Ophthalmology and Vision Care
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Neena.R 1*, Gayathri.M.S 2,Nimmy Prakash3 and Anantharaman Giridhar4
1Senior Consultant, Paediatric Ophthalmology, Strabismus & Neuro-ophthalmology, Giridhar Eye Institute, Kadavanthara, Kochi, Kerala, India-682020.
2Intern in Optometry, Giridhar Eye Institute, Kadavanthara, Kochi, Kerala, India-682020.
3Biostatistician, Giridhar Eye Institute, Kadavanthara, Kochi, Kerala, India-682020.
4Medical Director, Giridhar Eye Institute, Kadavanthara, Kochi, Kerala, India-682020
*Corresponding Author: Neena.R, Senior Consultant, Paediatric Ophthalmology, Strabismus & Neuro-ophthalmology, Giridhar Eye Institute, Kadavanthara, Kochi, Kerala, India-682020.
Received: June 02, 2021
Accepted: June 07, 2021
Published: June 14, 2021
Citation: Neena.R , Gayathri.M.S ,Prakash.N and Giridhar.A. (2021) “Impact of Online Classes on Eye Health of Children and Young Adults in the Setting of Covid-19 Pandemic: A Survey Based Analysis”, Ophthalmology and Vision Care, 1(3); DOI: http;//doi.org/05.2021/1.1014.
Copyright: © 2021 Neena.R. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Purpose: To analyse the impact of online classes on the eye health of children and young adults in the setting of COVID-19 pandemic. MATERIALS & METHODS: This was an observational study based on a written questionnaire provided to all children and young adults attending online classes, coming to the Paediatric ophthalmology & Strabismus OPD, of a tertiary eye care centre in South India, from August 2020 to January 2021 during the COVID-19 pandemic. RESULTS: Of the total 496 patients who completed the questionnaire, most were in the 5-10-year olds (44.9%), were attending online classes 1-2 hours daily and majority (84.7%) had less than 4 hours of online classes a day. However, 95.6% used electronic gadgets even after classes and 28.6% admitted to using it for more than 2 hours per day.50.8% had eye complaints which pertained to Digital Eye strain, of which headache or eye ache was most common (30.8%). Duration of online class was found to be the single most independent factor with significant association of developing eye complaints. Duration of class hours and light setting were found to be independent determinants of developing DES in our study. Worsening of refractive error and strabismus was seen in 52% and 10.1% participants respectively. New refractive error was observed in 15.3% and new strabismus in 12.4% patients with majority being symptomatic esotropias. CONCLUSION: Increased screen time, inadequate light setting, and excessive application of near vision can produce undesirable effects, including development of DES, worsening or development of new refractive errors and squint. Regulating the duration of e- learning, reducing the number of total hours of screen time, ensuring adequate lighting, taking breaks, promoting healthy lifestyle habits like increasing outdoor play should be recommended to improve the eye health of students.
Introduction:
The education system in India is facing a new crisis thanks to COVID-19 pandemic caused by the novel coronavirus SARS-CoV2.In the second week of March, state governments across the country began shutting down schools and colleges temporarily as a measure to contain the spread of the novel coronavirus.[1]A total of 320 million learners in India have been adversely affected by the COVID-19 pandemic and have transitioned to e-learning. The rapid shift to e-learning prompted by the pandemic has led to cropping up of many health problems in the students including weight gain, sleep disruption, and psychosocial stress.[2] The dependence on gadgets has worsened during the COVID-19 pandemic and has raised concerns of its negative effects on student’s eye health including that of computer vision syndrome and increased risk of myopia.[3] Even though the ministry of human resource development (MHRD), Government of India recommended just 30 minutes of screen time for pre-primary students, two classes of 45 minutes each for classes 1 to 8 and four classes of 45 minutes each for classes 9 to 12 per day, these guidelines are not strictly adhered to by many.[4]
Computer vision syndrome (CVS), also referred to as Digital eye strain (DES), describes a group of eye and vision-related problems that result from prolonged computer, tablet, e-reader and cell phone use and encompasses a range of ocular and visual symptoms. Its prevalence may be 50% or more among computer users.[5] Symptoms fall into two main categories: those linked to accommodative or binocular vision stress, and external symptoms linked to dry eye. Kozeis found that viewing computer screens regularly can lead to eye discomfort, blurred vision, fatigue, headaches, and other symptoms.[6] Zhixin Zhang etal noted that e-learning environment use time significantly affected the left and right eye visual acuity in elementary school students in China.[7]
Ever since the country wide lockdown due to Covid-19 began, we saw a substantial increase in children and young adults with issues of blurring of vision, dry eyes, headache and diplopia coming to the Paediatric ophthalmology & Strabismus OPD of our hospital. This prompted us to devise this questionnaire-based survey.
Purpose: To analyse the impact of online classes (e- learning) on the eye health of children & young adults in the setting of COVID-19 pandemic.
Materials & methods:
This was an observational study based on a written questionnaire provided to all children and young adults attending online classes, coming to the Paediatric ophthalmology & Strabismus OPD, of a tertiary eye care centre in South India, from August 2020 to January 2021 during the COVID-19 pandemic. The patients or their parents/care givers were asked to fill a written questionnaire [Table:1] regarding details of online classes including duration, mode, working distance, lighting, break in between classes and any eye complaints due to them. They were also asked to indicate if they used electronic gadgets after the online classes and if so, the duration of use. All participants underwent a comprehensive eye evaluation. Presence of any refractive error, squint, any worsening of refractive error or squint or new onset refractive error or squint were also noted. The study was conducted in accordance with the Declaration of Helsinki and was approved by the appropriate Institutional Review Board and Ethics committee.
Statistical analysis of risk factors was done using univariate and multivariate logistic regression analysis. In the univariate analysis, Chi‑square test was used to investigate the associations between the qualitative variables. In the multivariate analysis, multiple logistic regression analysis was performed to identify the independent risk factors by calculating the odds ratios (ORs) and their corresponding 95% CI. P value <0.05 was considered statistically significant.
Inclusion Criteria:
Children (5-18 years) and young adults (18-25 years) attending online classes, coming to the Paediatric ophthalmology & Strabismus OPD, of a tertiary eye care centre in South India, from July 2020 to December 2020; who answered a written questionnaire regarding online classes and eye complaints and who underwent a comprehensive eye evaluation.
Exclusion Criteria:
Those who were unable to complete the questionnaire, those with trauma and who underwent eye surgery were excluded.
Results:
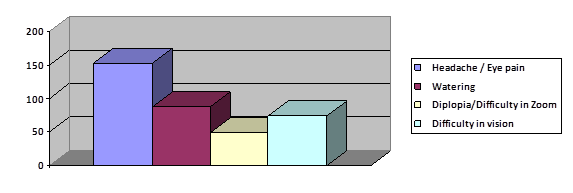
Total 496 patients who completed the questionnaire were included in the study. Mean age was 10.49 years (S.D: 3.83).Majority were in the 5-10 year age group(44.9%) and in the 10-15 year age group(40.1%); [Figure: 1].The youngest participant was 5 years old and oldest was 23 years old respectively. There was a slight female preponderance (52.8%) as compared to males (47.2%). 51.8% had 1-2 hours, 20.8% had 2-3 hours, 12.1% had 3-4 hours and 14.7% had more than 4 hours respectively of online classes in a day [Figure: 2]. Majority (42.5%) used tablets, 29.2% used laptops, 20.2% used mobiles and 7.9% used television for online classes [Figure: 3]. 84.3% had a break in between classes, even though most (40.5%) had only a break of 15 minutes. 42.7% used the electronic gadget at a working distance of 1 foot, 29.2% at 2 feet, 20.2% at less than 1 feet and 7.9% at more than 2 feet respectively. 76.2% used adequate light, 23% spotlight and 0.8% dim light respectively during the classes. 95.6% used electronic gadgets even after classes and 28.6% admitted to using it for more than 2 hours per day. 50.8% had eye complaints [Figure:4], of which headache or eye ache was most common (30.8%), followed by watering and excessive blinking (17.7%), difficulty in vision (14.9%) and double vision or difficulty in adjusting focus (9.9%).
Figure:1
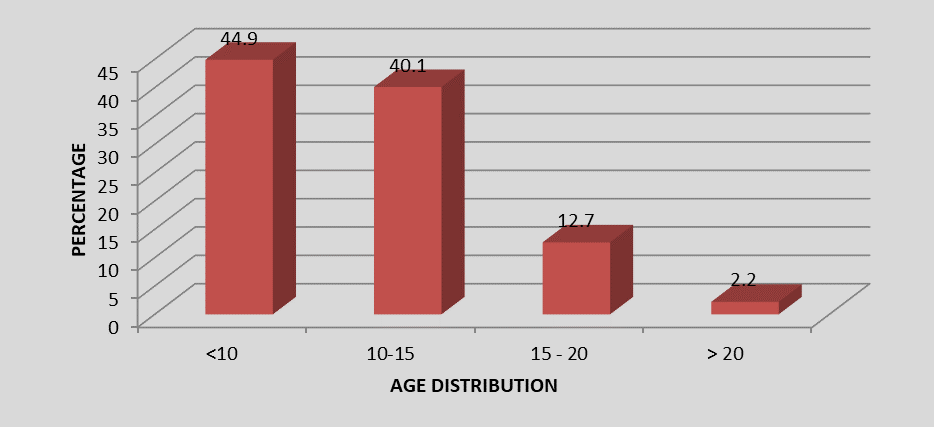
Figure:2
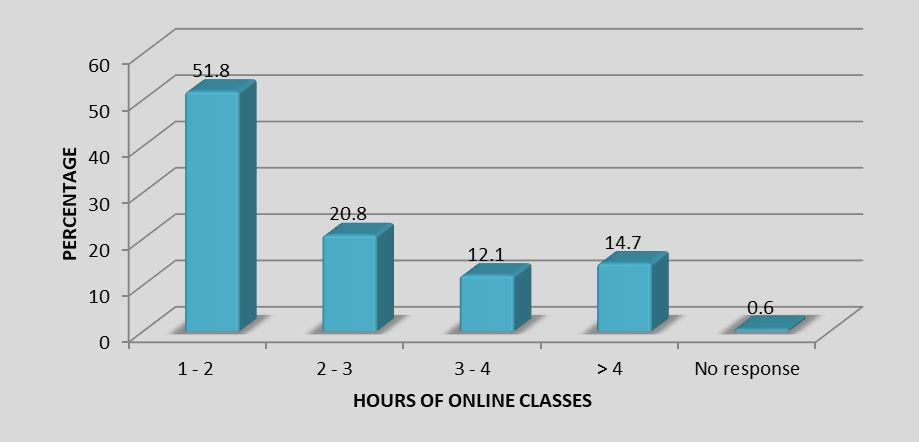
Figure:3
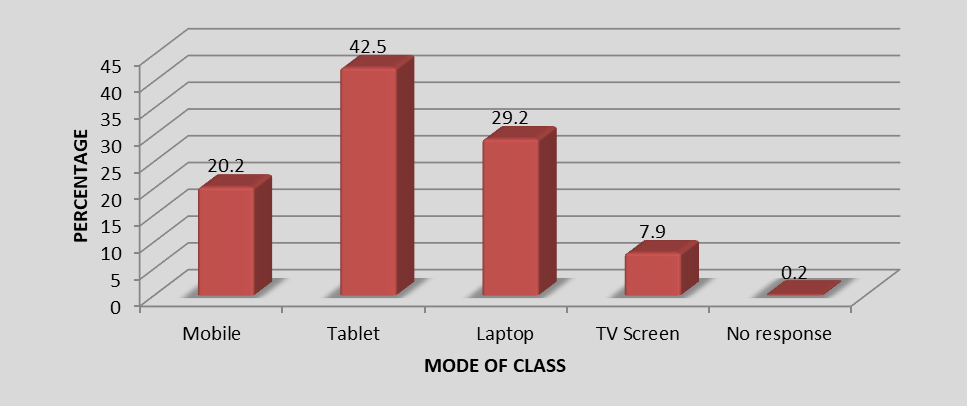
Figure: 4
Distribution of Eye Complaints
Statistical analysis by Chi square test revealed that duration of online class was the single most independent factor with significant association of developing eye complaints [Table:2]. Univariate analysis revealed that more than 2 hours of online classes had a 2.55 times increased likelihood of eye complaints and this increased to 3.28 times with more than 4 hours of online classes [Table:3]. The likelihood of headache/ eye ache was 2.13 times with more than 2 hours of online classes and 3.19 times with more than 4 hours of online classes [Table:4]. More than 2 hours of online classes also increased the risk of complaints of difficulty in vision to 2.4 times and this increased to 2.6 times with more than 4 hours of online classes [Table: 5]. Complaints of watering and excessive blinking increased with duration of online classes [Table:6] and in dim or spotlight as compared to adequate lighting. On multivariate logistic regression analysis, duration of class hours and light setting were found to be independent determinants of watering and excessive blinking [Table:7]. Subjects with duration of class hours more than 2 hrs were 1.91 times at higher risk of developing watering compared to those with less class hours [Table:8]. Subjects who used dim or spot lighting were 1.98 times at higher risk of getting watering compared to those who used adequate light setting [Table:9]. Other factors like mode of class, working distance, and break time were not found to have statistical significance.
Table:1 Questionnaire on Eye Problems in School Going Children and Adolescents Attending Online Classes
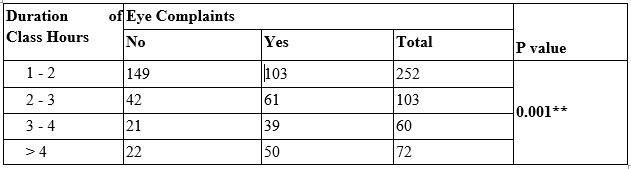
Table 2: Eye Complaints Vs Duration of Class Hours
** indicates significant association

Table 3: Determinants of Eye Problem: Univariate Analysis
** indicates significant association

Table 4: Determinants of Headache: Univariate Analysis
P value is calculated using Chi square test.
** indicates significant association
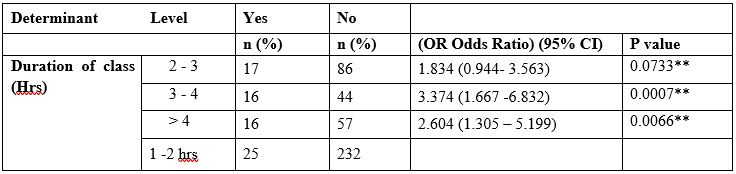
Table 5: Determinants of Difficulty in Vision: Univariate Analysis
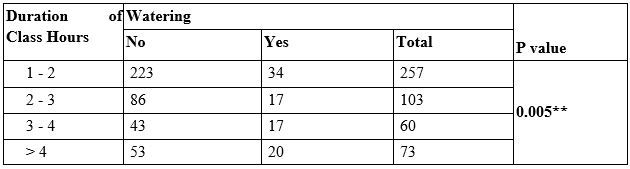
Table 6: Watering Vs Duration of Class Hours No response values are not presented in the table.
P value is calculated using Chi square test.
** indicates significant association
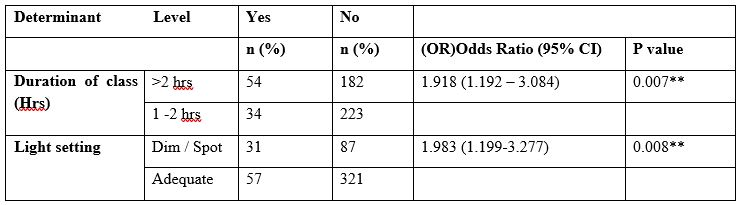
Table 7: Determinants of Watering-Multivariate Logistic Regression Analysis

Table 8: Determinants of Watering: Univariate Analysis
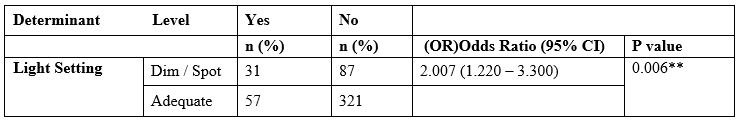
Table:9: Determinants of Watering: Univariate Analysis
Pre-existing refractive error was noted in 72% of the study patients (possibly because of this being a hospital-based survey). Compound myopic astigmatism (43.95%) was the most common pre-existing refractive error, followed by Simple myopic astigmatism (35.5%). Pre-existing strabismus was seen in 12.4% patients. Worsening of refractive error in 52% and worsening of strabismus seen in 10.1% respectively. New refractive error was observed in 15.3% and new strabismus in 12.4% patients. Among the newly detected refractive errors, Simple myopic astigmatism was the most common (59.2%), followed by Compound myopic astigmatism (30.3%), Myopia (6.6%), Hypermetropia (3.9%), Simple hypermetropic astigmatism (2.6%) and Compound hypermetropic astigmatism(2.6%). Among the newly developed strabismus, majority were esotropias (81.25%) compared to exotropias (18.75%) and were symptomatic with most having diplopia.
Discussion:
Of the 451 million monthly active users in India, 66 million are in the age bracket of five to 11 years, who access internet on devices of family members, an IAMAI report titled, ‘India Internet 2019’ said.[8] An European study by Palaiologou reported that 68% of children regularly used computers and 54% undertook online activities.[9] As per a study conducted in rural western India, the average time spent in front of a screen among children was approximately 2.7 ± 1.7 hours.[10] In a study which looked at the usage of social media devices, applications, parental knowledge and involvement among Abu Dhabi children, Badri et al, reported that the average time spent on social media by students was 5.2 hours per day.[11] Rafeeq etal [12]reported that the proportion of CVS among individuals who were using Visual Display Terminal(VDT) for more than 2 hours was significantly higher in adolescents as compared with the adult age group.
Digital eye strain (DES) [5], also known as computer vision syndrome (CVS), encompasses a range of ocular and visual symptoms which fall into two main categories: those linked to accommodative or binocular vision stress, and external symptoms linked to dry eye. Although symptoms are typically transient, they may be frequent and persistent, and bothersome. DES may be identified and measured using one of several available questionnaires, or objective evaluations of parameters such as critical flicker–fusion frequency, blink rate and completeness, accommodative function and pupil characteristics may be used to provide indices of visual fatigue. Correlations between objective and subjective measures are not always apparent. A range of management approaches exist for DES including correction of refractive error and/or presbyopia, management of dry eye, incorporating regular screen breaks and consideration of vergence and accommodative problems. Portello et al [13] also identified a clear split of computer-related symptoms into two categories: those associated with accommodation (namely, blurred vision at near, blurred distance vision after computer use and difficulty refocusing from one distance to another) and those that seemed linked to dry eye (irritated/burning eyes, dry eyes, eyestrain, headache, tired eyes, sensitivity to bright lights and eye. Moon etal noted that smartphone use was an important dry eye disease risk factor in children and recommended close observation and caution regarding video display terminal use, especially smartphones in children.[14] In our study also 50.8% had eye complaints which pertained to Digital Eye strain, of which head ache or eye ache was most common (30.8%), followed by watering and excessive blinking (17.7%), difficulty in vision (14.9%) and double vision or difficulty in adjusting focus (9.9%).
In an open online survey conducted through social media platforms for a period of 2 weeks, 93.6% of respondents reported an increase in their screen time since the lockdown.[15] With the education system itself shifting to the digital mode, parents are walking an emotional tight rope now, stuck between the demands of their children and the need to take care of their well-being. Even though majority in our study were in the 5-10-year age group and were attending online classes of 1-2 hours a day only; 95.6% used electronic gadgets even after classes and 28.6% admitted to using it for more than 2 hours per day. This was comparable to a study done in the UK, in which the participants spent approximately 4 hours per day on digital devices.[9] We found that the duration of online class was the single most independent factor with significant association of developing eye complaints. More than 2 hours of online classes had a 2.55 times increased likelihood of eye complaints and this increased to 3.28 times with more than 4 hrs of online classes. The likelihood of Digital Eye Strain (DES) also increased with increasing time of online classes (headache/ eye ache was 2.13 times with more than 2 hours of online classes and 3.19 times with more than 4 hours of online classes, difficulty in vision was 2.4 times with > 2 hours and 2.6 times with > 4 hours of online classes, watering and excessive blinking was 1.94 times with > 2 hours of online classes). Multivariate logistic regression analysis proved that duration of class hours and light setting were found to be independent determinants of DES. Subjects with duration of class hours more than 2 hrs were 1.91 times at higher risk of developing watering and excessive blinking compared to those with less class hours. Subjects who used dim/ spot illumination were 1.98 times at higher risk of getting DES compared to those with adequate light setting. Other factors like mode of class, working distance, and break time were not found to have statistical significance. Worsening of refractive error and worsening of strabismus was seen in 52% and 10.1% participants respectively. New refractive error was observed in 15.3% and new strabismus in 12.4% patients. Among the newly developed strabismus, majority were symptomatic acute acquired comitant esotropias (81.25%). Excessive application of near vision leading to development of acute acquired concomitant esotropia (AACE) has been reported by Lee etal16 and Vagge etal [17]. We also had 13 subjects with acute onset diplopia and esodeviation which were diagnosed to be AACE and are currently under evaluation.
Prolonged school closure and home confinement during the current COVID-19 lockdown have ushered in important lifestyle behaviour changes including a significant increase in screen time18 and raised serious concerns of worsening the global burden of myopia [3]. Apart from these, the excessive application of near vision might have other undesirable effects, including development of DES and acute acquired concomitant esotropia as seen in our study also.
Short comings of our study would be the lack of quantification of the DES in the study population and short duration, nevertheless we feel it is a good reflection of the impact of e-learning on the eye health of students.
Conclusion:
Increased screen time, inadequate light setting, and excessive application of near vision can produce undesirable effects, including development of DES, worsening or development of new refractive errors and squint. Regulating the duration of E- learning, reducing the number of total hours of screen time, ensuring adequate lighting, taking breaks, promoting healthy lifestyle habits like increasing outdoor play should be recommended to improve the eye health of students.