International Surgery Case Reports
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Messian Gallouo*, Austen Clehaude DibingueTsikambu, Hissein Hagguir, Ali Hannaoui, Amine Moataz, Mohammed Dakir, Adil Debbagh, Rachid Aboutaieb
Department of Urology, CHU Ibn Rochd, Casablanca, Morocco
*Corresponding author: Messian Gallouo, Department of Urology, CHU Ibn Rochd, Casablanca, Morocco.
Received date: March 15, 2022
Accepted date: March 25, 2022
published date: April 11, 2022
Citation: Gallouo M, Austen Clehaude DTsikambu, Hagguir H, Ali Hannaoui, Moataz A, Dakir M, Adil Debbagh, Aboutaieb R. (2022) “Intraperitoneal Bladder Rupture After Road Trafic Accident”. International Surgery Case Reports, 4(2). DOI: http;//doi.org/11.2022/1.1050.
Copyright: © 2022 Messian Gallouo. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
We are reporting a 38-year-old drug addicted man’ victim of a road trafic accident resulting in post-traumatic intra-peritoneal bladder rupture . The diagnosis was suspected by the total macroscopic hematuria and confirmed by uroscanner. Our managment consisted of surgical exploration and reparation of the bladder breach
Introduction :
The urinary bladder is a reservoir that is well protected from external trauma due to its deep location in the bony pelvis specially when it’s empty. Once its filled, it becomes abdominopelvic and very vulnerable to injuries .A closed urinary bladder trauma most often results from a high-energy impact and is associated with injury to other organs. In 2% of cases, abdominal trauma includes bladder rupture (1). An arly recognition and proper management would prevent the early complications such as sepsis, peritonitis, urinoma and renal failure due to peritoneal resorption of urine. Cystoscanner is the refered examination as it allows to determine the lesion and as well as the type the bladder rupture whether it’s extra- or intra-peritoneal character and to search for associated lesions(2)(3). Through a review of the literature, we are reporting a rare case of post-traumatic intraperitoneal bladder rupture revealed by a macroscopic hematuria. We will discuss the epidemiological, diagnostic and therapeutic aspects.
Medical observation :
This is about a 34 year old male patient, who had a past medical history of left colostomy for fourniers gangrene of digestive tract origin realised 5 years ago. The patient was a victim of apublic road trafic accident 10 hours before the admission with a cranio-abdominal impact point causing a cranial trauma and hypogastric pain without initial loss of conciousness,this scenario was followed by an immediate total clotting hematuria leading to an acute urine retention before the emergency consultation . The clinical examination revealed a conscious patient, eupneic, with a normally colored conjunctiva. Urogenital examination found a scar in the left iliac fossa (colostomy), a distended hypogastric region with superior convexity which was painful to palpation. The rest of the examination was unremarkable. Renal profile was slightly impaired with a blood creatinine level at 16 mg/L. Urea: 0.28 g/L, Hb: 11 g/dl. The patient was sent for an injected uro-scanner (with contrast medium) which showed a parietal defect at the level of the bladder dome measuring 3 cm with intraperitoneal leakage of contrast medium at the delayed stage images (figure 1), classified as grade 4 according to the AAST classification. Facing this intraperitoneal bladder rupture, we took the patient directly to the operating room. The surgical exploration found a 3cm urinary bladder breach at the level of the bladder dome (figure 2) with a small-amount of peritoneal effusion (uroperitoneum). A one-centimeter mesosigmoid lesion was also objectified in the exploration (figure 3). The bladder lesion was sutured in 2 planes with Vicryl (0) suture after aspirating and an abundant washing of the uroperitoneum (figure 4) . A 22 fr triple way- urinary catheter was placed before suturing the urinary bladder and two surgical drains were placed : One at the level of the space of Retzus and the other one was at the level of the pouche of Douglas. The mesosigmoide lesion was respected. The patient was put on broad spectrum antibiotics. The post-operative course was simple. A cystography was performed after 14 days from the surgery which did not reveal any abnormality (figure 5). Thus the removal of the bladder catheter was indicated and the urination after was preserved without hematuria.

Figure 1 : uroscanner showing a bladder parietal defect with extravasation of the contrast medium into the abdominal cavity
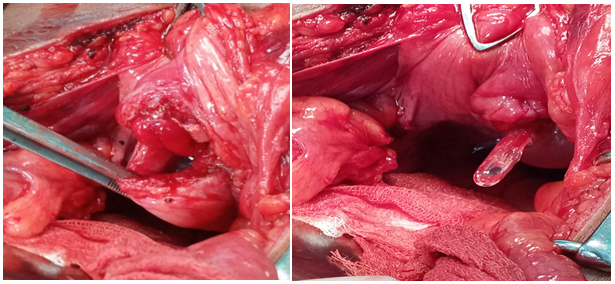

Figure 2 : Breach at the bladderdomeshowing exit of the urinarycatherthrough thebreach
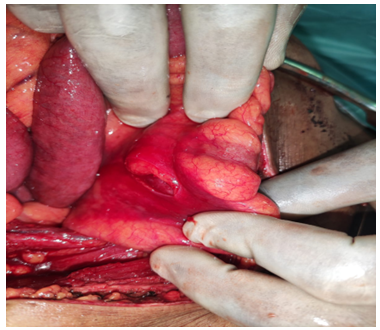
Figure 3 : lesion of the mesosigmoide
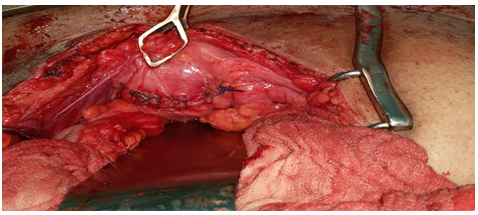
Figure 4 : cystorraphy

Figure 5 : cystography not revealing extravasation of the injected contrast product(intact bladder)
Discussion :
Bladder injuries can be intraperitoneal, extraperitoneal, or mixed (4). Bladder repletion and pelvic fracture are the two risk factors that promote bladder injury. Intraperitoneal ruptures occur during minimal trauma to a full bladder and the lesions are located preferentially at the level of the bladder dome (5). Fractures of the pelvis are responsible for bladder injuries by piercing the bladder wall by the bone fragments or splinters during a very violent trauma (1)(6). The clinical presentation of bladder injuries ranges from non-specific abdominopelvic pain to symptoms of an acute abdomen. Macroscopic hematuria and the diurese are the symptoms to ask for (7)(8)(9). Our patient consulted for a total clotting hematuria complicated by acute retention of urine. An elevated blood urea and creatinine level is explained by the peritoneal absorption of urine as found in our patient. The closed bladder trauma with hematuria associated with a pelvic fracture are the basis of the diagnosis and constitute the indication for radiological examinations(10). The cysto-scanner is the refered examination because it allows to determine the lesion and its extra peritoneal or intraperitoneal characters and also allows to look for associated lesions and to make the AAST classification (2)(3). Bladder injuries are mainly of four types : bladder contusion, extra peritoneal bladder rupture, intraperitoneal bladder rupture and bladder neck avulsion. Intraperitoneal rupture is suspected by extravasation of contrast medium into the parieto-colonic gutters, the space of Douglas, between the digestive tracts. In the absence of CT, cystography has a very good specificity and sensitivity for the detection of lesions. In our patient, the uro-scanner showed a parietal defect at the level of the bladder dome measuring 3 cm with leakage of the contrast medium into the peritoneal cavity at the delayed stage images. Therapeutic management depends on the severity of the condition as defined by the AAST (11), and the signs of severity must be initially detected and corrected. Surgical treatment is indicated for : grade 3, 4 and 5 lesions as well as perforations by a bony fragment and associated vaginal or rectal lesion(12). The lesion is sutured in one or two planes with absorbable sutures after trimming the contused tissue. Bladder watertightness can be tested by a retrograde filling of the bladder through a urinary catheter and then a pelvic drain is also put in to assess post-operative urine leakage (13)(10)(14). Conservative treatment is based on drainage through a urinary catheter for a few days and its only indicated for grades 1 and 2. Our treatment consisted of surgical exploration by trimming the soft tissues, then cystorraphy by two planes with a perfect watertightness test, then placement of two drains at the level of the cul de sac of Douglas and the space of Retzis(3). The evolution is favorable if the bladder injury is diagnosed early and managed appropriately. Close monitoring of the patients must be undertaken and broad spectrum antibiotic therapy is necessary to maintain sterile urine and reduce the risk of pelvic abscess. Cystography had been performed on the 14th day before removing the catheter as stipulated by some authors [15).
Conclusion
Post traumatic bladder rupture is rare but must be Suspected in front of post-traumatic macroscopic hematuria and or pelvic fracture. Cysto-scanner is the clue in case of doubt about a bladder injury. In case of intra-peritoneal bladder lesion ; surgical exploration is the rule