
Uta Fröschl, Melat Teklegiorgis, Hana Birhanu, Waltengus Birhanu *
Department of Otolaryngology, Head and Neck Surgery, Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia.
*Corresponding Author: Waltengus Birhanu, Department of Otolaryngology, Head and Neck Surgery, Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia.
Received Date: May 23, 2024
Accepted Date: June 15, 2024
Published Date: June 24, 2024
Citation: Fröschl U, Teklegiorgis M, Birhanu H, Birhanu W. (2024) “ Primary Tuberculosis Otomastoiditis In A 25-Year-Old Male; Ethiopian Case Report.”, International Surgery Case Reports, 6(2); DOI: 10.61148/2836-2845/ISCR/075
Copyright: © 2024. Waltengus Birhanu. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The number of cases of otitis media caused by tuberculosis (TB) has substantially declined. More recent studies report tuberculous otitis media rates of 0.05% to 0.9% [12]. In the early 20th century, 1.3% to 18.6% of all instances of chronic otitis media were reportedly caused by tuberculosis. World Health Organization 2019 Global Report on Tuberculosis: With 157,000 new cases of TB, Ethiopia is ranked 12th out of 30 nations with a high TB burden. Primary TB otomastoiditis is a rare presentation. This case report details the diagnosis of TB otomastoiditis in a 25-year-old man who is immunocompetent.
TB
Introduction
Tuberculosis is one of the most ancient infectious diseases afflicting mankind. It poses a theoretical threat to millions of lives globally and can cause harm to almost every organ in the human body [2].
There are two primary types of tuberculosis: the extra pulmonary kind, which affects any organ other than the lungs, and the typical pulmonary form. About 80% of instances of tuberculosis (TB) are pulmonary, which makes it the most common type of this disease. [1, 3]. Approximately 70% of cases include co-infection with HIV [1]. The larynx is the primary organ affected by tuberculosis in the head and neck; the tonsils, neck lymph nodes, middle and external ears, pharynx, mouth, and salivary glands can be affected.[4]. Jean-Louis Petit was the first to describe tubercular mastoiditis in the eighteenth century [13]. In 1853, Wilde reported about the description of TB otitis media, which included multiple perforations in the tympanic membrane, pale granulations in the middle ear cleft, and a painless, insidious onset of ear discharge [13]. Koch demonstrated the tubercle bacilli in 1892, but Politzer discussed the disease's destructiveness in 1882 [8]. Four percent of cases of head and neck TB are caused by tuberculous otitis media (TOM). 0.05–0.9% of middle ear chronic infections are caused by TOM [10]. Published case series are few in quantity since TBM is rarer.
Case Report
A 25-year-old male patient presented with left ear discharge for the last 2 years, which was thick, foul-smelling, and bloody. He has been treated at local primary hospitals with topical antibiotics, ear drops, and multiple PO antibiotic medications, but without any improvement. He also had non-pulsatile continuous tinnitus and significant hearing loss in the same ear, which worsened progressively. Otherwise, he had no history of a known co-morbid medical illness and no history of taking any immunosuppressive drugs. He had no cough, weight loss, or night sweating.
On otomicroscopic examination of the left ear, the external ear canal was filled with a foul-smelling, thick pus discharge. After performing aural toilet, there was granulation tissue visible in the external ear canal, which bled with little manipulation and was tender. The tympanic membrane was difficult to visualize (figure 1).

Figure 1: otomicroscopic finding
The right ear was normal on examination. Weber was lateralizing to the left ear, and the Rinne test was negative on the left ear and positive on the right ear. The audiogram examination showed moderately severe CHL (AC-65dB and BC-10dB), and the right ear was having normal hearing.
HRCT of the temporal bone was done, and it showed a left middle ear soft tissue attenuation mass with ipsilateral scutum blunting and widening of the prussak space. Left mastoid air cells were opacified with bony sequestrate; there was bone erosion of the mastoid cortex and sigmoid. The tegmen tympani was thinned out, and the tympanic segment of the facial nerve was difficult to comment on (Figure 2). The ossicles were eroded, which was suggestive of cholesteatoma and/or tuberculosis.
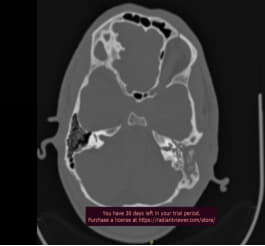
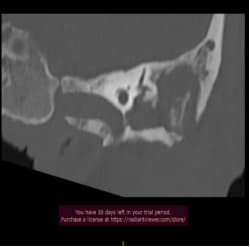
Figure 2: High resolution temporal bone CT
Brain MRI without contrast was done and showed mastoid air cell opacification with T1 iso and T2 hyper-intense signals. There was a T1 and T2 hyper-intense signal seen in the left middle ear and external auditory canal with rim diffusion restriction and rim enhancement involving the mastoid antrum and aditus, again suggestive for Tuberculosis otomastoiditis (figure 3).
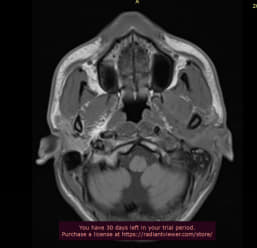
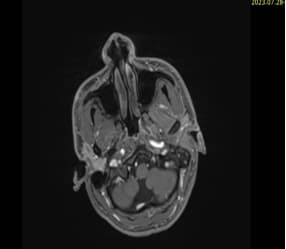
Figure 3: Brain MRI
The patient was investigated with CBC, which showed a normal result; ERS was 99 mm/hr; PICT was non-reactive; and FBS was in the normal range.
The patient was taken to the OR for exploration, and the intra-operative findings were granulation tissue and pussy discharge in the external ear canal. The posterior superior external ear canal was eroded, and there were bony sequestrate in the mastoid. Pus discharge was sent for gene X-pert examination. Multiple punch biopsies were taken from granulation tissue and sent for histopathology examination together with the bony sequestrate. Gene X-pert result detected MTB, and histopathology examination shows caseating granuloma which is suggestive for TB. After the TB confirmation, the patient started anti-TB medication.
Discussion
Our case emphasizes that Tuberculosis otomastoiditis is a rare presentation and usually difficult to differentiate from bacterial CSOM. Only about one percent of persistent ear infections are caused by tuberculosis [15].
The pathophysiology of TOM is described by three theories that are cited in the literature: a) haematogenous transmission; b) direct extension via the Eustachian tube, especially in children who drink milk contaminated with M. bovis; and c) direct implantation through a tympanic membrane perforation [3, 5, 8.10].
The classical description of tubercular otitis media includes painless, odorless otorrhea, insidious in onset, multiple tympanic membrane perforations, extensive granulation, and hearing loss [8]. The absence of pain is a characteristic feature [5].
In the early stages of TB OM, multiple perforations are rarely seen [3]. Unless cochlear involvement results due to the disease's progression, hearing loss is conductive; later, it may become mixed or sensorineural [5]. Our patient presented with the classical clinical features of tuberculous otitis media, i.e. blood mixed mucopurulent discharge, a moderately severe degree of conductive hearing loss and pale, extensive granulations in the middle ear cleft with bony sequestrate in the mastoid. Nowadays, chronic painless ear discharge is the most frequent finding, which is resistant to conventional antibiotic therapy [3].
Laboratory diagnosis of the condition may be difficult; AFB positive in ear discharge ranges from 5 to 35% [8]. culturing is more sensitive (0–44%), Although the incubation period is 6–8 weeks [3]. Histopathology analysis of the tissue from the infected ear is the only trustworthy method of diagnosis; even so, it has a 10% first false-negative rate [10]. The polymerase chain reaction (PCR) of infected otorrhea has been proposed as a potential alternate diagnostic method more recently [5]. In our patient case, GeneXpert showed positive for mycobacterium Tuberculosis and histopathology examination showed caseating granuloma.
High-resolution CT and CBCT of the middle ear cleft are helpful in identifying mastoid obliteration and bone erosions [3]. The whole middle ear cavity was filled with soft tissue, there was significant bony and ossicles erosion [10]. At an advanced stage of the disease, the eardrum or the atrium can present a granulomatous or necrotic aspect, and bony sequestrate occur frequently [14]. In our case, HRCT showed opacification of the middle ear and mastoid cavity with ossicles erosion and bony sequestrate. Due to their low sensitivity, magnetic resonance imaging (MRI) scans are unable to determine the degree of bone erosion. However, MRI scan is very helpful for differential diagnosis and to search for neurological complications of tuberculosis [3].
Surgery and anti-tuberculosis chemotherapy are the possible therapeutic options. After the development of potent anti-tuberculous treatment, the use of surgery in the treatment of tuberculous mastoiditis has significantly decreased [5]. Current indications for surgery include the treatment of a subperiosteal abscess and the removal of the sequestrate [11]. Like in our patient, bone sequesters, and granulation tissue were removed and submitted for histopathology examination. Some experts suggest that after effective Anti-TB chemotherapy, surgery can be done for reconstruction of tympanic membrane and Ossicles.
Conclusion
Primary Tuberculosis otomastoiditis is a rare clinical presentation. Diagnosis is based on a high index of clinical suspicion complemented by histopathology findings and newer techniques such as PCR. The management of this condition is primarily medical but surgical procedure can be done to take biopsy and to remove bony sequestrate.
Consent
Informed written consent was taken from the patient.