
Nathan Arboleda, MD1; Jennifer Tingley, MD1; Yu Hyon Kim, MD1
1Department of Ophthalmology and Visual Sciences, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY.
*Corresponding author:Yu Hyon Kim, Department of Ophthalmology and Visual Sciences, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY.
Received: February 05, 2024
Accepted: February 12, 2024
Published: February 26, 2024
Citation: Arboleda N, Tingley J, Yu H Kim. (2024) “Management of Submacular Hemorrhage in a Monocular Patient with Factor II Deficiency using Intravitreal Tissue Plasminogen Activator Injection and Silicone Oil.”. International Surgery Case Reports, 6(1); DOI: 10.61148/2836-2845/ISCR/070.
Copyright: © 2024 Yu Hyon Kim. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Submacular hemorrhage is a rare but visually significant diagnosis associated with a wide range of etiologies that can result in permanent decline in vision if not promptly managed. We present a case of submacular hemorrhage in a monocular patient with Factor II Deficiency that underwent surgical management utilizing intravitreal tissue plasminogen activator and silicone oil. This provided rapid inferior displacement and consistent tamponade to limit the risk of recurrent bleeding. We believe that this method is a viable surgical option in patients with submacular hemorrhage with an elevated risk of recurrence.
subretinal hemorrhage; submacular hemorrhage; silicone oil; tissue plasminogen activator; factor II deficiency
Introduction
Submacular hemorrhage (SMH) is an uncommon but vision threatening diagnosis, usually associated with diseases that result in choroidal neovascularization (CNV), including Age-related Macular Degeneration (AMD), polypoidal choroidal vasculopathy (PCV), high myopia, and angioid streaks. However, submacular hemorrhage can also more rarely be a complication of retinal macroaneurysms, trauma, and blood dyscrasias.
If left untreated, submacular hemorrhage can lead to irreversible damage to the photoreceptors secondary to clot contraction, oxidative stress from the iron rich hemoglobin, and impaired diffusion of oxygen and nutrients through the blood [1]. Animal studies suggest that the extent of injury is correlated with the chronicity of submacular hemorrhage [2]. Operative management has typically focused on AMD associated SMH, and over the past few decades the range of treatment combinations has grown to include vitrectomy, tissue plasminogen activator (tPA), along with a method of removing or displacing the submacular hemorrhage such as direct drainage through retinotomies or retinectomies, RPE-choroid patch grafting, or pneumatic displacement [3-8].
This case involves a monocular patient with factor II deficiency, which is associated with an elevated bleeding risk. Subretinal tPA was utilized to liquidate the hemorrhage, which was then displaced with silicone oil as an alternative to pneumatic displacement to improve immediate post-op vision in a monocular patient.
Case Report
A 67-year-old patient with a past medical history of factor II deficiency, type 2 diabetes, hypertension, and chronic obstructive pulmonary disease presented with decreased vision and a new ‘curtain-like’ shadow in the right eye after a severe episode of coughing.
Her past ocular history included left eye enucleation. Patient reported a similar episode of curtain-like vision in the left eye, retinal hemorrhage, and subsequently underwent left eye enucleation.
On exam, visual acuity was count-fingers, which had decreased from 20/25 at a routine exam four months prior. A dilated fundus exam revealed a large subretinal hemorrhage involving the temporal macula with an inferior bullous retinal detachment (Figure 1).
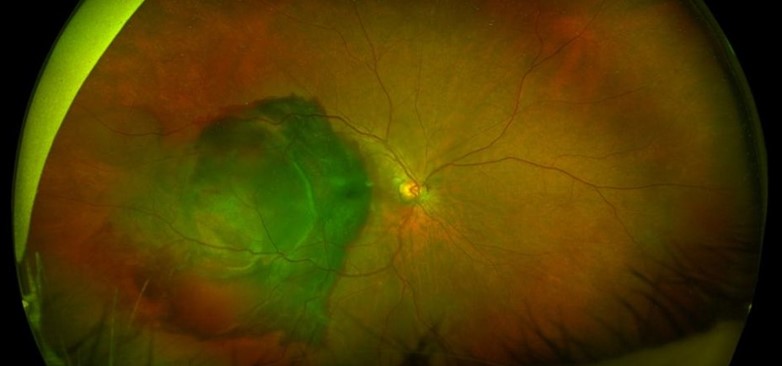
Figure 1. Fundus photo, Pre-operative: Macula involving subretinal hemorrhage with an inferior bullous retinal detachment.
After preoperative intravenous plasma infusion, urgent pars plana vitrectomy was performed with intraoperative subretinal tissue plasminogen activator injection using a 38-gauge needle. To maximize immediate post-operative vision in this monocular patient, 5,000 centistoke silicone oil was chosen for tamponade and hemorrhage displacement rather than pneumatic displacement.
The submacular hemorrhage was effectively displaced inferiorly (Figure 2).
 Figure 2. Fundus photo, post-operative day 2: Complete displacement of submacular hemorrhage after silicone oil injection, with residual inferior bullous detachment.
Figure 2. Fundus photo, post-operative day 2: Complete displacement of submacular hemorrhage after silicone oil injection, with residual inferior bullous detachment.
A small residual pigment epithelial detachment was present on immediate post-operative imaging that has continually decreased in size with resolution by follow-up 7 months after surgery (Figure 3).
 Figure 3A. Pre- and post-operative OCTs: Showing resolution of macula off submacular hemorrhage after surgery, with residual Pigment Epithelial Detachment (PED) seen 2 weeks post-op. The PED was with near complete resolution by 6 weeks post-op.
Figure 3A. Pre- and post-operative OCTs: Showing resolution of macula off submacular hemorrhage after surgery, with residual Pigment Epithelial Detachment (PED) seen 2 weeks post-op. The PED was with near complete resolution by 6 weeks post-op.
 Figure 3B. Post-op month 7. Resolution of previously seen PED, with a small amount of intraretinal fluid inferior to the fovea. Significant atrophy of the ellipsoid zone.
Figure 3B. Post-op month 7. Resolution of previously seen PED, with a small amount of intraretinal fluid inferior to the fovea. Significant atrophy of the ellipsoid zone.
The patient had an excellent anatomic outcome with minimal residual hemorrhage and vision improved to 20/200 with silicone oil in place (Figures 4-5).
 Figure 4. Fundus photo, 6 weeks post-operative: inferotemporal non-macular heme seen.
Figure 4. Fundus photo, 6 weeks post-operative: inferotemporal non-macular heme seen.
 Figure 5. Fundus photo, 7 months post-operative: Resolution of inferiorly displaced subretinal hemorrhage.
Figure 5. Fundus photo, 7 months post-operative: Resolution of inferiorly displaced subretinal hemorrhage.
Discussion
Submacular hemorrhage has a poor visual prognosis with size, chronicity, and poor visual acuity on presentation correlated with final visual outcome [8-10]. Evaluation of the effectiveness of any given operative technique in the management of submacular hemorrhage is confounded by the fact that submacular hemorrhage may be caused by a wide range of etiologies. In a review of studies comparing different management techniques for traumatic submacular hemorrhage, Casini et al. found good outcomes of SMH of all operative techniques when comparing intravitreal tPA, intravitreal tPA with pneumatic displacement, subretinal tPA with pneumatic displacement, or pneumatic displacement alone [8]. Subretinal tPA with pneumatic displacement was found to be the most effective in optimizing visual outcomes. However, of note, a majority of published literature consisted of small studies and case reports, limiting the generalizability of any given study. The use of silicone oil in displacement of submacular hemorrhage has been reported in the literature, however it is typically utilized in tandem with a temporal retinectomy, temporal retinotomy, or the less commonly utilized RPE-choroidal patch graft [11-14].
This case remains unique as the patient had a substantial risk for rebleeding from underlying factor II deficiency. Subretinal tPA was needed to maximize its fibrinolytic action on the hemorrhage, and to allow for rapid displacement out of the macula. Although subretinal tPA combined with pneumatic displacement would have been sufficient to displace the submacular hemorrhage, the patient at this time was monocular from a previously uncontrolled bleed, and priority was placed on maintaining useful vision in her remaining eye. Silicone oil provides a long term, consistent tamponade compared to pneumatic displacement to protect the eye from recurrent bleeding. The anatomic outcome after surgery has been excellent, and the patient has had improvement in her vision 6 months after surgery.
Conclusion
As there is a lack of clear guidelines on management of SMH we advocate for the use of subretinal tPA with silicone oil in patients with a substantial lifelong risk of recurrence. The subretinal tPA allows for a more concentrated fibrinolysis and displacement of the SMH, with silicone oil to allow for rapid displacement of the SMH with sustained tamponade. We believe this provided the best possible anatomic and visual outcome given these specific circumstances.
Conflict of Interest Disclosure(s)
The authors have no financial, commercial, or personal conflicts of interests to disclose.
Author Contributions
(I) Conception and design: All authors
(II) Administrative support: All authors
(III) Provision of study materials or patients: All authors
(IV) Collection and assembly of data: All authors
(V) Data analysis and interpretation: All authors
(VI) Manuscript writing: All authors
(VII) Final approval of manuscript: All authors
Acknowledgements: None.
Financial Support and Sponsorship: None.