
Ihar Ihnatovich1, Alexandr Vasilevich1
1Belarusian State Medical University, Minsk, Belarus.
*Corresponding author: Ihar Ihnatovich, Belarusian State Medical University, Minsk, Belarus.
Received date: January 29, 2023
Accepted date: February 10, 2023
published date: February 27, 2023
Citation: Ihnatovich I, Vasilevich A. (2023) “Advance In the Management of Acute Mesenteric Ischemia Over the Past 10 Years: A Case Study Demonstration”. International Surgery Case Reports, 5(1). DOI: http;//doi.org/02.2023/1.1063.
Copyright: © 2023 Ihar Ihnatovich. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
12/2010 Patient R., 70 years old, admitted to the emergency room 3 hours after the onset of severe abdominal pain and vomiting. History: right nephrectomy, ischemic heart disease, atrial fibrillation
Case Study
12/2010 Patient R., 70 years old, admitted to the emergency room 3 hours after the onset of severe abdominal pain and vomiting. History: right nephrectomy, ischemic heart disease, atrial fibrillation.
Upon admission, the patient's status was of moderate severity. Heart sounds were arrhythmic, blood pressure was 150/80 mmHg. The abdomen was moderately bloating, soft and without peritoneal symptoms. Intestinal peristalsis enhanced. Electrocardiography revealed atrial fibrillation, after abdominal ultrasound examination and fibrogastroduodenoscopy no additional information was obtained. Rectal examination revealed the presence of blood in the feces. Medication carried out, but it was not possible to control the pain syndrome. After 3 hours, initial symptoms of peritoneal irritation identified in the lower part of the abdomen. This fact was an indication for laparotomy because of an uncertain diagnosis of peritonitis. Laparotomy revealed bluish-burgundy loops of the jejunum and ileum without normal peristalsis. There were no signs of necrosis of the intestinal wall. (Fig.1).

Figure 1: Ischemic small intestine at laparotomy
Thromboembolism of the superior mesenteric artery (SMA) diagnosed. Exposure of the SMA performed from the anterior approach in the root of the mesentery. Arteriotomy performed in the 2nd segment below the origin of a. colica media (Fig.2).
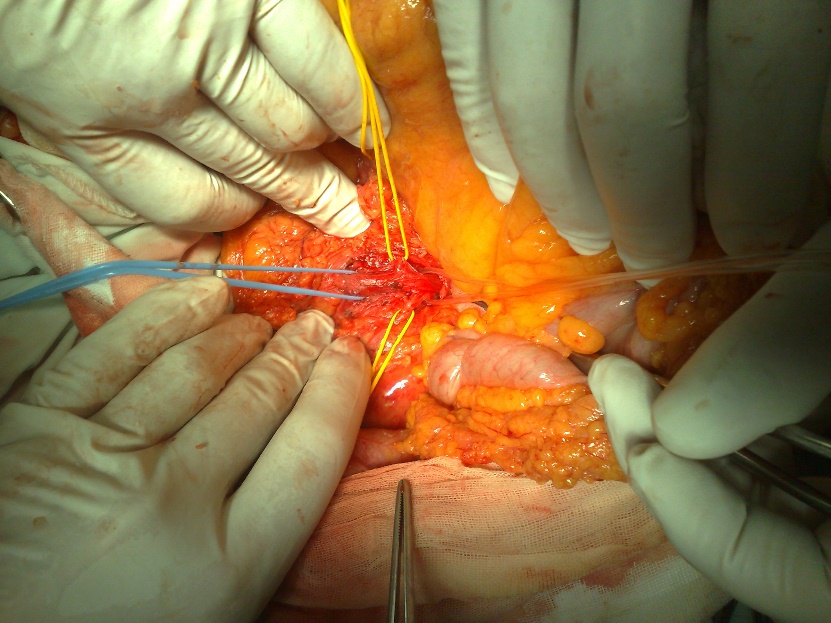
Figure 2: Dissected SMA (blue tourniquet) and artery colica media (yellow tourniquet)
Balloon thromboembolectomy from the lumen of the SMA performed using 4 Fr Fogarty catheter (Fig.3).
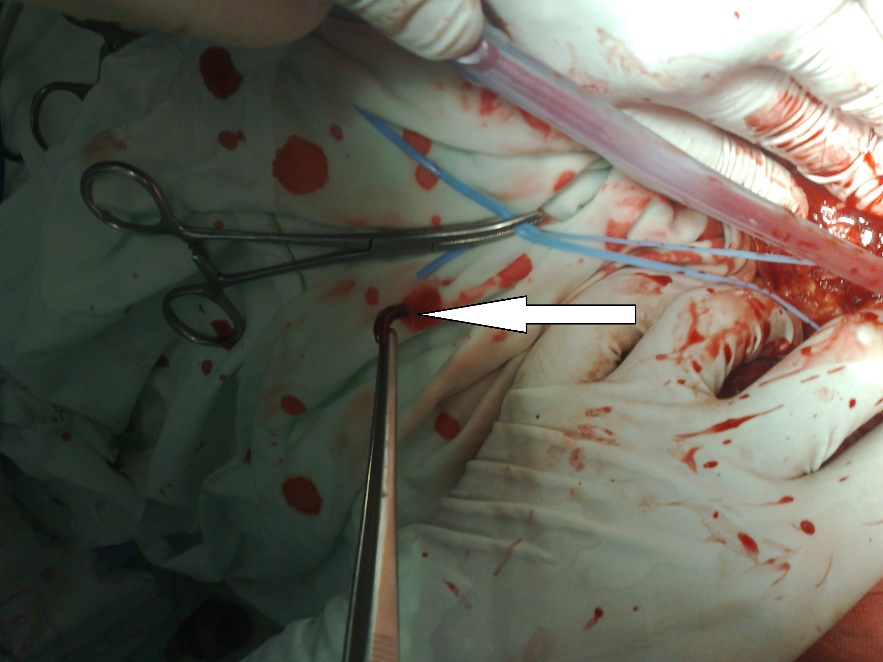
Figure 3: Thrombus removed from SMA (white arrow)
As a result, a pulsating central and satisfactory retrograde blood flow obtained. The incision of the arterial wall sutured. The early postoperative period was uneventful. On the 2nd day after the laparotomy and surgical intestinal revascularization, the second look re-laparotomy performed for clinical re-assessment of intestine viability. It established that the small intestine was viable, with normal peristalsis, and has a normal color (Fig.4).
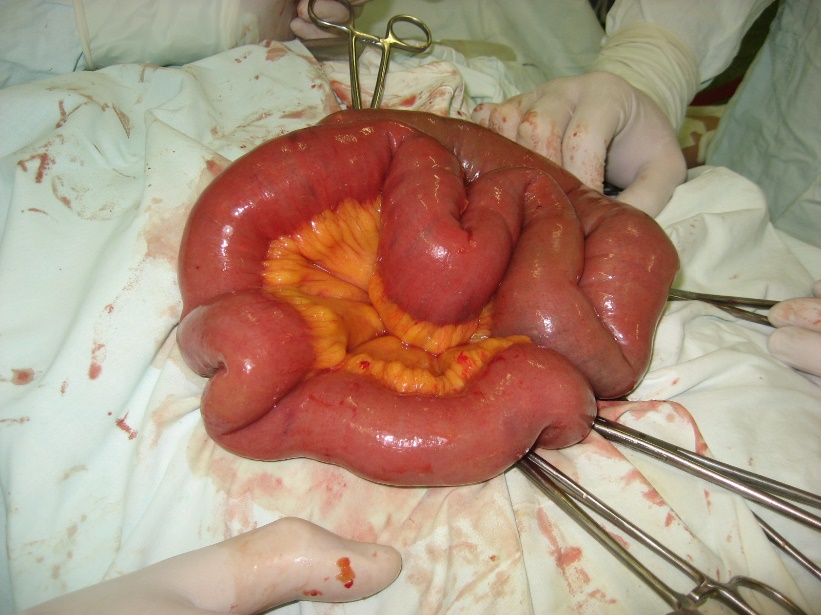
Figure 4: “Second look”: view of the small intestine after surgical intestinal revascularisation
Later in the course of the disease, the patient had frequent liquid bowel movements up to 10 times a day, these events exhausted the patient and required additional parenteral nutrition. Abdominal masses appeared in the meso-hypogastric region on the right side. There was an increase in temperature up to 38C for 5 days. Over time, the frequency of bowel movements decreased, the stool became normal, and the pain syndrome resolved. The abdominal masses significantly decreased in size, the temperature returned to normal. The patient had an episode of intestinal bleeding due to anticoagulation therapy (warfarin). Bleeding was moderate severity, controlled by medication. The patient discharged 17 days after the surgical intestinal revascularization.
03/2020 Patient A, 80 years old, admitted to the emergency room after 1 hour a sudden onset of very severe pain in the abdomen. History: ischemic heart disease, atrial fibrillation. Upon admission, the patient's status was of moderate severity. On examination, the patient was restless, complains of severe abdominal pain. Heart sounds were arrhythmic, blood pressure was 140/80 mmHg, the abdomen was without peritoneal symptoms. Intestinal peristalsis normal. Electrocardiography revealed atrial fibrillation, after abdominal ultrasound examination no additional information was obtained. An emergency computed tomography angiography was performed. Acute occlusion of SMA with small bowel ischemia has been established (Fig.5).
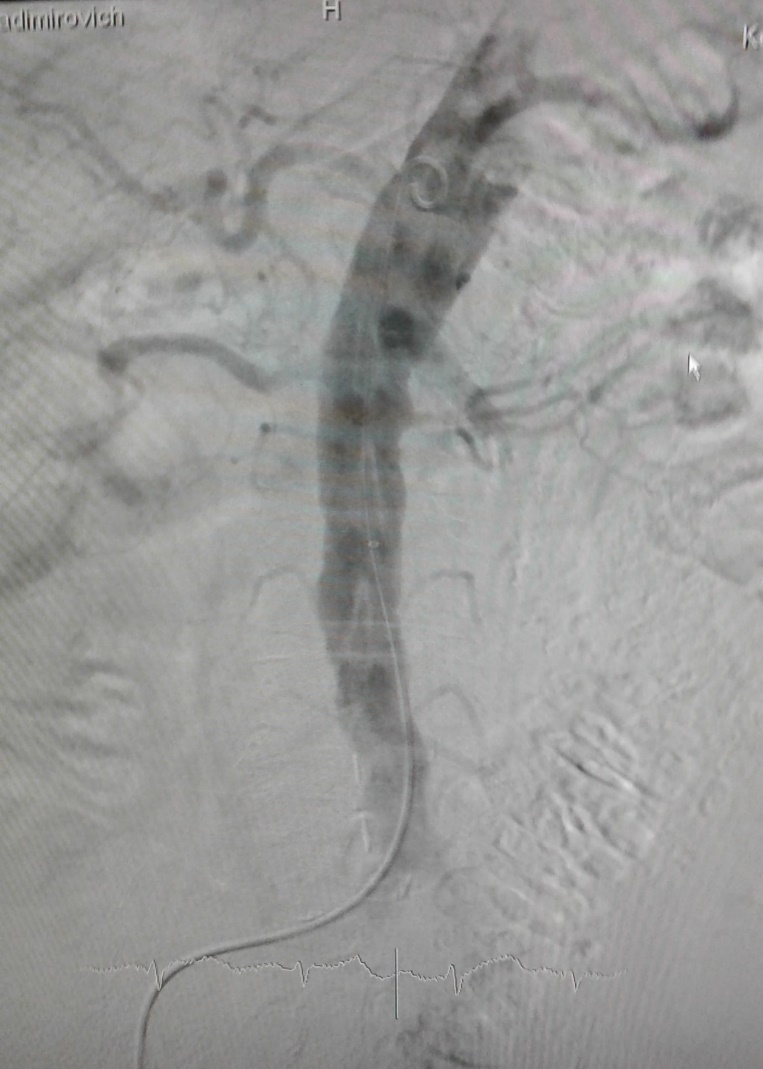
Figure 5: CT view of SMA acute occlusion.
The patient was taken to the endovascular operating room immediately. Abdominal aortography performed and the presence of acute occlusion (thromboembolus) in SMA below the origin of a. colica media confirmed. Endovascular aspiration thrombembolectomy performed (Fig.6).
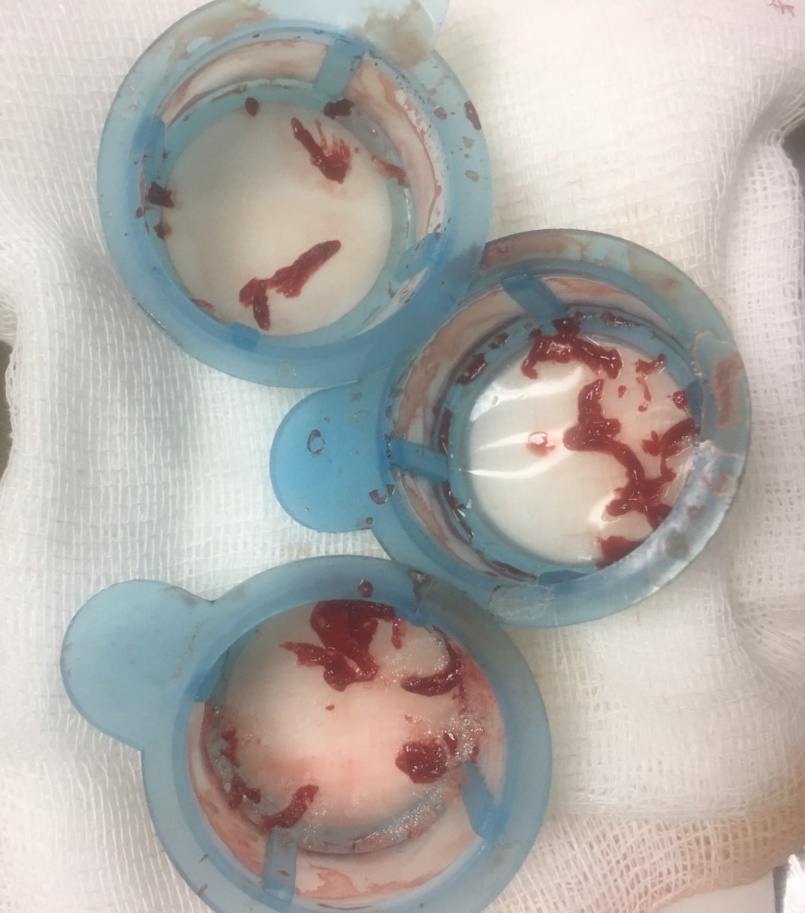
Figure 6: Thrombus aspirated from SMA.
Completion angiography control established restoration of blood flow in SMA and its branches (Fig.7).
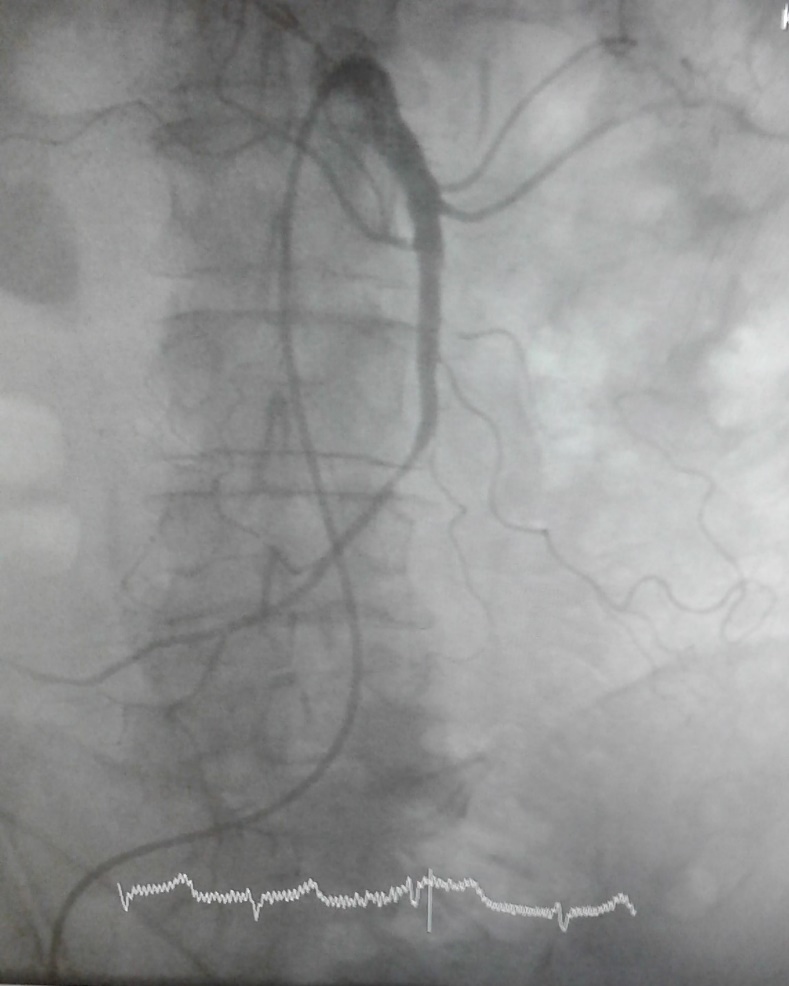
Figure 7: View of SMA after thrombus aspiration.
SMA was stented. The pain syndrome disappeared after endovascular intestinal revascularization. Second look computed tomography angiography performed on the 3rd day after the revascularization, SMA filling defects were not detected, the bowel wall accumulates contrast in all sections. The patient was discharged on the 5th day after the interventional endovascular intestinal revascularization. His anticoagulant medication (rivaroxaban) enhanced.
Conclusion. Endovascular methods for the treatment of acute abdominal ischemia have shown high efficiency and safety.
,