International Surgery Case Reports
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Zsofia Horvath MD1, Michele Marengo MD2, Fabio Garofalo MD1, Francesco Mongelli MD1*
1 Surgery, Ospedale Regionale di Lugano, Lugano, Switzerland
2 Surgery, Ospedale La Carità, Locarno, Switzerland
*Corresponding author: Francesco Mongelli, MD. Lugano regional Hospital, via Tesserete 46, 6900 Lugano, Switzerland.
Received date: March 09, 2022
Accepted date: March 18, 2022
published date: March 22, 2022
Citation: Horvath Z, Marengo M, Garofalo F, Mongelli F. (2022) “Intestinal Malrotation: A Rare Pathology Discovered During a Conversion from Sleeve Gastrectomy to Laparoscopic Gastric Bypass”. International Surgery Case Reports, 4(2). DOI: http;//doi.org/11.2022/1.1049.
Copyright: © 2022 Francesco Mongelli. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Intestinal malrotation is a rare first-presentation pathology in adulthood; most of the time it is discovered during the first years of life. If asymptomatic, it incidentally found during operations or diagnostic imaging (Ultrasound, CT-scan, upper GI contrast study). We present a clinical case of a 31-year-old female who was admitted for a conversion of a sleeve gastrectomy into gastric bypass. Intraoperatively, an intestinal malrotation was unexpectedly discovered. We were able to proceed with our planned operation notwithstanding the difficulty to create the anastomoses, inverted respect to the traditional way. To our knowledge, this is the first report of such anomaly during bariatric revisional surgery; a challenge many bariatric surgeons may have to face off with during their career.
Introduction
An intestinal malrotation is a rare disease, sporadically it is firstly found in adulthood. It has a prevalence of approximately 0.17 percent [1]. It is a congenital anomaly of the intestines and there are several types of rotational anomalies, ranging from a not-quite normal intestinal position to complete nonrotation. The most common variations are nonrotation, reverse fixation, and malrotation [2]. In case of malrotation, patients have typically the ligament of Treitz and jejunum on the right side, the whole position of the ileum is a mirror image of the normal and the ascending colon is medialized [2]. Because of its rarity, the diagnosis of intestinal malrotation is often delayed in adult patients and, therefore, associated with increased morbidity [3]. In most of the cases it is incidentally found during routine examination, on CT scans or in the operating theatre [4]. The knowledge of such uncommon condition is important as surgeons may have to face off with it during their carrier.
We present the case of a young patient, in which an intestinal malrotation was found during a conversion of a sleeve gastrectomy into a gastric bypass.
Case report
A 31-year-old female who underwent a sleeve gastrectomy in 2015 with no complications reported. During the first 6 months dropped the body mass index (BMI) dropped 11 points (from 37.4 kg/m2 to 26.1 kg/m2). Six years after surgery, she was referred again to our multidisciplinary bariatric center for a weight regain of 26 kg (actual BMI was 38.7 kg/m2). A conversion of the sleeve gastrectomy to laparoscopic gastric bypass was planned. During the surgery, an intestinal malrotation was found (Figure 1).
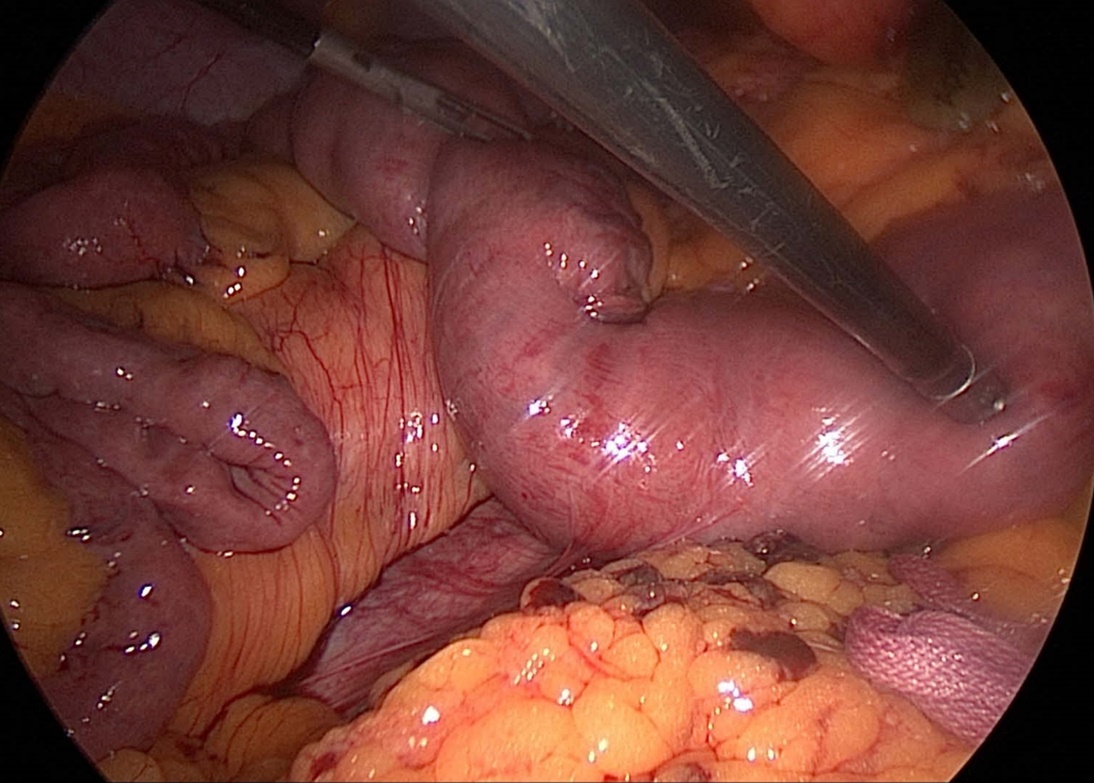
Figure 1: intraoperative view of the ligament of Treitz, placed on the right side
In particular, the ligament of Treitz and jejunum were placed on the right side of the abdomen, the whole ileum was a mirror image respect to the normal and the ascending colon was medialized.
As first step, the sleeve was freed from adhesions. The gastric pouch of 3x5 cm was created with multiple mechanical stapler (EndoGIA® 60mm violet cartridge). The other steps of the operation were carried out specularly in relation to normal anatomy: a biliary limb of 50 cm and an alimentary limb of 150 cm were measured. A latero-lateral mechanical jejuno-jejunal anastomosis was performed and the mesenteric defect closed with non-adsorbable sutures (Figure 2).
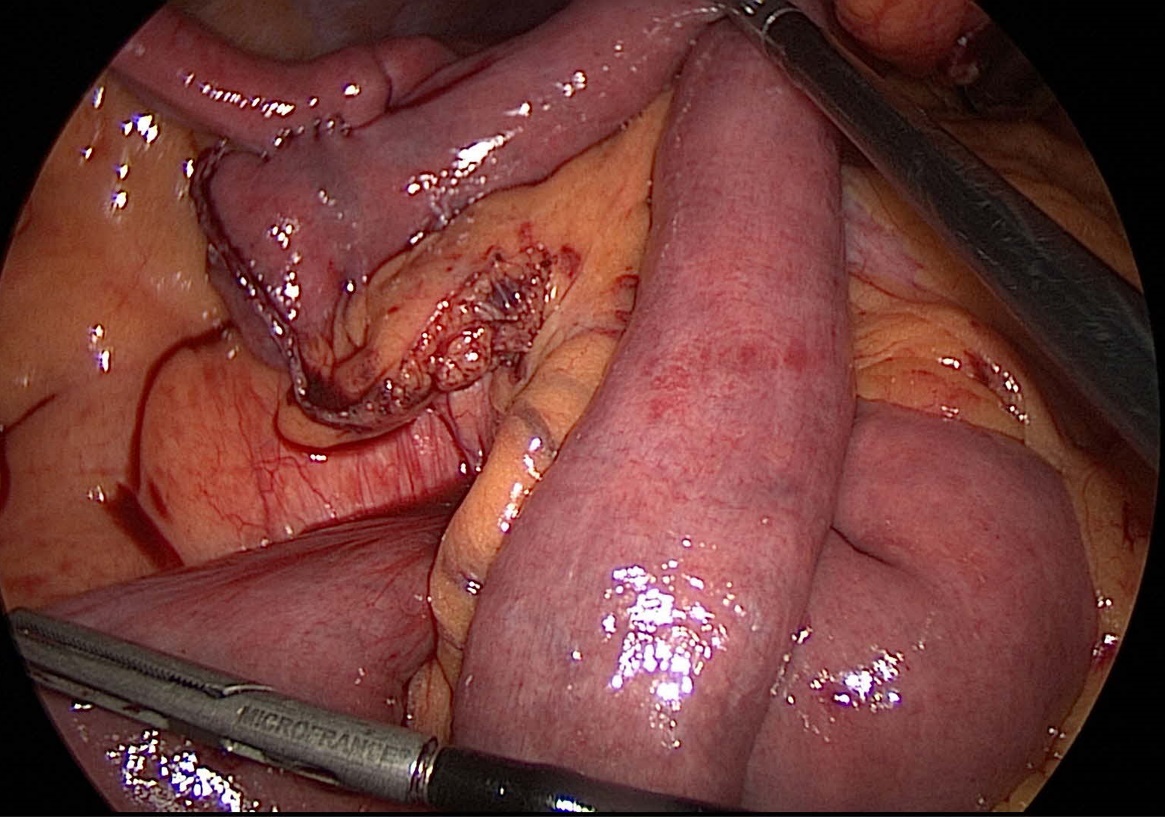
Figure 2: intraoperative view of the mirror position of the jejuno-jejunal anastomosis
An indocyanine-green test was used to assess blood supply of the gastric pouch. Finally, a hand-sewn gastro-jejunal anastomose was created and the mesenteric defects closed with non-adsorbable sutures (Figure 3).
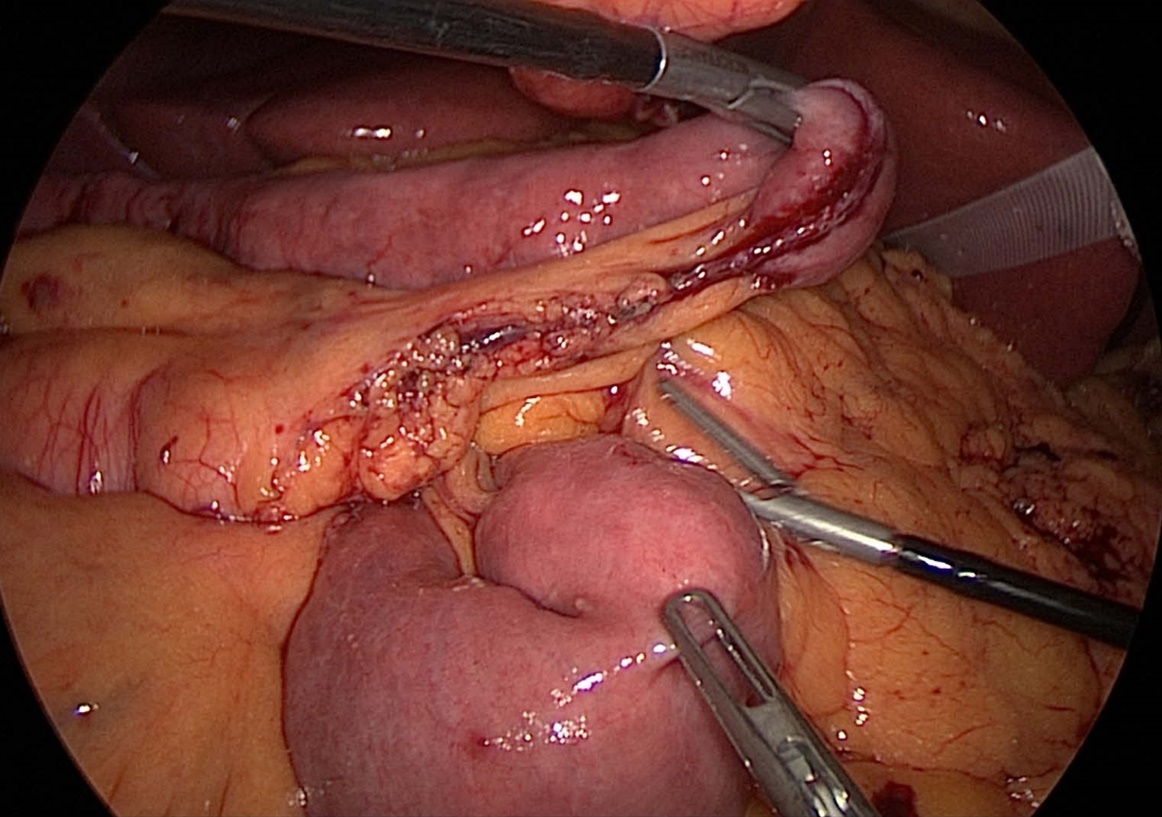
Figure 3: intraoperative image showing the mirror position of the alimentary limb and the Petersen space
The operative time was 151 minutes, with no blood loss. After 6 months the patient lost 25 kg (BMI 26.7 kg/m2) with no complications reported.
Discussion
Intestinal malrotation is a congenital anomaly of the intestine. It is a condition that occurs when the normal rotation of the embryonic gut is arrested during in utero development [5]. Most cases of intestinal malrotation become symptomatic during the neonatal period or within the first years of life, some present in older children or adults as an incidental finding [3]. Because of its rarity, the diagnosis of intestinal malrotation in adult patients is often delayed and could have serious consequences.
Signs of this pathology can be intermittent or acute abdominal pain, intermittent vomiting, failure to thrive/weight loss due to poor oral intake, food intolerance or malabsorption, chronic diarrhea.
The treatment is generally reserved to symptomatic patients, where the majority of experts is in favor to Ladd procedure to prevent volvulus or bowel ischemia [2].
In our case, the malrotation was unrecognized during the sleeve gastrectomy and was found incidentally during the conversional bariatric surgery as we started measuring the small bowel. Intraoperatively, we did not judge the malrotation as a reason to discontinue the operation. The main difficulty in carrying out a conversion into gastric bypass was the need to perform all anastomoses as a mirror image in comparison to the normal. All the automatic surgical movements have to mirror the normal gastric bypass assembly: the direction of measuring the small bowel, the anastomoses, the mesenteric defects closures. In such situations, the knowledge of this congenital anomaly is important to exactly figure out the correct bypass assembly. Intraoperatively, we also discussed if a Ladd procedure was necessary. However, we chose to perform a gastric bypass only as the patients was asymptomatic preoperatively. The anatomy distortion introduced by the gastric bypass might also cause symptoms of the intestinal malrotation in the future. A watchful follow-up is necessary to recognize early alarm symptoms.
Conclusions
Our case is an example of an intestinal malrotation that remained silent till an incidental intra-operative finding in adulthood. Such cases may remain undiagnosed for a long time, even after abdominal operations where the small bowel is not revised. In such situations, when a bariatric surgery is performed, either primary or as conversional surgery, surgeons have to be aware that the whole operation should be assembled as a mirror image of the normal anatomy. Associated procedures (e.g., Ladd procedure) might be not necessary for asymptomatic patients.
Authors' contributions: Conceptualization: FM, ZH. Data curation: ZH, MM, FG. Writing – original draft: ZH, FM. Writing - review and editing: FG, MM.
Funding: none.
Conflicts of interest: none declared.