International Surgery Case Reports
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Zehao Guo1, Xumei Kang2, Yufei Duan3, Ling Zhang3, Senlin Yang3, Yan Cao3, Ting Wu3 Junwang Zhang3,
1Gastroenterology Department, the graduate student of Shanxi Medical University.
2Imaging Department, Second Hospital of Shanxi Medical University.
3Gastroenterology Department, the Second Hospital of Shanxi Medical University
*Corresponding author: Junwang Zhang, The Second Hospital of Shanxi Medical University, Gastroenterology Department, No 236, Wuyi Road, Xinghualing District, Taiyuan City, Shanxi Province, China.
Received date: September 09, 2022
Accepted date: September 23, 2022
published date: October 10, 2022
Citation: Guo Z, Kang X, Duan Y, Zhang L, Yang S, Cao Y, Ting Wu, Zhang J, (2022) “The Size of Chippings of Phytobezoar May Be an Important Indicator of The Prognosis of Endoscopic Fragmentation Treatment: A Report of Two Cases”. International Surgery Case Reports, 4(3). DOI: http;//doi.org/11.2022/1.1058.
Copyright: © 2022 Junwang Zhang. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Phytobezoar is a common and significant gastrointestinal disease. It often causes several severe complications. Endoscopic fragmentation is an ideal treatment modality for phytobezoars. However, the result is not very certain. We report two cases that reveal the prognostic value of phytobezoar fragment size. In one case, the patient was treated with more elaborate lithotripsy under endoscopy. The transverse diameter of the largest fragment was ≤ 2 cm. The patient recovered with no complications. But in another case, the patient was treated with two sessions of rough lithotripsy. The transverse diameter of the largest fragment was still > 2.0 cm. The obstruction occurred in the duodenum and ileum successively. Finally, the patient underwent exploratory laparotomy removing the phytobezoar and recovered with no complications. Endoscopy lithotripsy is a safe option for phytobezoars; however, the size of chippings may be a crucial determinant of treatment outcome.
Introduction
A phytobezoar is an indigestible conglomeration trapped in the gastrointestinal tract. It is a relatively common, hard, and large subtype of bezoar. It attaches to the gastrointestinal tract and often causes severe complications, such as gastric outlet obstruction, ileus, ulceration, hemorrhage, and perforation [1]. For patients with phytobezoars, several treatment options [2] exist, including pharmacotherapy, surgery, and endoscopic lithotripsy. With the development of digestive endoscopy, non-invasive endoscopic lithotripsy has become an ideal treatment modality for phytobezoars [3]. However, the efficacy of endoscopic lithotripsy may be affected by various factors such as the fragment size, texture, and hardness of the phytobezoar. Among these factors, the size of chippings may be one of the important predictors of prognosis. If the lithotripsy procedure is not adequately performed, such that the diameter of fragments is greater than the lumen diameter, the desired treatment effect cannot be achieved. In this paper, we present two cases of phytobezoar that we encountered at our hospital, which confirm the prognostic importance of the size of phytobezoar chippings.
Case Reports
Case 1
Patient History
A 72-year-old woman was admitted to our hospital because of a one-month history of nausea and vomiting. She had eaten approximately 20 persimmons at once prior to the onset of her symptoms. She began to experience nausea, anorexia, and abdominal distention. After 2 weeks, she visited a local hospital. Gastroscopic examination revealed a gastric calculus (approximate dimensions, 6.0 × 5.0 × 5.0 cm) (see figure 1-A). The doctor performed initial lithotripsy under endoscopy with a big snare. The entire bezoar was broken into two main parts, but the size of one large part was still approximate 5.0 × 5.0 × 4.0 cm after lithotripsy (see figure 1 -B). Subsequently, the patient began to drink 200 ml of Coca-Cola [4] three times daily, but the vomit was aggravated and she could not eat anything. One week later, she felt weak and tired, so she was admitted for further diagnosis and treatment in our hospital.
Clinical Findings
The patient was conscious and slightly dehydrated. Her vital signs were stable and normal. Abdominal examination showed no obvious positive signs. After admission, the patient was administered a proton pump inhibitor and fluid replacement therapy. A plain abdominal film revealed a high-density shadow with dimensions 5.0 × 4.5 cm in the upper abdomen (see figure 1-C). A second gastroscopic examination revealed yellowish-green columnar stones (approximate dimensions, 5.0 × 4.0 × 4.0 cm) trapped in the horizontal part of the duodenum with little motility (see figure 1-D).
Treatment and Outcomes
Before lithotripsy commenced, written informed consent was obtained from the patient. During gastric endoscopic examination, we made every effort to use a polypectomy snare to break the phytobezoar into pieces. Due to the narrow space and distant location in the duodenum, we could not loop the stone and finally had to strip the surface material from the phytobezoar with alligator forceps. The remaining part of the bezoar was still 4.0 × 3.5 × 3.5 cm in size. Oral Coca-Cola therapy was continued. The next day, the dense shadow in the duodenal horizontal segment had migrated into the jejunum, the patient’s vomiting stopped, and her general condition improved. After one week, the vomit recurred, and the plain abdominal radiograph revealed a high-density shadow embedded in the ileum and proximal intestine dilated with accumulated fluid and air (see figure 1-E). The patient was diagnosed with a mechanical ileus. Therefore, an exploratory laparotomy was performed. Intraoperatively, an obstructive phytobezoar at approximately 70 cm proximal to the ileocecal region was removed. Its approximate dimensions were 3.8 × 3.5 × 3.0 cm. Postoperatively, the patient recovered smoothly without any complications.

(A) the phytobezoar in the fundus of stomach. (B) the phytobezoar was roughly broken at first time. (C) the phytobezoar was incarcerated in the duodenum in plain abdominal radiograph (black arrow displayed). (D) the phytobezoar was displayed in duodenum under endoscopy. (E) the phytobezoar was embed in ileum in abdominal X-ray plain film two weeks later (black arrow displayed).
Figure 1 : the migration process of the phytobezoar in case 1
Case 2
Patient history
A 57-year-old woman was admitted to the hospital for long-term abdominal distension and intermittent epigastric pain. She, too, had eaten more than 20 persimmons at once 3 weeks prior to hospital admission. Her regular food intake had reduced by half, but she experienced no nausea or vomiting. The patient had taken an oral proton pump inhibitor and a gastric mucosal protective agent for 1 week. However, her symptoms failed to resolve, and she was admitted to our hospital.
Clinical Findings
On physical examination, her abdomen was soft on palpation. Apart from an intra-abdominal mass of approximately 8.0 × 7.0 cm in size, there was no other positive sign. A plain abdominal film revealed a large upper abdominal mass. Gastroscopy revealed hard, spherical, brown stones (approximate dimensions, 6.0 × 5.0 × 5.0 cm) in the gastric fundus (see figure 2-A), which could roll in the gastric lumen. There was an ulcer of approximately 2.5 × 2.0 cm in the gastric angle.
Treatment And Outcomes
Written informed consent was obtained from the patient. We performed an endoscopic lithotripsy. First, we dug a 0.5 cm deep groove on the surface of the bezoar with forceps. We then placed a piece of nylon wire [5] into the groove on the bezoar’s surface through a biopsy channel, where we pulled both ends of the nylon wire forcibly, resulting in the large phytobezoar separating into two pieces. We then used the nylon wire to split the stone fragments repeatedly, with all the stone fragments broken into many pieces, having a lateral diameter smaller than 2 cm (see figure 2-B). The entire procedure lasted approximately 70 min. Two days later, the patient drained a large amount of dark green feces and began having a liquid diet. The patient was discharged on the fifth postoperative day without complications.
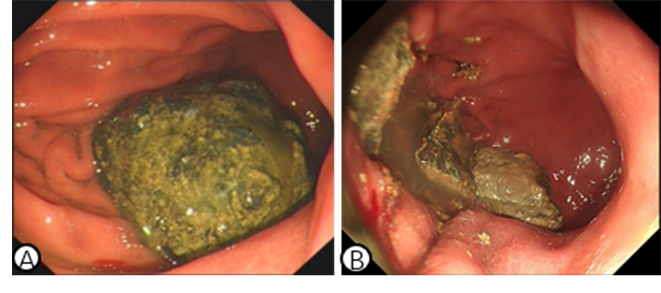
(A) the state before lithotripsy. (B) the phytobezoar was elaborately fragmented.
Figure 2: the phytobezoar in the stomach in case 2
Discussion
Phytobezoar is an eating disorder type of disease. Pharmacologic treatment has a low cure rate of approximately 23.5% [6]. Endoscopic lithotripsy has a success rate of approximately 89.7% [7]. Surgical treatment is the most effective method, with a high success rate of approximately 98.1% [7]; however, the trauma is extensive, and the rate of acceptance among patients is low [8]. Here, we have reported two cases of gastric calculi in patients without a significant medical or abdominal surgery history. In both cases, the stones were larger than 5 cm. One patient was treated with two sessions of rough lithotripsy in a different hospital. The transverse diameter of the largest fragment was still ≥2.0 cm. The obstruction recurred in the duodenum and ileum. Finally, the patient had to undergo exploratory laparotomy. Intraoperatively, the stone was removed, and the patient recovered uneventfully. The second patient was diagnosed in our hospital and treated with more elaborate lithotripsy under endoscopy. The transverse diameter of the largest fragment was less than 2 cm, and no subsequent complications occurred. The fragment size of phytobezoar may be an important indicator of the effect of endoscopic treatment.
The small intestine is divided into the duodenum, jejunum, and ileum. The diameter of the duodenum is the largest (3.5 ± 0.5 cm), while that of the ileum is smaller (2.0 ± 0.5 cm) [9]. Theoretically, to avoid obstruction of the distal gastrointestinal tract caused by incomplete lithotripsy, the transverse diameter of gastric stone fragments should be smaller than 2.0 cm. There is no universally accepted standard for treatment at present.
The stomach is more suitable for lithotripsy. In the human alimentary system, the stomach has the largest diameter and space. It is, therefore, suitable for the physician to strive for complete lithotripsy. The duodenal cavity is narrow and deep, and it is unsuitable for lithotripsy. In the first case, the residual remnant stones were embedded in the horizontal part of the duodenum. We could not crush the stone to the state of the transverse diameter less than 2 cm. Thus, if possible, the phytobezoar should be fragmented in the stomach.
Lithotripsy, however, should be performed with adequate preparation, not in haste. If the lithotripsy is incomplete, subsequent complications of gastrointestinal obstruction may occur. According to a previous report, most cases of duodenal obstruction caused by stones required surgical removal [10].
Since our conclusions are based on only two case studies, more studies are required for validation. Moreover, the treatment outcomes may be influenced by race and custom of the patients.
In conclusion, the size of chippings of phytobezoar may be an important indicator of the prognosis of lithotripsy treatment; the transverse diameter of the fragments should be less than the lumen diameter.
Acknowledgement
We would like to express our gratitude to the endoscopists and nurses from our endoscopy center who contributed to the management of patient.
Ahthor Contribution
Zehao Guo collected the data and wrote the initial draft of the manuscript. Kang Xumei, Senlin Yang, contributed to analysis and interpretation of data. Duan Yufei, Zhang Ling, Yan Cao and Ting Wu were accountable for investigating and resolving all aspects of the work that related to the accuracy or integrity. Junwang Zhang reviewed the manuscript.
Conflict Of Interests: All authors declare no conflicts of interest for this article.
Funding Information: The authors declare that this study has received no financial support.