
Nida S Bham, MD 1*, Sora Ely, MD 2, Alisa Savetamal, MD, MA 3, Saral Mehra, MD, MBA 4, Brooks V. Udelsman, MD, MHS 5, Frank C. Detterbeck, MD 6, Vincent J. Mase Jr., MD 7
1Division of Thoracic Surgery, Department of Surgery, Yale School of Medicine, New Haven, CT
(0000-0001-5188-6532).
2Division of Thoracic Surgery, Department of Surgery, Yale School of Medicine, New Haven, CT.
3Trauma Surgery, Northeast Medical Group, Bridgeport Hospital, Bridgeport, CT.
4Division of Otolaryngology, Department of Surgery, Yale School of Medicine, New Haven, CT.
5Division of Thoracic Surgery, Department of Surgery, Yale School of Medicine, New Haven, CT.
6Division of Thoracic Surgery, Department of Surgery, Yale School of Medicine, New Haven, CT.
7Division of Thoracic Surgery, Department of Surgery, Yale School of Medicine, New Haven, CT.
*Corresponding author: Nida S. Bham, MD, 330 Cedar St, New Haven, CT 06510o:203-785-4931 / f:203-737-2139.
Received: March 26, 2024
Accepted: April 02, 2024
Published: May 03, 2024
Citation: Nida S Bham, Ely S, Savetamal A, Mehra S, Brooks V. Udelsman. (2024) “Tracheoesophageal Fistula after Severe Burn and Inhalational Injury.”. International Surgery Case Reports, 6(1); DOI: 10.61148/2836-2845/ISCR/071.
Copyright: © 2024 Nida S. Bham. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Tracheoesophageal fistula (TEF) is a rare complication of inhalational burn injury. While more commonly seen after chemical ingestion, there are few reports in the literature of spontaneous TEF in burn patients not related to tracheostomy.
Case: We present a case of a patient with cutaneous burn and severe inhalational injury who ultimately was found to have a tracheoesophageal fistula. In this case, diagnosis was difficult and definitive repair required a multidisciplinary approach.
Conclusion: Awareness of this possible sequela of inhalational burn injury will promote early recognition and appropriate management.
tracheoesophageal fistula; inhalational injury
Introduction
Discussion of tracheoesophageal fistulae (TEF) in the burn literature is primarily focused on TEFs resulting from endotracheal or tracheostomal intubation. There are only 3 case reports of primary spontaneous TEF following inhalational burn injury (1 adult1 and 2 pediatric2,3). The presentation of this rare complication can be difficult to recognize in patients who remain intubated and enterally tube-fed4, particularly if the usual positioning of the ETT or tracheostomy extends distal to the TEF. We present a case of TEF resulting from severe inhalational burn injury in an intubated patient.
Case Report
A 50-year-old woman was found down and presented to outside hospital with burns to bilateral upper extremities, face and neck totaling 15% body surface area (BSA) as well as inhalational injury (soot suctioned from secretions). She was intubated and transferred to the intensive care unit (ICU) at the regional burn center, where she underwent bronchoscopy through the ETT on hospital day (HD) 2. At the time extensive inhalational injuries were noted, with visible soot and necrotic respiratory epithelium extending from the trachea into the mainstem bronchi bilaterally (Figure 1).
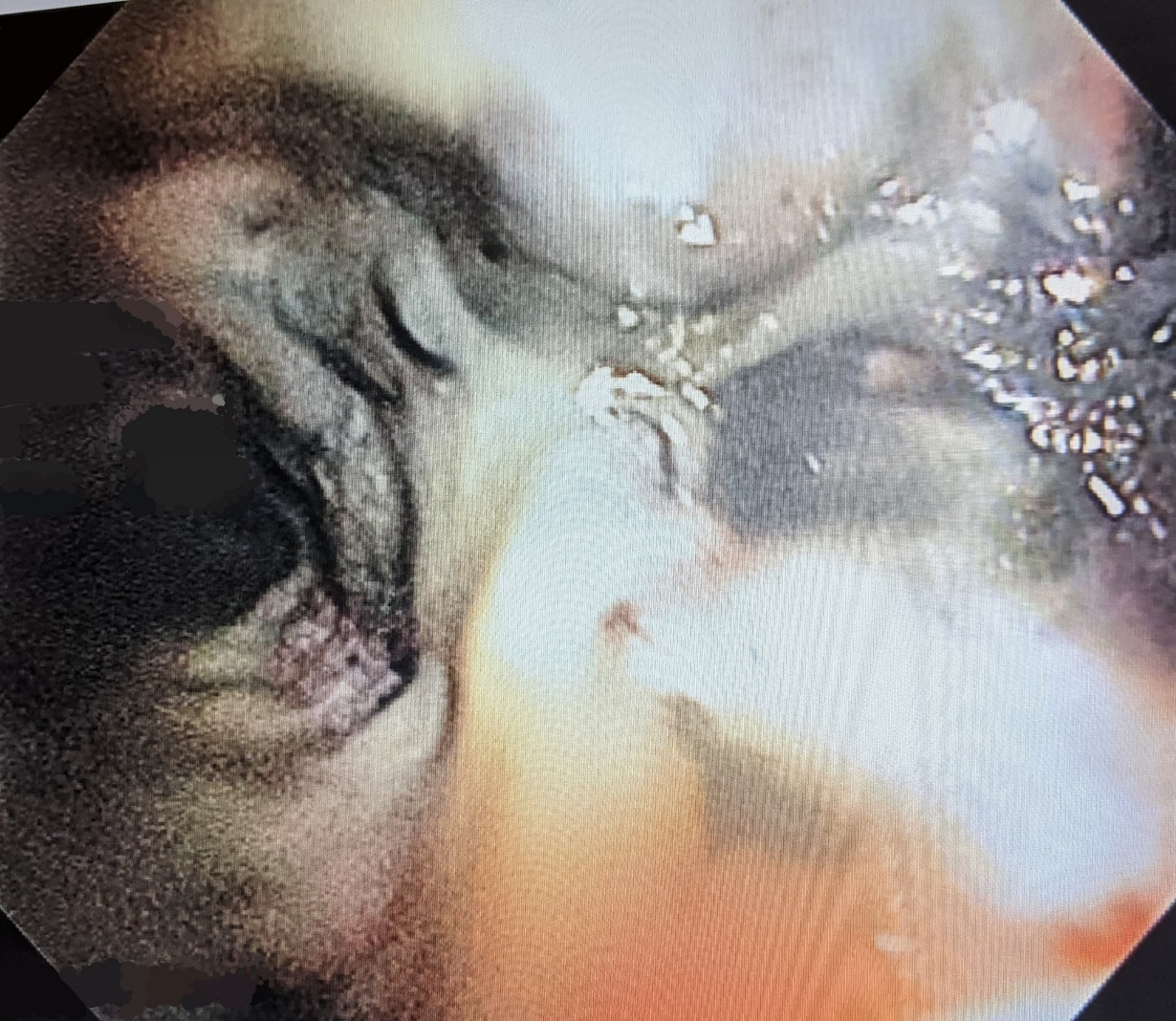
Figure 1: Initial severe respiratory inhalational burn injury on bronchoscopy.
The ETT was not manipulated during the procedure and the trachea proximal to the ETT tip was not examined. Over the following four weeks, the patient’s recovery was complicated by benzodiazepine withdrawal, agitation, intermittent gastrointestinal (GI) bleeding, blood-tinged secretions from the ETT, inability to transition to spontaneous ventilation modes, and recurrent pneumonia. She underwent bedside hybrid tracheostomy (open approach to the trachea followed by modified Seldinger insertion of tracheostomy appliance over a wire) on HD 19 without intra-procedural bronchoscopic evaluation. The tracheostomy was exchanged in the operating room on postoperative day (POD) 7, due to difficulty passing the airway suction catheter and recurrent emesis with suctioning attempts. Bronchoscopy at that time was interpreted as showing “hypergranulation tissue” partially occluding the distal opening (Figure 2A) and an extra-long appliance was placed past the area. Ultimately, on HD30, an upper endoscopy was performed to investigate the intermittent concern for GI bleed and revealed erosion of the ETT balloon into the proximal esophagus (Figure 2B), prompting a consult to thoracic surgery.
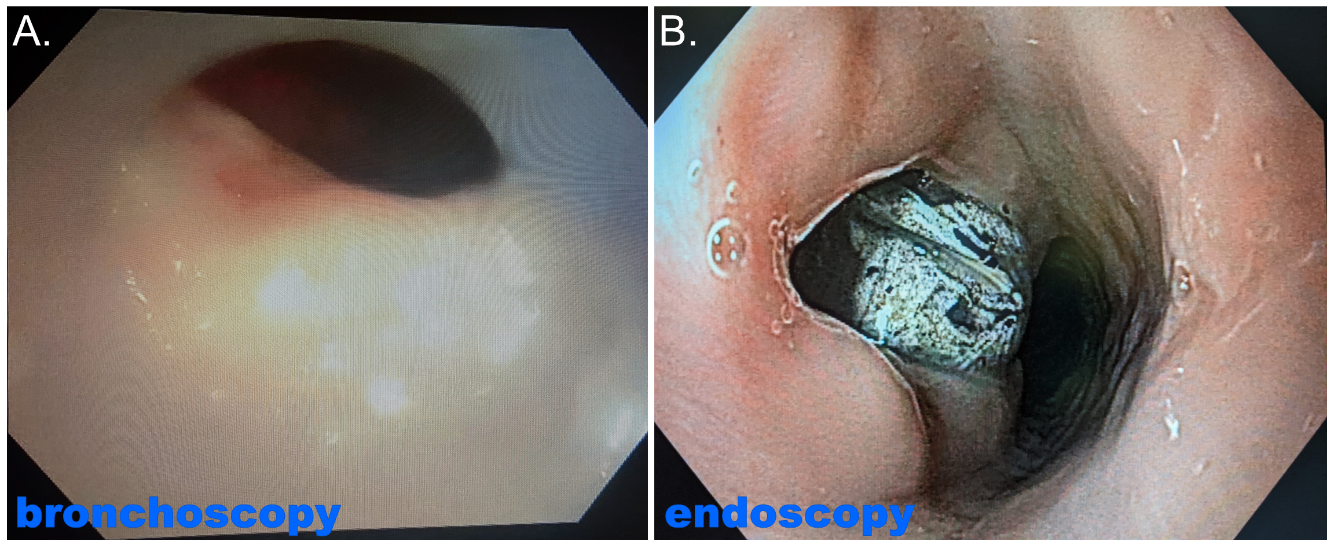
Figure 2: A) “Hypergranulation tissue” at the distal cannula on bronchoscopy during tracheostomy exchange.
B) ETT balloon within the esophagus on endoscopy.
After recognition of the TEF and consultation by our team, the patient was transferred to our main tertiary care facility and Otolaryngology was also consulted for a coordinated procedure that would include planned muscle and tissue flap coverage. Several factors needed to be addressed by our team at the time of transfer: preoperative assessment of the vocal cords; long-term nutritional/enteral access; safe and secure airway access; soft tissue/flap coverage of the repair. The patient underwent tracheoesophageal fistula takedown with segmental resection and primary re-anastomosis of the trachea, primary closure of the esophagus, strap muscle flap interposition, and locally mobilized soft tissue coverage.
At the time of her surgery, endoscopy revealed a 4cm esophageal defect approximately 16-20 cm from the incisors. Tracheoscopy and laryngoscopy revealed edematous upper airway around the cords with erythema extending down to the level of the defect. We would like to highlight that the tissue dissection for her tracheoesophageal fistula takedown was atypical; given the unique nature of her case, with inhalation injury, the planes were fused and dissection tedious secondary to extensive inflammation and necrosis. The recurrent laryngeal nerves were dissected and followed superiorly and preserved. Resection of the affected portion of the trachea permitted access and exposure to the esophageal defect, which was repaired in usual 2-layered fashion after debridement back to healthy tissue edges. This closure was reinforced with vascularized omohyoid and sternothyroid pedicled muscle flaps raised separately and placed over the esophageal closure but behind the trachea. The tracheal injury required resection of a 4cm segment beginning just distal to the cricoid cartilage. The complexity of the procedure was further increased by the unanticipated but ultimately unsurprising finding that the trachea did not mobilize as much or as readily as would be expected in other settings. We were finally able to complete a segmental resection and primary anastomosis of the trachea with running monofilament non-absorbable suture. Closure utilized the previously mentioned pedicled strap muscle interposition flaps as well as local soft tissue coverage.
She recovered well from surgery and was extubated uneventfully on POD7, and subsequently discharged about 2 weeks postoperatively to skilled nursing facility. She did, however, develop a late complication of subglottic stenosis with the fibrosis involving the vocal cords for which she is undergoing endoscopic treatment by our ENT and Interventional Pulmonology colleagues.
Comment
The imaging findings leading to the discovery of the tracheal injury were quite notable. These included a computed tomography (CT) scan of the chest 2 weeks after admission and numerous daily chest X-rays (CXRs). Review of these images suggests that the ETT balloon had changed in conformation and width over the preceding several days before diagnosis of the TEF, becoming wider and rounder suggesting expansion beyond the boundaries of the trachea (Figure 3).
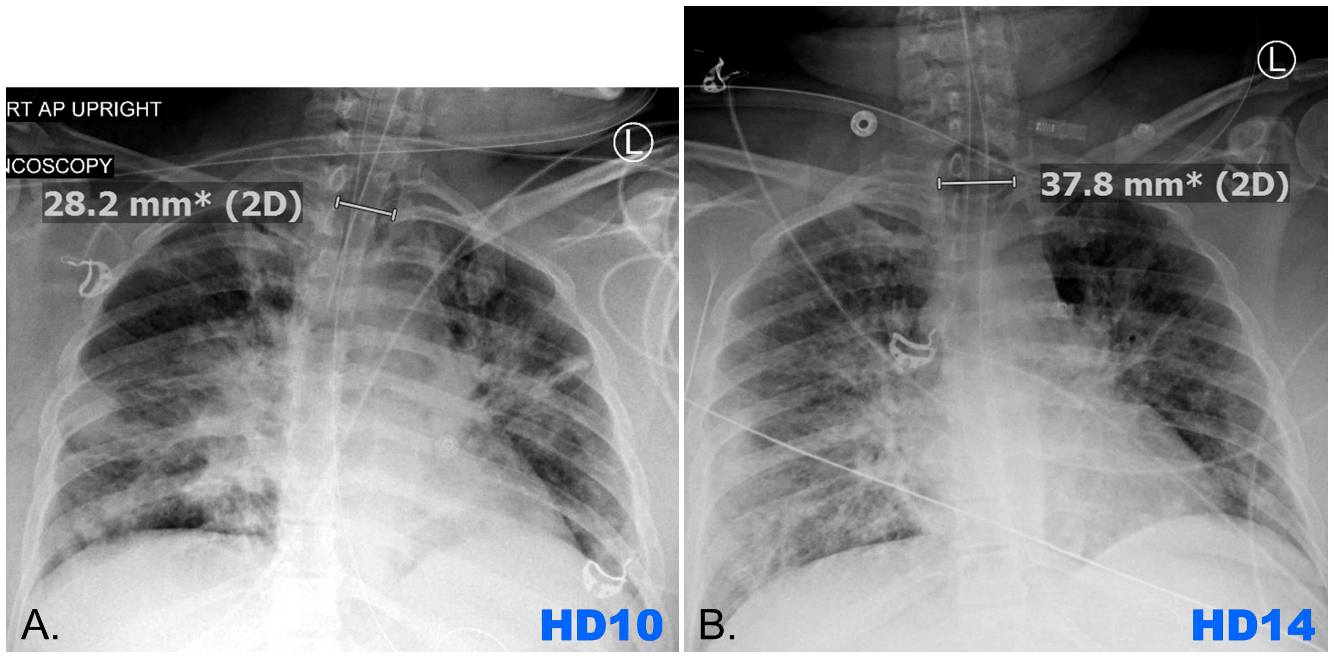
Figure 3: ETT balloon measurements on HD10 (A) and HD14 (B).
Fortunately, the patient was stable such that additional work-up, consultation, and operative planning could be undertaken before proceeding to the operating room. We suggest that heightened attention be paid to the radiographic studies of patients presenting with moderate to severe inhalation injuries, as the findings on these studies may be subtle.
The extent of damage and scarring to the trachea, even after significant review of imaging, was found to be more severe than anticipated at time of the definitive repair. The challenges of this case underscore the need for the surgical care of TEF to be undertaken at a tertiary care center with a multidisciplinary team including ENT, thoracic surgery, and, depending on institutional practice patterns, interventional pulmonology and plastic surgery. Though it was time-consuming, we found it essential to expose the normal tissue planes in order to facilitate the repair and to achieve the necessary mobilization for a primary anastomosis.
It is critical for providers to be cognizant of the degree of tracheal injury that is possible and of the potential for a TEF to occur in burn patients with severe inhalational injuries in order not to miss this serious complication. Protective strategies such as maintenance of lower than typical “safe” pressure in ETT balloons, even maintaining a small cuff leak, should be utilized5. One study of tracheostomies in 99 burn patients noted that patients who later developed TEF were older and the large majority (80%) had findings of tracheal necrosis on bronchoscopy and/or intraoperatively6. Although studies have demonstrated the safety of percutaneous tracheostomy approaches in inhalational burn patients7, use of bronchoscopy as well as selection of a hybrid or traditional open approach may be considered, as the intraoperative findings may identify patients at risk for or with TEF.
Acknowledgements: None
COI & Funding: No disclosures.
Informed Consent: Consent was obtained from the patient described in this report.