment), fundus photography, fundus fluorescein angiography to confirm macular leakage, optical coherence tomography (OCT) to confirm macular thickening, assess vitreoretinal relationship and demonstrate cystoid spaces and multifocal electro-retinagram MF-ERG to assess macular function.
MFERG:
All ERG data were recorded using (Roland Consult, Brandenburg, Germany). Stimulation and recording of MF-ERG responses were performed using the ISCEV guidelines. [6] The stimulus, consisting of (61) hexagons covering a visual field of 30o was presented at a frame rate of 75Hz on a monitor 30cm from the patient’s eye. The luminance (97%) of each hexagon independently alternated between black and white. The amplifier gain was set at 100,000, the lower cutoff frequency
were 5 Hz and the upper frequency being 100 Hz. After maximum dilation of the pupil, Dawson Trick litskow (DTL) electrode were applied to topically anaesthetized cornea with one ground electrode in the forehead and two temporal reference electrodes and the opposite eye occluded. The
Eyes were optically corrected for near vision in order to see clearly the small fixation spot in the center of the stimulus matrix. and the patients were instructed to fixate at the intersection of the spokes. The recording period was comprised of eight segments of 30 second, providing a total recording time of 4minute. The quality of the recording was controlled by real-time display and contaminated segments were discarded & repeated
The MF-ERG stimulus location and anatomical areas corresponded roughly to the following: ring 1 to fovea, ring 2 to the parafovea, ring 3 to perifovea, ring 4 to the near periphery and ring 5 to central part of the middle periphery.[11]
The response density (amplitude per unit of retinal area (nv/deg2) of each local response and latency were estimated over central ring and four quadrants.
OCT:
OCT was performed on every patient using (Topcon, three dimensional (3D) OCT, -1000, -USA). After dilation of the pupil. Central retinal characteristics were analyzed by optical coherence tomography utilizing 6 radial line scans (6mm) directed on the fovea as determined by simultaneous evaluation of the red-free image on the computer monitor of the OCT scanner. The retinal thickness of the 1mm central retina was obtained using the macular thickness map for calculation
Triamcinolone Acetonide Injection:
For IVTA injection, topical 1% Benoxinate was applied to the ocular surface followed by preparation with 5 % povidone Iodine. triamcinolone acetonide (40 mg/ml, 1 ml/both) was drawn into lcc tuberculin syringe after cleaning the top of the bottle with an alcohol wipe. The needle was placed in an upright position to allow the triamcinolone powder to precipitate. The supernatant fluid was then discarded. A separate 27- or 26-gauge needle was placed on to the syringe, which was then inverted to remove the air bubbles. The excess triamcinolone was discarded till 0.1 ml (4 mg) remained in the syring.
The injection was set to inferior pars-plana to avoid drug deposition in front of the visual axis. The stab was 4mm from the limbus. The bevel of the needle was directed anteriorly (with the needle aimed posteriorly and slightly inferiorly) to avoid direct injection over the macula using a single continuous maneuver, the chemical was injected into the eye. The needle was removed simultaneously with the application of a cotton-tipped applicator over its entry site to prevent regurgitation of the injected material. Indirect ophthalmoscopy was used to confirm proper intravitreal localization of the suspension, perfusion of the optic nerve head and central retinal artery (CRA) pulsation, paracentesis was performed if CRA pulsation was present or if the globe felt very tense.
Patients were asked to sit up immediately after injection and continue maintaining an erect posture for the next six hours at least. This was to ensure that drug assumes a dependant position and does not collect over the macula which would cause a transient visual loss. Patients were given a course of topical antibiotics for 1 week.
Macular Argon Laser Photocoagulation:
Macular grid laser photocoagulation was applied 3 weeks after undergoing IVTA in group 2 only. Patients received laser according to ETDRS guide lines.2 All treatment were performed under topical anesthesia with fundus contact lens .Test laser spots were applied in the macular area at a distance of one to two spots from one to another in concentric lines near vascular arcade with argon green ,a duration of 0.2-0.5 second ,diameter of 100 to 200 µ and power increased from 75mv to produce mild gray burn. Based on the finding of fluorescein and OCT, prior IVTA, the grid pattern of macular laser on areas of capillary non perfusion and retinal thickening ,About 50 laser spot were applied to parafoveal region up to the edge of the foveal avascular zone. Direct photocoagulation was applied only to areas in which focally leaking micro aneurysms were observed.
Post-Injection Follows Up:
Follow up was scheduled 1 week, 1 month, 2 month ,3 months and 6 months and included: BCVA, slit lamp examination with special attention to (presence of complicated cataract, IOP), fundus biomicroscopy (to determine the presence of any post-injection complication), flourescein angiography , OCT and MF-ERG were done after intravitreal injection
Outcome Measures:
Primary outcomes were monitored anatomically by OCT macular thickness and functionally by visual acuity assessment and MF-ERG. Secondary outcomes were potential corticosteroids and injection related complication (IOP elevation, endophthalmitis, cataract and vitreous hemorrhage).
Injection success was judged by: improvement of macular thickening on biomicroscopy, reduction of diffuse leakage on fluorescein angiography, improvement of BCVA, reduction of macular thickness by OCT and improvement of macular function by MF-ERG (tables 1-4, figures 1-4).
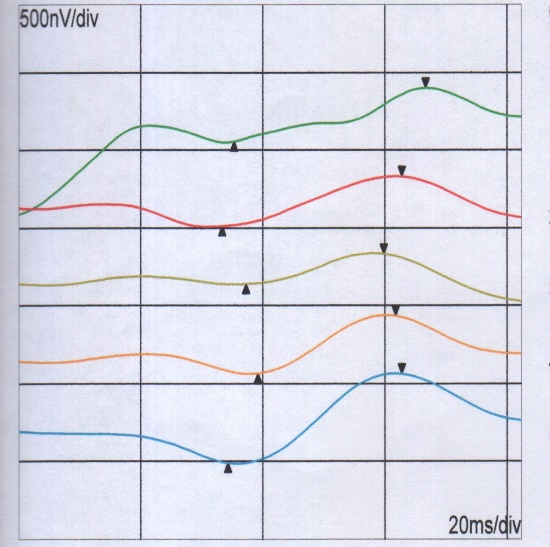
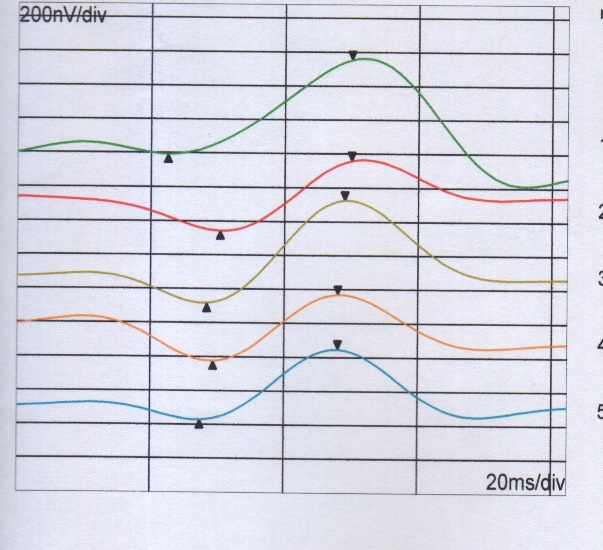
Figure 1:MF-ERG over rings before& after IVTA, before IVTA, there is delay in latency and reduction in amplitude, after IVTA, there is increase in amplitude and reduction in latency.

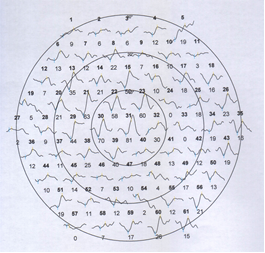
Figure2: MF-ERG trace array,before injection there is irregular curve, just irregular line ,no apparent peak and trough ,after injection ,appearance of the peak and trough of the curve.
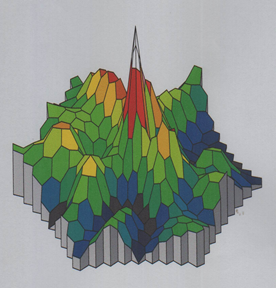
Figure 3: Three-dimensional MF-ERG
, Before IVTA, there is depression of foveal peak and after IVTA, there is increase and appearance of the foveal peak .
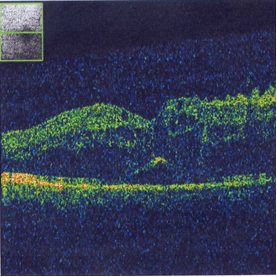

Figure4: OCT before and after IVTA, Before injection, there is increase in retinal thickness, after injection ,there is reduction of retinal thickness.
|
P |
Group 2 Number of patients |
Group 1 Number of patients |
|
|
0. 1 |
57± 9years |
55±11years |
Age |
|
0.2 |
23 |
22 |
Gender female |
|
0.5 |
17 |
18 |
male |
|
0.55 |
6 |
5 |
Hypertension |
|
0.11 |
1 |
2 |
Renal impairments |
|
0. 1 |
12.4±0.35 mmHg |
12±0.9mmHg |
IOP |
|
0.18 |
18 |
16 |
Type of diabetes type 1 |
|
0.16 |
22 |
24 |
Type2 |
|
0.11 |
20 |
22 |
HB A |
|
0.15 |
20 |
18 |
B |
|
0. 1 |
0. 96± 0.4 |
0.95±0.3 |
Visual acuity at enrollment |
|
|
|
|
|
Table1: Characteristics of groups
|
P |
Group 2 |
Group 1 |
Time of visual acuity |
|
0. 1 |
0. 96± 0.4 |
0.95±0.3 |
Before IVTA |
|
0.2 |
0.77 ±0.31 |
0.75±.34 |
After 1week |
|
0.5 |
0.76±0.33 |
0.75.5±0.5 |
After 1month |
|
0.05 |
0.75±0.2 |
0.93±0.31 |
After 2months |
|
0.01 |
0.74±0.41 |
0.95±0.5 |
After 3months |
|
0.001 |
0.74±0.35 |
0.99±0.9 |
After 6months |
Table 2: Comparsion of log MAR visual acuity between groups
|
P |
Group 2 |
Group 1 |
Time of OCT Changes |
|
0. 5 |
541± 150 |
528±170 |
Before IVTA |
|
0.44 |
250±110 |
240±100 |
After 1week |
|
0.5 |
248±108 |
239±105 |
After 1month |
|
0.01 |
260±110 |
270±107 |
After 2months |
|
0.02 |
270±99 |
302±120 |
After 3months |
|
0.001 |
285±90 |
420±130 |
After 6months |
OCT changes in groupsTable 3:
|
P |
Group 2 |
Group 1 |
MF-ERG parameters |
|
0. 1 0.8 |
28.7±6.1 69 ± 2 |
25.4 ± 5.5 70 ± 2.4 |
Before IVTA P1amplitude(nv/deg2) P1 latency(ms) |
|
0.2 0.6 |
47 ± 3.1 56±4.6 |
45.3±6.4 57±4.5 |
After 1week P1amplitude(nv/deg2) P1 latency(ms)
|
|
0.5 0.8 |
51±3.1 56±4.4 |
50±2.1 55±3.6 |
After 1 month P1amplitude(nv/deg2) P1 latency(ms)
|
|
0.1 0.3 |
48.8±2.7 56±4.1 |
49±2.5 55±3.7 |
After 2 months P1 amplitude(nv/deg2) P1 latency(ms)
|
|
0.02 0.01 |
48±3.5 55±5.1 |
40±5.1 60±6.4 |
After 3 months P1amplitude(nv/deg2) P1 latency(ms)
|
|
0.005 0.003 |
47±4.1 55.5±3.1 |
30±3.3 65±5.1 |
After 6 months P1 amplitude(nv/deg2) P1 latency(ms)
|
|
|
0.004 |
0.001 |
P |
Table 4: MF-ERG parameters before and after IVTA over central ring
Statistical Analysis:
Repeated measures analysis of variance (ANOVA) was used to compare mean values and to analyze mean retinal thickness, BCVA (best corrected visual acuity), intra ocular pressure (IOP) and MF-ERG parameters (P1 amplitude and P1 latency) .Values of the two groups at each measurement were compared by ANOVA. In each group, values before and after treatment were compared by ANOVA. Spearman's correlation coefficient was used to calculate correlation between variables P < 0.05 statistically significant, R ≥ 0.5 good correlation, R< 0.5weak correlation.
Results:
The study included one hundred and twenty eyes of eighty patients, forty patients were bilaterally studied (50%) and forty patients were unilaterally studied (50 %). Forty five (45) patients were female (56%) and thirty five (35) patients were male (44%). All procedures were carried out in accordance with the tenets of the Declaration of Helsinki (1989) of the world medical association. The study was approved by Mansoura University Hospital Trust Ethics Committee.
The patients aged from forty (40) years up to sixty – five (65) years with a mean age fifty (50) years. Most of them suffered from type II diabetes (46 patients (57.5%) with mean duration of the disease 10 years (SD±3) (table 1)
Fifty eyes suffered from diffuse maculopathy, fifty eyes suffered from cystoid maculopathy and twenty eyes suffered from mixed maculopathy. Macular edema has been present for 6 month(8±2months) All patients were treated with intra-vitreal injection of 4 mg. triamcinolone acetonide using the same technique. Among (120) eyes: sixteen eyes (13.3%) had marked improvement in visual acuity (3 lines in landolt chart ), 32 eyes (26.6 %) had moderate improvement (2 lines), 60 eyes (50 %) had mild improvement in visual acuity (one line in londolt chart ) and 12 eyes (10 %) had no improvement in visual acuity after one week. The improvement noticed in the first six months is included in table 2.
By OCT studying (table 3,fig 4) ,the study revealed marked improvement ( more than 120 μm ) in 20 eyes (16.6 % )with macular edema depending on the retinal thickness measured from the retinal surface to the retinal pigment epithelium before and after treatment as central retnial thickness ( before treatment ) ranged from 550 micron (μm) to 700 μm with mean thickness 570 μm ±SD 90 μm reduced into mean thickness 400 μm ±SD 50 μm after treatment with mean reduction ( 170 μm ), 36 eyes ( 30 % ) with moderate reduction as central thickness ranged from 450 μm to 350 μm before treatment with mean thickness was 400 μm reduced into mean thickness was 300 μm with mean reduction was 100 μm after treatment , 48 eyes ( 46.6 %) with mild reduction as retinal thickness ranged from 350 to 305 μm with mean thickness was 300 μm reduced into mean thickness 255 μm with mean reduction 45 μm and eight eyes had no improvement after treatment .Although macular thickness was significantly reduced ,values were higher than normal (<200) after injection .This was probably due to chronic edema and high baseline values.
There was good correlation between retinal thickness and visual acuity (R=-5.00, P=0.01). The reduction in retinal thickness was associated with improvement of visual acuity
Flourescein Angiography showed leakage from macular area in all cases before IVTA. After IVIA, there was reduction of the macular leakage in most of the cases (116 eyes) (96.6 %)
The retinal response density of MF-ERG in affected eyes before treatment ranged from 15 nv/deg2 to 2 nv/deg2 (mean value ± SD 7.4 ±5.5 nv/deg). After treatment, the response density ranged from 22 to 17 (mean value ±SD 15.3 ± 6.4). Table 4 (Fig.1-3)
The latency of MF-ERG in eyes before treatment ranged from 70 millisecond (ms ) to 59 ms ( mean value ±SD 65 ±2 ms)
After treatment the latency ranged from 54 to 58 ms (mean ± SD 55± 3.1 ms )
There was good correlation between increased amplitude of MF-ERG and decreased macular thickness by OCT ( R=0.54 , P=0.008 )
The IVTA effect (OCT improvement, MFERG changes and visual acuity improvement) regressed 2 months after injection in group 1 while in group 2, there were more stabilization of improvement.
Post-Treatment Complication:
Intra-ocular pressure: The mean pre-injection IOP was 15 ± 2.2.
The mean post injection IOP was 17 ±3.5 . There was only four cases (3.3%) develop mild increase in IOP (It was 26 mm Hg) and was controlled with B-blocker
Minor local adverse events related to the treatment procedure (conjunctiva hyperemia and subconjuctival haemorrhage) were presented in 6 cases only (5% ) during the first week
Lens status: The lens was clear in all patient before treatment. At the end of follow up, none of the eyes displayed any cataract.
There were no cases of endophthalmitis, clinically evident inflammation, retinal tear, retinal detachment or thrombi embolic .
Discussion:
Diabetic macular edema is a major complication of diabetic retinopathy that faces a challenge in its management . Although several treatment modalities have been tried for the management of diabetic macular edema ,these modalities have many limitations . Focal and grid laser photocoagulation have remained the primary treatment option for diabetic macular edema for several years . However most eyes treated with laser photocoagulation do not have an improvement in visual acuity . Although ETDRs,[2] demonstrated that immediate focal photocoagulation reduced moderate visual loss by 50%, 12% of treated eyes still lost vision at the 3-year follow up interval and 24%of immediately treated eyes had thickening involving the center of the macula at 36 months .In addition , laser treatment of eyes with diffuse macular edema has been disappointing .[15,16]
In the past years, attempts to understand the pathogenesis of diabetic retinopathy had led to other strategies in the management of diabetic macular edema . The development of diabetic retinopathy is a multifactorial process. Much of retinal damage that characterizes the disease is now understood to result from retinal vascular leakage and non perfusion mediated by numerous growth factors.[17,18] The up regulation of growth factors is associated with breakdown of the blood – retinal barrier with increased vascular permeability resulting in retinal oedema, stimulation of endothelial cell growth and neovasculization.[19]
For years, corticosteroids have been used in ophthalmology to suppress intraocular inflammation and reduce leakage from retinal blood vessels . Local application of cortisone was used to decrease the adverse side effects of systemic cortisone and at the same time achieve a higher concentration at the site of action . The use of intraocular corticosteroids for diabetic macular oedema started after the significant observations of McCuen et al , [20] and Young et al, [21] on the lack of toxicity of intra-vitreal triamcinolaone (9-fluoro – 16 – hydroxyl prednisolone ) . Subsequently , there have been several studies documenting the antiangiogenic , anti proliferative and antiedematous effects of IVTA. The landmark study by Martidis et al [22] involved sixteen eyes with clinically significant macular oedema that failed to respond to at least two previous sessions of laser photocoagulation at least 6 months after laser therapy, the response was measured by clinical examination and OCT. Eyes with residual central macular thickness more than 300 µm. were administered an intravitreal injection of 4mg in 0.1 ml of trimacinolone acetonide. The central macular thickness deceased after injection by 55%, 57% after lst and 3rd month respectively as measured by OCT. Aurder et al 27 characterized the pharmacodynamic profile of the IVTA on macular thickness as 3-phase curve (fast decrease , steady state and a relapse) The maximum effect duration was 140 day. [23] Massin et al. too, [24] have found transient improvement of macular thickness that necessitate repeated injection However, Jonas et al,21 have found an impressive improvement in visual acuity after IVTA injection. but 25 mg of the drug was used. There was significant transient increase in the intraocular pressure. [25]
In this study, there was decrease in retinal thickness with improvement of visual acuity after IVTA for 2 months. Then begin to relapse in group 1 . There was improvement in retinal function after IVTA after one week that continued to improve for 1month then begin to decrease after 2 month in group 1. There was increase in the amplitude of P1 wave and decrease in latency of P1 wave for 2 months. The visual benefit of argon laser photocoagulation subsequent to IVTA for DME became apparent months afterwards .In contrast to IVTA only ,this combination therapy appears to maintain reduced central macular thickness at least for 6 months follow up .Central macular thickness was minimal and visual acuity was improved at examination performed 1week and 1month after IVTA.
The exact mechanism underlying the maintenance of improved vision, increase MFERG amplitude and decreased central macular thickness due to grid laser photocoagulation was not identified, but several factors may be involved. First, decreased foveal thickness after IVTA may enhance the effects of grid laser photocoagulation. Without IVTA, markedly increased foveal thickness, subfoveal fluid and retinal opacity due to edema might interfere with adequate laser burning of the retinal pigment epithelium and photoreceptor layers. However, after IVTA, decreased foveal thickness and restoration of retinal transparency achieved by the treatment would facilitate the delivery of the laser energy selectively to retinal pigment epithelium and photoreceptor layers. Second, the possibility exists that steroid might act beneficially in the process of mature laser scar formation. It has been established that 2 or 3 weeks should elapse for the formation of mature laser scar and laser treatment itself frequently induces aggravation of macular edema or inflammation during this period .The presence of intravitreal steroids might exert certain protective effects against the initial deleterious events that follow grid laser treatment and might also modulate retinal pigment epithelium remodeling after laser photocoagulation.
Karacorlu et al, found significant increase in mean P1, response amplitude at all examinations compared with pretreatment. The mean p1, peak latencies were shorter.[22]
Similarily, Koutsandrea et al, observed increase in MF-ERG amplitude after triamcinolone acetonide injections.[28]
The interval 3 weeks for the separation of laser photocoagulation was chosen because therapeutic effects of IVTA were found to reach maximum values in most cases.[24]
The rational for the use of corticosteroids in the treatment of diabetic macular edema follows from the observation that the breakdown of the blood retinal barrier leads to the edeme and is in past mediated by vascular endothelial growth factor VEGF[23]. Corticosteroids have been shown to inhibit (VEGF), other cytokines and other growth factors, thereby regulating endothelial cell tight Junctions. In addition, corticosteroids inhibit prostaglandin and leukotriene synthesis, which results in local reduction of inflammatory mediators. The resultant anti-inflammatory effect contributes to the reduction of oedema.[24] Increased diffusion by modulation of calcium channels could also account for the efficacy of the corticosteroids in reducing macular edema. [25] The two main complication of IVTA are the intra ocular pressure rise and the development of cataract furthermore, the effects of intravitreal injections are short lasting requiring repeated injections which would further increase the risk of complications. It sounds prudent to think that this treatment modality could replace or complement focal/grid laser photo coagulation Further -more focal grid laser photo coagulation could be used to consolidate the results obtained with one intravitreal injection and decrease the need for re-injection. [26]
There was inverse significant correlation between central macular thickness and visual acuity.
In this study, the incidence of complications between the two groups were similar and there were only four eyes (2 in group 1, 2 in group 2) that had increased intra ocular pressure after IVTA within one week . The rates were consistent with previous studies. [10,29]
Thus, the all complications appeared to be attributable to IVTA and laser photocoagulation appears not to cause significant additional complications.
Also, Martidis, et al, [4] and sutler et al [5] found significant increase in intra-ocular pressure after IVTA. [4,5] Similarly, paccola, et al, [29] observed significant IOP increase from baseline at 4 weeks after IVTA.
In summary, the results seen in this study after IVTA are encouraging. IVTA resulted in statistically significant improvement of best corrected visual acuity, central macular thickness and macular function with little complication (mild increase in IOP that controlled with B-blocker, transient conjunctival hyperemia and subconjuctival haemorrhage)
Conflict of Interest: None