Ophthalmology and Vision Care
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Jitendra Kumar1, Renu Sahai2, Naveen Sirohi3, Samya Singh 4*
1Dept. of ophthalmology, MLB Medical College Jhansi, India.
2Dept. of pathology, MLB Medical College Jhansi, India.
3Dept of ophthalmology, MLB Medical College Jhansi, India
4Department of Ophthalmology, MLB Medical College, Jhansi, India
*Corresponding Author: Samya Singh, Department of Ophthalmology, MLB Medical College, Jhansi, India.
Received: May 06, 2021
Accepted: May 10, 2021
Published: May 17, 2021
Citation: Jitendra Kumar, Renu Sahai, Naveen Sirohi and Samya Singh. (2021) “A Prospective Study of Clinical and Histopathological Features of Eyelid Tumors”, Ophthalmology and Vision Care, 1(2); DOI: http;//doi.org/05.2021/1.1010.
Copyright: © 2021 Samya Singh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Introduction: The incidence of eyelid tumors is increasing [1-5]. Eyelid tumors thus form an important part of ophthalmology practice and are by far the most common neoplasms encountered in ophthalmic practice. Tumors of eyelids are common in people of both sexes and all age groups representing more than 90% of ophthalmic tumors [6]. Most of the tumors are diagnosed clinically. The treatment depends on the site, extent of spread and invasiveness of the tumor. Fortunately, majority of these cases are either inflammatory or non-malignant tumors
Aim: To study the clinical and histopathological features of eyelid tumors in Bundelkhand region
Material and Methods:
This study was carried out in the Department of Ophthalmology, MLB Medical College, Jhansi between November 2019 to October 2020 (12 months). All patients who fulfilled the inclusion criteria underwent surgical excision and histopathological examination.
Results:
The eyelid tumors are slightly more common in females (male female ratio 1:1.27
The majority of cases in our study presented from low socio-economic status (57.33%).
Even though eyelid tumors can present in all age group, benign tumors present more commonly in the third and fourth decade and malignant tumors in the fifth and sixth decade
The vision in the involved eye is usually not affected except in cases of large malignant tumors. Benign tumors (85.33%) are more common than malignant tumors (14.67%) (almost six times more common). Among the benign tumors, most common was epidermal inclusion cyst and among malignant tumors most common was Sebaceous gland carcinoma
Conclusion: Benign tumors were more common as compared to malignant ones.
1. Introduction:
The incidence of eyelid tumors is increasing [1-5]. Eyelid tumors thus form an important part of ophthalmology practice and are by far the most common neoplasms encountered in ophthalmic practice. Tumors of eyelids are common in people of both sexes and all age groups representing more than 90% of ophthalmic tumors [6]. Most of the tumors are diagnosed clinically. The treatment depends on the site, extent of spread and invasiveness of the tumor. Fortunately, majority of these cases are either inflammatory or non-malignant tumors; however, many malignancies can mimic a host of benign neoplasms and need differentiation before definitive therapy is started.
The eyelid:
The lesions are numerous in the eyelid due to the unique anatomical features of the eyelid as all the skin structures and its appendages, muscle, modified glands and conjunctival mucous membrane are represented in the eyelid.
Structure:
each eyelid from anterior to posterior consists of the following structures [figure1]:
Skin
Subcutaneous areolar tissue
Layer of striated muscle
Submuscular areolar tissue
Fibrous layer
Layer of non-striated muscle fibres
Palpabral conjunctiva

Figure 1: Showing structures of the eyelid (made by Dr Samya Singh, junior resident, Department of Ophthalmology)
Classification of eyelid tumors:
As tumors in other organs, tumors of the eyelid can be classified according to their tissue or cell of origin and as benign or malignant. [7,8]

Figure 2: Clinical picture of a 37 years old male, with right upper lid epidermal inclusion cyst.
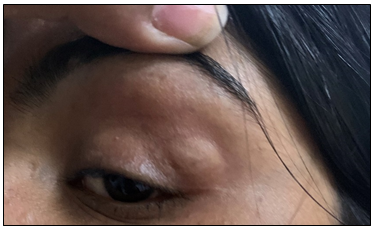
Figure 3: Clinical picture of a 17 years old patient, with left upper lid dermoid cyst
Adnexal tumors:
Lesions of adnexal origin arise from the epidermal appendages which include the sebaceous glands of Zeis, Meibomian glands, pilosebaceous units, eccrine sweat glands and apocrine sweat glands of moll.
Vascular tumors:
Includes capillary hemangioma, lymphangioma and pyogenic granuloma (most common acquired vascular lesion to involve the eyelids).
Tumors of neural origin:
neurofibroma
Pigmented lesions of melanocytic origin:
These include freckles, lentigo simplex, solar lentigo, melanocytic nevi, congenital melanocytic nevus, etc
Malignant eyelid tumors:
Malignant lesions are common around the eyes partly because many are induced by sun exposure or develop from sun-related benign lesions. They are mostly slow growing. Although most malignancies rarely metastasize but they can all be very destructive locally. Any periocular lesion that shows some growth especially when associated with chronic irritation or bleeding should undergo a diagnostic biopsy. Common malignant tumors include:
Basal Cell Carcinoma:
Squamous Cell Carcinoma:
Sebaceous Gland Carcinoma:
Malignant Melanoma:
Kaposi sarcoma:
MANAGEMENT OF TUMORS
Biopsy- can be
Incisional in which only part of lesion is removed
Excisional in which entire lesion is removed
Surgical excision followed by reconstruction:
Aims to remove entire tumor with preservation of as much normal tissue as possible.
Radiotherapy
Cryotherapy:
For small superficial BCCs useful as an adjunct to surgery
2. Material and Method:
We included any patients who were admitted in the IPD of department of Ophthalmology, M.L.B. Medical college, Jhansi between November 2019 to October 2020 (12 months) whosatisfied the eligibility criteria. Patients were included in the study under the following inclusion and exclusion criteria:
Inclusion criteria:
We included the following patients:
All patients who presented with primary tumors over eyelid (benign and malignant) and satisfied the following criteria:
Age between 3 years- 70 years
Those who were fit for surgery
Those who were willing to undergo surgery
Patients who were willing to give a written consent for the study
Surgeries performed by a trained ophthalmologist
Those who were willing to come for follow up
Exclusion criteria:
Patients who refused treatment or biopsy
Patients having lid swelling secondary to infectious lesion like stye, angioneurotic edema, molluscum contagiosum, pyogenic granuloma and chalazion were excluded from our study.
Patients with previously resected lid tumours
Patients with primary intraocular tumours that spread to the eyelids
Patients with history of trauma
Physically or mentally unfit patients
Patients who did not come for follow up after 1 or 2 visits
Patients satisfying the inclusion criteria signed an informed and written consent before participating in the study:
A detailed history of all the patients was taken and the parameters that were noted included demographics of patients, history of trauma and history of tumours in other parts of the body. A thorough clinical examination of the lesion regarding its location, shape, size, border, margin, skin overlying lesion, eyelashes, ulceration, induration and mobility over the underlying surface was done.The anterior and posterior segment examination of both eyes was thoroughly done by slit lamp and direct and indirect ophthalmoscope. The acronym LUM (loss of eyelashes, ulceration, margin obliteration) was created to assist in memory recall and analyzed to provide physicians with an evidence-based, easy-to-remember system for assisting in the triaging of these lesions [9].

Figure 4: Clinical picture of a 60-year-old patient suspected of having BCC in the left lower lid

Figure 5: Clinical picture of same pt as seen on slit lamp(20x)
After obtaining routine investigations like complete blood cell counts, fasting blood sugar, bleeding time, clotting time and urine sugar and albumin, the patients were posted for surgery as per protocol. Radiological investigations for assessment of extent of lesion were obtained wherever indicated. Patients were briefed about the surgery and written consent was taken for surgical procedure. Clinically diagnosed malignant tumour was excised with 3mm clear margins followed by reconstructive lid surgery under local anesthesia using was xylocaine 2% with adrenaline (1:200000) which was infiltrated around the lesion. The specimen was preserved in a bottle containing 10% formalin and sent to the Department of Pathology for histopathological examination. The specimen was fixed with formalin and stained with hematoxylin and eosin [H and E]. Histopathological examination of the specimen was done under a microscope (10x, 40x and 100x) to obtain a definitive diagnosis. After that photos were taken using a NIDEK DSLR camera.

Figure 6: Clinical picture of an excisional biopsy being done on the left eye of 65 year old patient with mass over left upper lid in the eye operation theatre at MLB Medical College, Jhans

Figure 7: Clinical picture showing histopathological evaluation of specimens under the microscope in the Department of Pathology, MLB Medical College, Jhansi
The procedures followed were in accordance with the ethical standards committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975, as revised in 2000. The necessary permission from the Ethical and Research Committee was obtained for the study.
Stastistical Analysis:
The patient’s protocols were recorded in data collection form. Quantitative data were expressed as mean and qualitative variables were expressed using percentages
3.Results:
A total of 80 patients who fulfilled the inclusion criteria were selected for this study out of which 5 patients were excluded (dropouts) at initial stage of study due to various reasons mentioned below. Finally, 75 patients were included in this study. In total 75eyes of 75 patients were included in the study.
|
Age (in years) |
Number of patients |
Percentage (%) |
|
0-10 |
7 |
9.33% |
|
11-20 |
10 |
13.33% |
|
21-30 |
15 |
20% |
|
31-40 |
11 |
14.67% |
|
41-50 |
13 |
17.33% |
|
51-60 |
13 |
17.33% |
|
61-70 |
6 |
8% |
|
Total |
75 |
100 |
Table 1: Age Wise Distribution of Various Tumours (Both Benign and Malignant)
|
Sex |
Number of patients |
percentage |
|
Male |
33 |
44% |
|
Female |
42 |
56% |
|
Total |
75 |
100 |
Table 2: Gender distribution
|
Socioeconomic Status |
Number of patients |
Percentage |
|
High |
6 |
8 % |
|
Medium |
26 |
34.67% |
|
Low |
43 |
57.33% |
|
Total |
75 |
100% |
Table 3: -Socio-economic status of total patients (according to the modified Kuppuswami scale)
|
Baseline BCVA/log MAR (in operative eye) |
No. of cases |
Percentage (%) |
|
6/6(0) |
27 |
36% |
|
6/9(0.176) |
16 |
21.33% |
|
6/12(0.301) |
9 |
12% |
|
6/18(0.4771) |
7 |
9.33% |
|
6/24(0.602) |
5 |
6.67% |
|
6/36(0.78) |
1 |
1.33% |
|
6/60(1) |
3 |
4% |
|
FC 3mt(1.301) |
1 |
1.33% |
|
FC 2mt(1.477) |
1 |
1.33% |
|
FC 1mt(1.778) |
0 |
0% |
|
HM+ |
1 |
1.33% |
|
PL+ |
2 |
2.67% |
|
PL- |
0 |
0 |
|
Response to light-follows light |
2 |
2.67% |
|
Total |
75 |
100% |
Table 4: Bcva In Operative Eye of The Patients At The Time Of Persentation
BCVA (best corrected visual acquity), FC (finger counting), HM (hand movement), PL (perception of light), + (positive), - (negative)
|
Type |
Number |
% |
Female |
Male |
|
Malignant |
11 |
14.67 |
7 |
4 |
|
Benign |
64 |
85.33 |
35 |
29 |
|
Total |
75 |
100 |
42 |
33 |
Table 5: Distribution of cases according to the type of lesion
|
Type |
Number |
% |
Male |
Female |
|
Basal Cell Carcinoma |
4 |
36.36 |
1 |
3 |
|
Sebaceous cell carcinoma |
5 |
45.45 |
1 |
4 |
|
Squamous cell carcinoma |
2 |
18.18 |
2 |
0 |
|
Total |
11 |
100 |
4 |
7 |
Table 6: Total Number and Percentage of Cases of Malignant Tumor.
|
Type |
Number |
% |
Male |
Female |
|
Epidermal inclusion cyst |
25 |
39.06 |
7 |
18 |
|
Dermoid cyst |
17 |
26.56 |
10 |
7 |
|
Squamous papilloma |
9 |
14.06 |
5 |
4 |
|
Sebaceous cyst |
3 |
4.69 |
1 |
2 |
|
Xanthogranuloma |
3 |
4.69 |
2 |
1 |
|
Granulomatous lesion (pyogenic granuloma) |
2 |
3.13 |
1 |
1 |
|
Sebaceous keratosis |
2 |
3.13 |
2 |
0 |
|
Eccrine hidrocytoma |
1 |
1.56 |
1 |
0 |
|
Capillary hemangioma |
1 |
1.56 |
0 |
1 |
|
Reverse follicular keratosis |
1 |
1.56 |
0 |
1 |
|
Total |
64 |
100 |
29 |
35 |
Table 7: Total Number of Cases and Percentage of Benign Tumors
|
Type |
Age group (range) in years |
Mean age of presentation (In years) |
|
Basal cell carcinoma |
60-70 |
64.50 |
|
Sebaceous gland carcinoma |
45-62 |
56.40 |
|
Squamous cell carcinoma |
50-60 |
55 |
Table 8: Age wise distribution of various malignant tumors
|
Type |
Male: Female |
Mean age (in years) |
Eye involved (right: left) |
Location (UL: LL) |
|
Basal cell carcinoma |
1:3 |
64.50 |
3:1 |
1:3 |
|
Sebaceous gland carcinoma |
3:2 |
56.40 |
3:2 |
5:0 |
|
Squamous cell carcinoma |
0:2 |
55 |
1:1 |
2:0 |
Table 9: Clinical features of various malignant tumours
|
Type |
Age-group (range) In years) |
Mean age (in years) |
|
Epidermal inclusion cyst |
3-65 |
30.52 |
|
Dermoid cyst |
3-67 |
26.53 |
|
Squamous papilloma |
17-70 |
46 |
|
Sebaceous cyst |
28-32 |
30 |
|
Xanthogranuloma |
42-54 |
47 |
|
Granulomatous lesion (pyogenic granuloma) |
35-55 |
45 |
|
Seborrhoeic keratosis |
49-52 |
50.50 |
|
Eccrine hidrocytoma |
28 |
28 |
|
Capillary hemangioma |
4 |
4 |
|
Reverse follicular keratosis |
54 |
54 |
Table 10: Age wise distribution of various benign tumors
|
Type |
Male: female |
Mean age (in years) |
Eye involved (right:left) |
Location (UL:LL) |
|
Epidermal inclusion cyst |
7:18 |
30.52 |
13:12 |
18:7 |
|
Dermoid cyst |
10:7 |
26.53 |
10:7 |
15:2 |
|
Squamous papilloma |
5:4 |
46 |
5:4 |
5:4 |
|
Sebaceous cyst |
1:2 |
30 |
1:2 |
3:0 |
|
Xanthogranuloma |
2:1 |
47 |
2:1 |
2:1 |
|
Granulomatous lesion(pyogenic granuloma) |
1:1 |
45 |
2:0 |
2:0 |
|
Seborrhoeic keratosis |
2:0 |
50.50 |
0:2 |
2:0 |
|
Eccrine hidrocytoma |
1:0 |
28 |
0:1 |
1:0 |
|
Capillary hemangioma |
0:1 |
4 |
0:1 |
0:1 |
|
Reverse follicular keratosis |
0:1 |
54 |
1:0 |
1:0 |
Table 11: Clinical Features of Various Benign Tumours
|
Duration (in years) |
Malignant tumors |
Benign tumors |
|
0-1 |
0 |
0 |
|
1-2 |
2 |
12 |
|
2-3 |
5 |
20 |
|
3-4 |
2 |
23 |
|
4-5 |
1 |
4 |
|
>5 |
1 |
5 |
Table 12: Distribution of Cases According to Duration of Lesion at Presentation

Figure 8: Histopathological picture of epidermal inclusion cyst (H&E 40x) [courtesy: Department of Pathology, MLB Medical College, Jhansi]

Figure 9: Histopathological picture of BCC (H&E 40x) [courtesy: Department of Pathology, MLB Medical College, Jhansi]
4.Discussion:
Eyelid lesion is a common condition in clinical practice encountered by ophthalmologists [10]. Approximately 5%-10% of all skin cancers and 15% of all face tumors occur on the eyelid [11]. Several studies have been done time and again which prove beyond doubt that incidence of eyelid tumors is increasing. Histopathological examination of eyelid tumours becomes very important as often there is discrepancy in the clinical diagnosis and biopsy result. 75 cases who fulfilled the inclusion criteria were studied over a period of 12 months from November 2019 to October 2020 in the Department of ophthalmology, Maharani Laxmi Bai Medical College, Jhansi.
Demography:
In our study the overall male female ratio was found to be 1:1.27(33:42). The number of cases were found slightly more in females than males. In the malignant tumour cases male female ration was found to be 1:1.75(4:7) therefore slightly more in females while in benign cases male female ration was found to be 1:1.20(29:35) therefore slightly more in females. In a study done by Gosai et al from June 2007 to July 2009, 120 patients of eyelid tumors were studied where male to female ratio was 1.4:1 for benign tumors whereas amongst the malignant cases females outnumbered males with ratio of 1.16:1[12]. In a retrospective study done by Sharma et al on 135 cases, female to male ratio was 1.3:1 in malignant cases and thus showed preponderance of female patients in malignant tumors [13]. Studies by Krishnamurthy et al [14] (male to female ratio 1:1.5) and Bagheri et a [15]l (male to female ratio 1:1.5) also showed similar results. The most probable reason for the slightly higher number of female cases could be that females are more conscious cosmetically and therefore present more frequently to the hospital for excision.
The majority of cases in our study presented from low socio-economic status (57.33%). Lim et al found that a high incidence of BCC and a larger BCC size were associated with a low socioeconomic status, which corresponds to studies in the UK, Ireland and the Netherlands showing that patients living in areas of socioeconomic deprivation are more likely to have BCC. Since early and small BCCs are usually easily managed with a good prognosis, prevention is preferable to treatment. People living in economically deprived areas should be informed that simple measures like avoiding extensive sun exposure or the long-term use of hats with brims can reduce the incidence of periocular skin cancers [16].
The vision in the involved eye is usually not affected except in cases of large malignant tumors. In this study we found that majority of patients had a vision of 6/6 or 6/9 in the involved eye (30.67% and 24.33% respectively) though there were patients with vision as low as PL positive. The patients with lower vision were mostly either of the older age-group or had large malignant tumors.
The most common type of tumours seen were benign tumors(85.33%) while the malignant tumors accounted for about 14.67% , which is nearly similar to that reported by Krishnamurthy et al (2014)[14] from Karnataka in which they found that 91.9% cases were benign eyelid tumours. Xu et al[17] from Beijing found 86.2% benign tumours involving 2638 patients, Deprez et al[11] found 84% benign lesions from a study on 5504 cases, Paul S et al[18] found that 75.9% were benign and Obata H et al[19] found73% benign cases. In a similar study conducted in Siriraj Hospital from 2000 to 2004, the majority of tumors were benign, while malignant tumors contributed only 10.8% of the total eyelid lesions [10]. In a study by Rathod et al, there were 61 benign and 39 malignant cases out of a total of 100 cases of eyelid tumors [6]. In a similar study by Aurora and Bloodi in 1970 comprising of 892 cases, non-malignant lesions accounted for 76% of all the cases, while malignant cases accounted for 24%. Hence, they found that non-malignant cases were 3 times more common than malignant[20] However, studies by Abdi et al[1] (India) & Bagheri A et al[15] from Tehran have reported 58.9% (n=207 cases) and 45.5% (n=182 cases) benign cases respectively, showing comparatively lesser prevalence of benign lesions. These differences could be attributed to the differential referral pattern to a center equipped with oculoplasty services [9]. Most studies therefore show that benign lesions largely constitute the most frequent type of eyelid tumours outnumbering the malignant category in the general population.
Amongst the malignant tumors, the most common type was the Sebaceous gland carcinoma (45.45%) followed by basal cell carcinoma (36.36%) and lastly the Squamous cell carcinoma (18.18%). In the study by Gosai et al in M & J Western Institute of Ophthalmology from June 2007 to July 2009, amongst the malignant tumors mebiomian gland carcinoma was maximum (46. 34%) followed by basal cell carcinoma (29.26%) and then by squamous cell carcinoma (21.93%) [12]. In a study done in Central India by Jahagirdar et al where a series of 27cases of eyelid malignancies were analyzed, sebaceous cell carcinoma (37%) was almost as prevalent as basal cell carcinoma [21]. In another study by Sharma et al, sebaceous cell carcinoma constituted 44.4% of all malignancies which was almost similar to our study [13]. In a study done by Ramya et al sebaceous gland carcinoma was commonest malignant tumor (47.7%) followed by basal cell carcinoma (26.8%) and squamous cell carcinoma (21.9%) [22]. Sihota R et al (1996) performed a retrospective study of 313 tumors of the eyelids in the Indian population. There was almost equal incidence of sebaceous gland carcinoma (32.56%), basal cell carcinomas (29.77%) and squamous cell carcinoma (28.08%) among malignant tumors [23].
The reported incidence of SGC varies from 0.5 to 5% of all lid carcinomas in USA and approximately 25–30% in China and India [23,24,25]. The study by Deprez and Uffer[37] reported that basal cell carcinoma accounted for 86% of all malignant tumors.
Among whites, light pigmentation is a risk factor for BCC; conversely, the disease is rare among blacks. These evidences suggest that BCC is related to chronic and cumulative solar damage and it is more common in fair. skinned and elderly adults. The relation between BCC and sun exposure had been proposed by various researchers [9]. Up to 30% of Caucasians develop basal-cell carcinomas in their lifetime.
SGC is more common in Asian population (South Asian and Indians) accounting for 27–40% of all eyelid malignancies.[5,26,27] In the white population SGC is rare, accounting for 1–5.5% of all eyelid malignancies.[5,27,28,29]. Racial and genetic predisposition may probably play an important etiological role.[30]. SGC is known to masquerade as chalazion in eyelid, hence the possibility of SGC should be considered in Asians presenting with persistent or recurrent chalazion.[27]. In studies by Ni et al (U S) observed that SGC accounted for 32.7% of malignant eyelid tumors in Shanghai; whereas, at the Massachusetts Eye and Ear Institute in United states, SGC accounted for only 1.5% of malignant eyelid tumors.[30,31] The reported incidence of SGC in USA varies from 0.5 to 5% of all lid carcinomas.[32] In the San Francisco population, despite having a significantly higher no of Asians, SGC was reported in only 7.3% of all eyelid malignancies than other parts of the United States. This result has confirmed that established Asian/Pacific Islander an-cestry is not a risk factor for developing sebaceous carcinoma as concluded by a recent study by Dasgupta et al [31,33]. In Asians, SGC accounts for a higher proportion of eyelid malignancies, similar to our study, but this is not due to a higher incidence of SGC but to a relative lack of other malignant eyelid tumors [31]. Higher incidence of sebaceous gland carcinoma can be attributed to oily nature of skin among Indians. Decline in basal cell and squamous cell carcinoma can be due to more melanin in indian population which provides preotection from sunlight.
The age of presentation for malignant tumors ranged from 45-70 years for malignant tumors. The mean age of presentation for malignant tumors was found to be -64.50 years for basal cell carcinoma, 56.40 years for sebaceous gland carcinoma and 55 years for squamous cell carcinoma. These results are similar to a study by Kale (2012) et al from India who observed that mean age was 59 years [16]. Hussain et al (2013) from Pakistan found that the mean age of the patients with eyelid malignancy was 59.3±14.2 years [21]. Wang et al reported 127 cases of malignant eyelid tumor with a mean age of presentation of 62.6 year [5]. Rathod et al reported 100 cases of eyelid tumors with mean age of malignant eyelid tumors presentation was 58.59±11.271 and benign tumors was 37.02±16.847[6]. The median age of presentation was 63 years for SGC, 60years for BCC, 57.5years for SCC, 55years for melanoma. lymphoma presented at 75 years and MCC at 52years in a study by Krishnamurthy et al [40]. Thus, we see that malignant tumors are more common after the fifth decade.
Right eye was more frequently involved in cases of BCC (3 out of 4 cases) and SGC (3 out of 5 cases) while in SCC both eyes were equally involved. BCC was located more frequently on the lower lid (3 out of 4 cases) while SGC was located more frequently on the upper eyelid (all five cases). SCC was found only in upper eyelid in the two cases that we studied. Most sebaceous gland carcinomas were found on the upper eyelid which possibly reflected the greater number of meibomian glands in the upper eyelid [36]. Basal cell carcinomas commonly affected the lower eyelid that is consistent with other studie[5,37]. In a study by karan S et al there was marked predilection for right eye in both benign and malignant lesions [38] while in most studies no specific laterality was found.
Amongst the benign tumors we found that epidermal inclusion cyst presented most frequently (39.06%) followed by dermoid cyst (26.56%). Squamous papilloma was the third most frequent (14.06%). These results are similar to the study by Krishnamurthy et al (2014) from Karnataka in which the most common benign lesions were epidermal cysts (30.5%), naevi (17.5%), dermoid cysts (13.8%) and papilloma (6.5%) [14]. Hsu and Lin [39] series reported epidermal cysts (23.1%) to be the most common lesion and Kersten et al reported it as the second most common lesion in their cases series (22.2%). However, Abdi et al [1] from India reported vascular tumours (21.3%), neural tumours (18.0%), dermoid cysts (16.4%), squamous cell papilloma (13.1%) and naevi (12.3%) as the common benign lesions. Xu XL et al (2008) from China found that the most common benign lesions were inflammatory lesions, melanocytic nevi, papillomas, dermoid and epidermoid cysts, and epithelial cysts [17]. In Bastola et al study (2013), the conclusion was made that the most common benign lesion was dermoid cyst (21%) which was followed by epidermal inclusion cyst (14%) and then dermal nevus (12.2%)[40] .Thus, we see that in different studies there is a difference in the most commonly presenting benign tumour.
The age of presentation of benign tumors ranged from 3 years to 67 years. The mean of presentation of the most common benign tumor i.e. the epidermal inclusion cyst was found to be 30.52 years, 26.53 years for dermoid cyst, 46 years for squamous papilloma, 30 years for sebaceous cyst, 47 years for xanthogranuloma , 45 years for granulomatous lesion, 50.50 years for seborrheic keratitis, 28 years for eccrine hidrocytoma, 4 years for capillary hemangioma and 54 years for reverse follicular keratosis. Similarly, karanS et al reported that benign tumor ranged 0-70 years and most common age group was 31-40[38].
No significant laterality was noticed in our cases of benign tumor. Upper eyelid was more frequently involved in most benign tumors (73.44%) [table 13]. These results are consistent with the study by Krishnamurthy et al [40] who showed that the upper eyelid (n=131, 60.6%) was more commonly involved than the lower lid (n=85, 39.4%).
Malignant tumors being more rapidly growing and aggressive, had a shorter duration at presentation which was between 1 and 5 years (maximum cases seen at 2-3 years) [table14 and graph 11]. This is was also found in a study by karan et al [38]. Benign tumors are slow growing in nature therefore majority were seen at 3-4 years duration [ table 14 and graph 11].
Malignant cases had a maximum incidence of complications at presentation. 7 out of 11 malignant tumors, presented with one or more complications and few upper lid tumors presented with mild to severe ptosis. There was no case of recurrence seen in our study probably because the duration of study was short (12 months). Also, no case of metastasis from elsewhere was reported. The method for surgical removal employed was wide excision with tumor free margins.
5.Conclusion:
At the end of the duration of the study we can concluded that-
The eyelid tumors are slightly more common in females (male female ratio 1:1.27). The most probable reason for the same could be that females are present to the hospital more often as they are cosmetically more aware.
The majority of cases in our study presented from low socio-economic status (57.33%). Hence, we have to spread more awareness amongst them
Even though eyelid tumors can present in all age group, benign tumors present more commonly in the third and fourth decade and malignant tumors in the fifth and sixth decade. This point is important for the clinician to keep in mind while making a diagnosis especially in these age groups.
The vision in the involved eye is usually not affected except in cases of large malignant tumors. In this study we found that majority of patients had a vision of 6/6 or 6/9 in the involved eye (36% and 21.33% respectively) though there were patients with vision as low as PL positive. The patients with lower vision were mostly either of the older age-group (therefore could have other age-related causes for diminution of vision) or had large malignant tumors.
Benign tumors are more common than malignant tumors (almost six times more common). There could be differences in the number of cases of each type which could be attributed to the differential referral pattern to a center equipped with oculoplasty servicesand avoidance of the disease and/or late presentation/incautious to seek timely medical advice in developing nations.
Among benign tumors the most common one is epidermal inclusion cyst and among malignant tumors the most common one is SGC. This result can vary from region to region. These differences can be due to multiple factors such as genetic predisposition, environmental trigger and ocular infections. Another factor affecting this could the referral bias to tertiary care centers and lack of appropriate medical facilities in rural areas.
Wide excision with tumor free margin can be employed for surgical management with low complication rates. Recurrence and metastasis are rare among eyelid tumors.
The limitations of this study could be emphasized as having lesser number of study subjects and short duration of follow up. So, a long term, multi-centeric study with more follow-up visits and duration is the need in coming future. In developing countries, people have to be aware of eyelid tumors (their risk factors, prevention, presentation and cure). Also, proper medical facilities oriented to timely screening, diagnosis, management and referral need to be set up with efficient staff and ophthalmologists and/or oculoplasty surgeons