International Surgery Case Reports
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Ijeoma Agu MD, Asha Bhalwal MD*
University of Texas Health Science Center 6431 Fannin St Houston TX 77030 USA
*Corresponding Author: Asha Bhalwal, University of Texas Health Science Center 6431 Fannin St Houston TX 77030 USA.
Received date: January 13, 2022
Accepted date: January 21, 2022
published date: January 24, 2022
Citation: Agu I, Bhalwal A. (2022) “Laparoscopic Resection of Advanced Gestation Rudimentary Horn Pregnancy: A Case Report”. International Surgery Case Reports, 4(1). DOI: http;//doi.org/11.2022/1.1047.
Copyright: © 2022 Asha Bhalwal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective - To report laparoscopic resection of second trimester horn pregnancy using laparoscopy in a morbidly obese patient. Rudimentary horn pregnancy is a rare condition with incidence quoted as 1 in 76,000 to 150,000 pregnancies. Although uncommon, its presence can lead to significant maternal risks from uterine rupture. Surgical management is the gold standard for care. Laparotomy is traditionally utilized, however laparoscopy is a viable method for management. In this case, we report laparoscopic management of a second trimester rudimentary horn pregnancy in the setting of class III obesity, BMI 48.5. Method - A 14-week gestation rudimentary pregnancy was effectively resected laparoscopically, extracted in a contained fashion. Informed consent was provided and patient authorized authorship and publication of her case as a case report. Results - Pathology findings were consistent with a non-communicating rudimentary horn with pregnancy in situ and evidence of placenta accreta. Conclusion - Second trimester rudimentary horn pregnancy was successfully managed laparoscopically. Accurate preoperative diagnosis and surgical skill are important for detection and management of midtrimester rudimentary horn gestation.
Introduction:
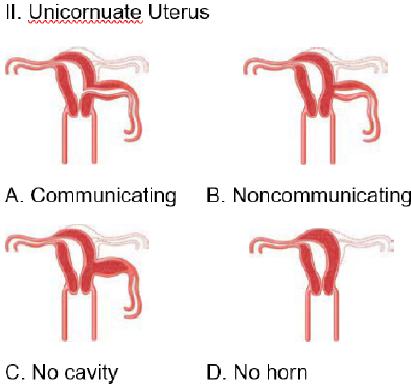
Unicornuate uterus is a type of Mullerian anomaly in which a functional uterus, cervix, fallopian tube, and round ligament are present on one side, however agenesis, or more commonly a rudimentary horn, is present on the contralateral side. The rudimentary horn may communicate or connect with the cavity of the dominant horn (Figure 1).
Figure 1
If the rudimentary endometrial cavity is functional, common symptoms include cyclic unilateral pain or hematometra. Women with unicornuate uterus have an increased incidence of infertility, endometriosis, and dysmenorrhea [5,9,17]. Once diagnosed, standard treatment is surgical removal, traditionally via laparotomy. Laparoscopy is also acceptable. Upon review of the literature, fifteen cases report minimally invasive resection of rudimentary horn pregnancies using laparoscopy, with few advanced gestation pregnancies [5,17]. To date, few reports mention laparoscopic resection in a morbidly obese patient. We report the laparoscopic management of a second trimester rudimentary horn pregnancy in the setting of class III obesity.
Case Presentation:
A 27-year-old G3P0 at 14 weeks and 2 days gestation presented to our medical center as a transfer of care for evaluation and management of suspected abdominal pregnancy. Her obstetric history included an early first trimester spontaneous abortion followed by a pregnancy complicated by periviable rupture of membranes and fetal demise at 20 weeks gestation. She had a pelvic ultrasound showing a 14-week singleton pregnancy with fetal heart tones present and a gestational sac which appeared to be implanted on bowel or on the abdominal side wall. She was sent to our medical center for further evaluation.
On arrival to the hospital, she was hemodynamically stable, denying abdominal pain or vaginal bleeding. On physical exam, her abdomen was soft, nontender to palpation. Medical history was significant for Class III obesity with body mass index of 48.5. Prior surgical history included one suction dilation and curettage for retained products of conception following delivery of 20-week fetal demise. She denied tobacco, alcohol, or illicit drug use.
Abdominal and pelvic MRI were obtained, revealing a unicornuate uterus with a non-communicating rudimentary right uterine horn (Image 1).
Image 1

Rudimentary horn gestation was confirmed with a fundal placenta. Segments of the myometrium within the rudimentary horn were thinned to 3 mm or less.
Given the patient’s gestational age, evidence of myometrial thinning within the rudimentary horn, and morbidity of future uterine rupture, we recommended surgical management. We prepared the patient for diagnostic laparoscopy, laparoscopic resection of rudimentary uterine horn with pregnancy in situ, and the possibility of conversion to laparotomy.
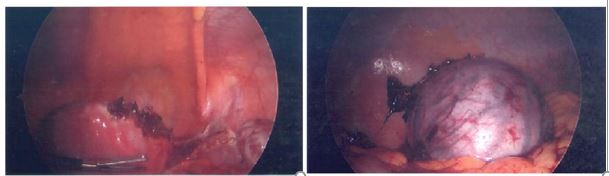
The patient was positioned into dorsal lithotomy with arms tucked to her side. Orogastric tube and foley catheter were placed prior to surgical draping. On exam under anesthesia, her uterus was noted to extend to the umbilicus. Left upper quadrant entry was performed using Palmer’s point. Intra-abdominal survey revealed normal appearing left fallopian tube, normal ovaries bilaterally, and a 7cm right rudimentary horn distended and decidualized in appearance with pregnancy in situ (Figure 2).
Figure 2

The rudimentary horn was attached to the dominant horn about 3 to 4cm at the base. Abdominal survey was otherwise normal.
An infraumbilical 2cm incision was made to accommodate the GelPOINT Advanced Access PlatformTM. Right salpingectomy was performed using LigaSure ImpactTM. Diluted vasopressin was introduced via spinal needle to the base of the rudimentary horn in an effort to minimize blood loss. Right utero-ovarian ligament was coagulated and transected using the LigasureTM. The broad ligament was dissected anteriorly and posteriorly. Bladder flap was created anteriorly. Uterine vessels were skeletonized on the right and ureters identified bilaterally. Bipolar Kleppinger was used to ligate the uterine arteries on the right side, followed by the base of the rudimentary horn. LigasureTM was then used to coagulate and dissect the horn in its entirety from the left horn (Figure 3).
Figure 3
A contained tissue extraction system was placed through the GelPOINTTM port in the umbilicus. The horn with pregnancy in situ was placed into the bag and brought to the abdominal wall (Figure 4).
Figure 4
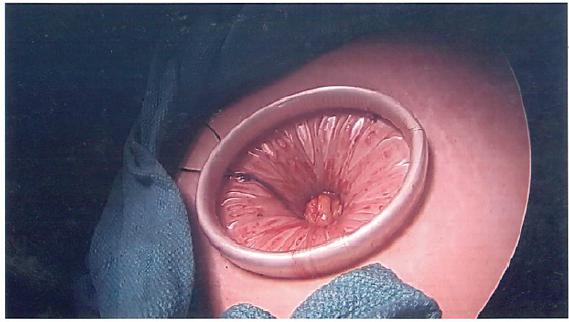
Amniotic fluid was drained using the suction cannula. Specimen was decompressed by removing placental tissue and fetus. The remainder of the specimen with uterine horn was removed from the abdomen, contained in the bag, through the GelPointTM port (Figure 5).
Figure 5

Hemostasis was verified under decreased intra-abdominal pressure. All ports were removed under direct visualization after closing the left upper quadrant 10mm port. The umbilical port was closed using a UR-6 needle in a continuous non-locking manner. Skin was reapproximated using Monocryl in a subcuticular fashion. She was extubated and transported to recovery in stable condition.
She had an uncomplicated postoperative course and was discharged home on postoperative day one. Surgical pathology was consistent with non-communicating rudimentary horn pregnancy with evidence of placenta accreta.
Discussion:
Rudimentary horn pregnancy is very rare, with incidence quoted as 1 in 76,000 to 150,000 pregnancies [10,13,18]. This condition is thought to result from intra-abdominal transit of sperm or fertilized ova from contralateral fallopian tube. Although rare, rudimentary horn pregnancy is associated with serious maternal morbidity resulting from uterine rupture, occurring in 50% of cases, typically prior to 20 weeks gestation [9,13,17]. Reduced uterine distensibility, reduced myometrial contractility, and reduced blood supply attribute to the cause of uterine rupture as the pregnancy progresses [1]. Additionally, rudimentary horn carries a heightened association with placenta accreta. In this case, the pathologists reported the chorionic villi located in intimal proximity to the uterine horn myometrium. Hypothesized etiology suggests a thin, poorly formed decidual layer within rudimentary uterine horns which predisposes the horn to abnormal placentation [1].
Given the morbidity associated with uterine rupture, accurate diagnosis is imperative. Two-dimensional ultrasound may be used as initial imaging modality, but often cannot accurately define the rudimentary horn - as evidenced in this patient who had prior pelvic ultrasounds outside of pregnancy which failed to identify the mullerian anomaly. Further techniques, including MRI or three-dimensional ultrasound, may be required. [5,9,17]. On initial presentation to our medical center, the patient had a two-dimensional ultrasound, however after an equivocal diagnosis, MRI helped to accurately portray the borders of the uterus and outline her anatomy.
Once rudimentary horn pregnancy is diagnosed, surgical management is the gold standard of care. Few laparoscopic cases exist in the literature. In this case, we successfully attempted laparoscopic resection of a rudimentary horn pregnancy. We opted for laparoscopic management in an effort to decrease the patient’s risk of wound complications and prolonged hospital stay from laparotomy, as extracted from data comparing minimally invasive hysterectomy to open hysterectomy in obese patieints [19]. In addition, we utilized hemostatic techniques shown to be beneficial in surgical management of cornual ectopic pregnancies and myomectomies [2]. By injecting Vasopressin, 20U diluted in 100mL of normal saline, along with careful uterine artery ligation and dissection, we were able to maintain minimal blood loss of 100mL.
Identification of ureter location is especially prudent before transecting the uterine arteries, as unicornuate uterus is associated with a 40% risk of renal anomalies, most frequently renal agenesis [7]. Fortunately, this patient did not have renal agenesis, as noted in prior imaging depicting normal kidneys bilaterally outside of pregnancy.
Finally, the patient’s primary concern following treatment surrounded her ability to carry future pregnancies. Patients with uterine anomalies have an increased rate of miscarriage, preterm birth - quoted as 39.7% and 14.5% < 34 weeks [16], and breech presentation, in addition to a risk of hypertensive disorders in pregnancy in the setting of concurrent renal agenesis [7-8,13]. Sawada et al demonstrated successful vaginal delivery in patients who were deemed good candidates for trial of labor, as defined as those who did not require uterine myometrium resection during surgery [16]. Additionally, close intrapartum maternal and fetal monitoring are imperative.
Conclusion:
Rudimentary horn pregnancy is a rare condition which carries significant maternal risks. Surgical management is strongly recommended. Although laparotomy is traditionally utilized,
laparoscopy is a viable method for management. This case reports a second trimester rudimentary pregnancy which was effectively managed using minimally invasive techniques to minimize blood loss, extract specimens in contained fashion, and minimize hospital stay.
Data Availability:
All data supporting the conclusions above can be accessed in the listed references
Contributors:
All authors made a substantive contribution to the information or material submitted for publication.
Funding Statement
This work was supported by Department of Obstetrics, Gynecology, and Reproductive Sciences at the University of Texas Health Sciences Center Houston
Conflict of Interest:
The authors declare that they have no conflict of interest regarding the publication of this case report