Ophthalmology and Vision Care
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
AL Hashmi K 1*, Mahin Erum 2, Al Hatmi S 3, De Silva S 4, Al Hajri 5, Al Seidi R 6
1Consultant hematologist-Oncologist, Hematology division, Department of Medicine, Armed Forces Hospital (AFH), Al Khoud, Muscat, Oman.
2Medical officer, Acute Medicine Division, Department of Medicine, Armed Forces Hospital (AFH), Al Khoud, Muscat, Oman.
3Senior Specialist neurologist Neurology division, Department of Medicine, Armed ForcesHospital (AFH), Al Khoud, Muscat, Oman.
4Registrar, Acute Medicine Division, Department of Medicine, Armed Forces Hospital (AFH), Al Khoud, Muscat, Oman.
5Senior consultant radiation Oncology, Oncology Center Royal Hospital, Muscat, Oman.
6Senior consultant ophthalmologist, department of ophthalmology, Armed Forces Hospital (AFH), Al Khoud, Muscat, Oman.
*Corresponding Author: Khalid Al Hashmi, Consultant hematologist-Oncologist, Hematology division, Department of Medicine, Armed Forces Hospital (AFH), Al Khoud, Muscat, Oman.
Received: May 26, 2021
Accepted: June 10, 2021
Published: June 12, 2021
Citation: AL Hashmi K, Mahin Erum, Al Hatmi S, De Silva S, Al Hajri. (2021) “Catastrophic Radiotherapy-Induced Bilateral Optic Neuropathy One Year after Radiation”, Ophthalmology and Vision Care, 1(3); DOI: http;//doi.org/05.2021/1.1012.
Copyright: © 2021 Khalid Al Hashmi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited
We describe a case of age 57-year-old woman with a history of adenosquamous lung cancer with brain metastasis who had previously underwent successful radiotherapy for brain metastasis. One year after radiotherapy, while on maintenance chemotherapy, she presented with severe rapidly progressive visual impairment, which started in the right eye and followed shortly by visual loss in the left eye. Initially she was given high dose of dexamethasone. Despite the therapy, her vision rapidly worsened until light was no longer perceptible. The clinical evidence was confirmed by the rapid progression of the Magnetic Resonance Imaging (MRI), which showed homogeneous enhancement of the chiasm and optic nerves. Based on these findings, and exclusion of other possible etiologies (e.g., infectious, paraneoplastic, metabolic and nutritional) radiation-induced optic neuropathy was diagnosed. The purpose of the case report is to report an unusual presentation of optic neuropathy induced by intra-cranial radiation and discuss the clinical approach to acute progressive visual loss.
Introduction
Radiation is frequently used in the treatment of intracranial tumors, and a small percentage of patients develop vision loss as a consequence of injury to the anterior visual pathway [1, 2]. Radiation-induced optic neuropathy (RION) is a rare complication after radiation therapy in which exposure of the anterior visual pathway to radiation results in acute, painless vision loss in one or both eyes months to years after treatment [3]. RION occurs commonly between 10-20 months, with an average of 18 months after treatment; but the onset may range from three months to 9 years and the onset may be acute and characterized by the progressive loss of vision in one or both eyes [4].
Fewer previous descriptive case reports, case series, and reviews published in the past. In one series of 219 patients who received radiotherapy for carcinomas of the nasal or paranasal region, retinopathy occurred in seven, optic neuropathy with blindness in eight, and chiasm damage with bilateral visual impairment in one [5]. Another series described potentially predisposing factors for RION according to possible pathogenic mechanism [6]. We report a patient who developed RION and detailed clinical pathway to evaluate a patient with rapidly progressive bilateral visual loss.
Case Report
A 57-year-old woman, nonsmoker, with a past history of hypertension and dilated cardiomyopathy with ejection fraction of 40%. she presented to us with right hemiparesis, further workup showed she has multiple brain metastasis. MRI brain showed multiple left cerebellar and bilateral (predominantly left) cerebral ring enhancing lesions, figure (A), and pan CT scan showed a left lower lobe apical segment lung mass, biopsy of the lung mass showed adeno-squamous lung carcinoma of the lung (EGFR mutation - wild type, ALK, ROS1: Negative, PO-L1: less than 1%)
She received Whole brain Radiotherapy (WBRT) to a total dose of 2000 cGy in five fractions daily, followed by six cycles of systemic chemotherapy (bevacizumab, carboplatin and pemetrexed). Subsequently, her neurological finding of stroke (aphasia, right side weakness and upper facial nerve palsy) recovered to almost normal. Repeat MRI brain showed significant disease regression, no evidence of enhancing brain lesion and no infraorbital lesion Figure (B). She was started on maintenance chemotherapy with bevacizumab and pemetrexed as per protocol.
She presented one year after completion of the WBRT with gradual painless progressive vision loss. Right eye, on examination her visual acuity was 6/18 and on left eye 6/36, with fundoscopy normal. Vision loss was attributed to cataract at that time.
After one month she presented with worsening vision loss in the right eye for four weeks and left eye for two weeks. At that time there was absence of light perception in both eyes and fundoscopy showed bilateral optic disc atrophy without evidence of retinopathy. Her The intraocular pressures were normal bilaterally, the rest of neurological examination was normal. She received 40mg of intravenous dexamethasone for one week with tapering dose, but there was no improvement in her vision. She was evaluated for reversible causes of optic neuropathy including infiltrative (e.g., sarcoidosis), demyelinating, ischemic, toxic, nutritional, infectious, systemic, autoimmune, and paraneoplastic disorders. Unfortunately, the patient and her relatives refused LP for CSF tests. Repeat Brain and orbit MRI angiography with contrast demonstrated gadolinium enhancement of bilateral intracranial optic nerves without intracranial tumor progression nor vascular compressing lesion. Visual evoked potential showed abnormal signals suggestive of optic atrophy. All the serological workups came as negative including vitamin B12, folate, vitamin D, ESR, ANA, dsDNA, ANCA, TFT, HIV, syphilis, Lyme disease serology, anticrmps, antienolase, antipca2, antirecoverin antibody.
Considering the clinical context, MRI findings and with exclusion of other potential causes of optic neuropathy (ON) the diagnosed with radiation induced optic neuropathy (RION) was established. Unfortunately, she progressed to complete bilateral visual loss within one month without any recovery on OPD follow up.
She was followed up 5 months post diagnosis, without no improvement in vision. She lost interest to receive any further treatment for her cancer.
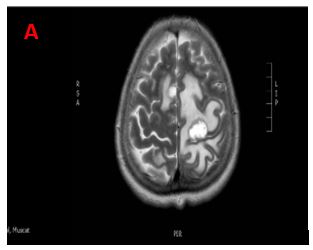
Figure A: brain metastasis before radiotherapy
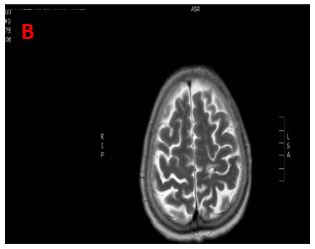
Figure B: Regression of brain metastasis after radiotherapy
Discussion
Radiation optic neuropathy (RON) typically characterized by sudden and irreversible unilateral or bilateral profound vision loss which is a late complication of radiotherapy to the anterior visual pathway [7]. It is thought to be a result of radiation necrosis of the anterior visual pathway. Radiation doses from 5,000–6,000 cGy may produce RION with a risk of up to 5% within 10 years [8]. Most RION however, will present within 3 years of radiation treatment with a peak incidence after 1.5 years. Most significant risk factors include the dose of radiation, proximity of radiation therapy to the optic apparatus. Other factors such as time between doses, and a patient’s age can influence RION incidence and severity [9]. RION is a diagnosis of exclusion. Other causes such as compression, infiltrative optic neuropathy, metastasis to meninges (meningeal carcinomatosis), toxic optic neuropathy secondary to chemotherapy, an immune response to the neoplasm (paraneoplastic optic neuropathy), or inflammation of the arachnoid (arachnoiditis) should be ruled out. Gadolinium-DTPA-enhanced Magnetic Resonance Imaging is considered procedure of choice in evaluating radiation induced optic neuropathy. Orbital cut MRI will display enhancement of a discrete segment of the intracranial prechiasmatic optic nerve, often with accompanying expansion and T2 hyperintensity. In various reported cases enhancements can precede clinical symptoms [10,11] Electrophysiological studies such as visual evoked potential can be helpful in earlier diagnosis of RION before the settlement of visual symptoms. Treatment with systemic corticosteroids and anticoagulation with heparin or warfarin have unfortunately not been proven successful for RION. Hyperbaric oxygen therapy (HOT) is thought to allow for angiogenesis and cease ischemic necrosis [12, 13].
Results of treatment of RION have been disappointing and there is no definitive treatment available. Therefore, in absence of clinical guidelines, current best option is prevention by adhering to published dose tolerance limits for optic apparatus.
Prognosis is usually poor, as the eye affected with RION will have a visual acuity < 20/200 to light perception in 45% of eyes. As the most extreme consequence, there is potential for permanent blindness either unilaterally or bilaterally.
Conclusion
This case further delineates the profile of RION. Visual loss is often acute, profound, and monocular but may decline slowly after acute onset and later affect both optic nerves. Prompt and detailed evaluation to exclude potential reversible causes should be considered prior to final diagnosis of radiation induced optic neuropathy.
Unfortunately our patient didn’t show any response to high dose of intravenous steroid despite immediate administration of treatment. Novel therapies should have randomized trial in large study group before implementing in practice.