Ophthalmology and Vision Care
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Anubhav Chauhan 1*, Deepak Kumar Sharma 2, Pankaj Kumar Thakur 3, Anchit Wap4
1Medical Officer (Specialist), Deptt. of Ophthalmology, Shri Lal Bahadur Shastri Government Medical College and Hospital, Nerchowk, Distt. Mandi, Himachal Pradesh, India.
2Assistant Professor, Deptt. of Ophthalmology, Shri Lal Bahadur Shastri Government Medical College and Hospital, Nerchowk, Distt. Mandi, Himachal Pradesh, India.
3Medical Officer(Specialist), Deptt. of Ophthalmology, Shri Lal Bahadur Shastri Government Medical College and Hospital, Nerchowk, Distt. Mandi, Himachal Pradesh, India.
4Senior Resident, Deptt. of Ophthalmology, Shri Lal Bahadur Shastri Government Medical College and Hospital, Nerchowk, Distt. Mandi, Himachal Pradesh, India.
*Corresponding Author: Anubhav Chauhan, Medical Officer (Specialist), Deptt. of Ophthalmology, Shri Lal Bahadur Shastri Government Medical College and Hospital, Nerchowk, Distt. Mandi, Himachal Pradesh, India.
Received: April 10, 2021
Accepted: April 16, 2021
Published: April 19, 2021
Citation: Chauhan.A and Deepak K Sharma and Pankaj K Thakur and Anchit Wap .(2021) “Pituatory Tumor Mimicking Retrobulbar Neuritis”, Ophthalmology and Vision Care, 1(2); DOI: http;//doi.org/04.2021/1.1008.
Copyright: © 2021 Anubhav Chauhan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
A twenty-nine-year-old male presented with a history of diminition of vision in the left eye for four months. There were no other symptoms. Magnetic Resonance Imaging (MRI) of brain revealed pituatory tumor. Unilateral loss of vision was the presenting sign in this case diagnosis.
Introduction:
Intracranial tumours are a leading cause of morbidity and mortality in patients. Clinical features are caused by mass effect, raised intracranial pressure or influence of hormones. Eye signs and symptoms occur as an initial presentation in up to fifty percent of patients diagnosed with primary brain tumours in adults.[1]
Case:
A twenty nine year old male presented with a history of painless,progressive diminition of vision in the left eye for four months. There was no other significant perinatal, medical, surgical, family, traumatic or drug abuse history. Ocular examination was carried out and his visual acuity was 6/6 in the right eye and hand movements close to face in the left eye. He was diagnosed and treated as a case of retrobulbar neuritis in the left eye elsewhere, but no investigations were carried out (as per the records brought by him). On ocular examination, hispupillary reactions, ocular movements, intraocular pressure and fundus were normal bilaterally.
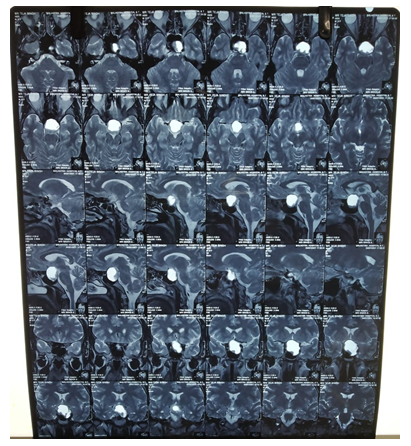
Figure 1A
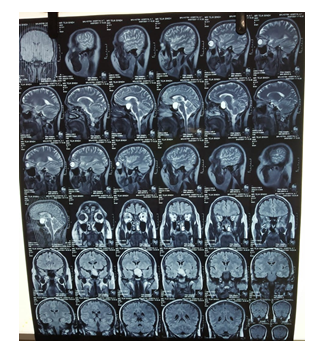
Figure 1B
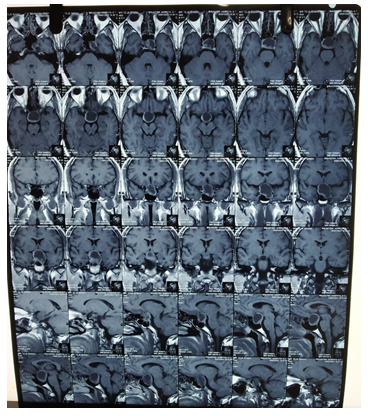
Figure 1C
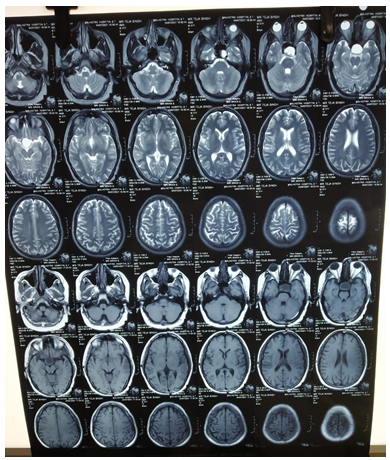
Figure 1D
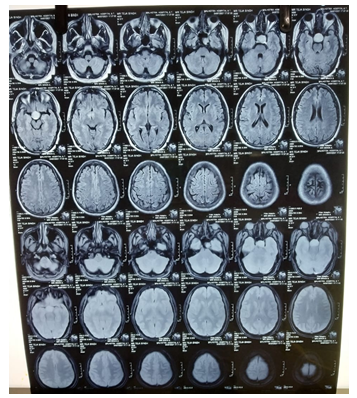
Figure 1E
An MRI of the brain(figure 1a,1b,1c,1d,1e) was done which revealed a 2cm by 2cm by 3 cm peripherally enhancing cystic lesion in the sella and suprasellar region not seperately differentiated from the pituatory gland and possibilities of pituatory adenoma,craniopharyngioma and rathke's cleft cyst were given. Laboratory workup of the patient was not performed and the patient was referred to a neurosurgical and endocrinologist opinion at a higher centre.We are awaiting a followup from him.
Discussion:
Ophthalmic signs and symptoms in brain tumors include visual loss, diplopia, nerve palsy, pupillary abnormalities, and optic nerve head defects.[2] Pituitary diseases are an important cause of compression of optic chiasma leading to visual disturbances. Pituitary adenomas, craniopharyngiomas, meningiomas, and pituitary apoplexy are a few important examples.Visual field defects may be one of the first signs of developing pituitary tumors.[3] The ophthalmic presenting symptoms of pituitary enlargement also depend upon the compression of the neighbouring structures. The pituitary fossa is bounded superiorly by optic chiasm, cavernous sinuses on both sides, and sphenoid sinus inferiorly. The visual signs could be due to raised intracranial pressure, compression of the structures in the visual pathway, and the involvement of cranial nerves in the cavernous sinus.[4]
Neurosurgery is the treatment of choice for nonfunctioning pituitary adenomas [5] while functioning pituitary adenomas that secrete prolactin usually require dopamine-agonist such as bromocriptine. Surgical resection, usually with the trans-sphenoidal approach, should be considered for pituitary tumors that secrete prolactin and show rapid deterioration in visual function. When medical and surgical treatments are unsuccessful, radiotherapy may be used post-operatively.[6]
Source Of Support-None:
The paper being submitted has not been published,simultaneously submitted,or already accepted for publication elsewhere.
Conflicts of Interest: The authors declare that they have no competing interest.
Financial Disclosure(s): The authors have no proprietary or commercial interest in any material discussed in this article.