International Surgery Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Raghunandan Dixit 1, Asuri Krishna 2*, Vuthaluru Seenu 3, Virinder Kumar Bansal 4
1Junior Resident, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi
2Additional Professor, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi
3Professor, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi.
4Professor, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi
*Corresponding Author: Asuri Krishna, Department of surgical disciplines, All India Institute of Medical Sciences, New Delhi, India.9
Received date: November 16, 2021
Accepted date: November 24, 2021
published date: December 06, 2021
Citation: Dixit R, Krishna A, Seenu V, Virinder K Bansal, (2021) “Covid-19 And Gut Ischemia- An Unusual Presentation.”. International Surgery Case Reports, 3(3); DOI: http;//doi.org/11.2021/1.1041.
Copyright: © 2021 Asuri Krishna. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
The novel COVID-19 disease caused by the SARS-CoV-2 virus which initially manifested as a lower respiratory tract infection, but has now been found to have manifestations involving multiple systems. In several studies, acute COVID-19 infection has been linked with hypercoagulability and higher incidence of arterial and venous thrombosis. We report a case of a 54-year-old man who presented to the emergency with severe abdominal pain and vomiting. A Contrast-enhanced computed tomography (CECT) scan of the abdomen revealed superior mesenteric artery occlusion with gangrenous small bowel. A positive COVID-19 test was obtained. Emergency surgery with resection of gangrenous ileal segment and creation of a double-barrel stoma was done with ongoing COVID-19 treatment. A CT angiography after COVID negative status revealed a significant resolution of SMA thrombus and good distal flow. The patient was discharged on oral anticoagulation. Restoration of bowel continuity was done in view of frequent emergency admissions with dehydration
Background
Acute mesenteric ischemia (AMI) is a rare, life-threatening abdominal emergency, accounting for 0.09-0.2% of all emergency surgical admissions[1]. Although it is a rare cause of abdominal pain, prompt diagnosis and treatment is required because, if left untreated, mortality in the range of 50% has been reported[1]. COVID-19, the novel coronavirus disease caused by SARS CoV-2, originated in Wuhan, China, in 2019 initially as a pulmonary infection, while later reports indicated a multi-system involvement. 15% of COVID-19 patients experience gastrointestinal symptoms ranging from anorexia, nausea, vomiting, diarrhea, and abdominal pain[2,3]. A higher level of C-reactive protein, ferritin, interleukin-6, lactate dehydrogenase, fibrinogen, and D-dimer in COVID-19 infected patients suggests a systemic pro-inflammatory state[4]. Angiotensin-converting enzyme-2 (ACE-2) receptors of COVID-19 are abundantly present on the alveolar epithelium and enterocytes of the small intestine[5]. The virus binds to these receptors, causes local inflammation that leads to thrombi forming in small and large vessels, leading to diverse clinical manifestations. In the intensive care unit (ICU), the incidence of venous and arterial thromboembolism is 28% (95% CI, 22-34%), and 3% (95% CI, 2-5%), respectively. The incidence of venous thromboembolism is reported to be 10% (95% CI, 6-14%) in non-ICU settings[6]. Multiple case reports of acute ischemia of limbs in COVID-19 infected patients have been reported[7,8]. A few cases of acute intestinal ischemia in patients with COVID infection have been published, but they were seen in patients with severe COVID infection and with risk factors for acute thrombotic and embolic events[9,10]. We present a case of superior mesenteric artery thrombosis with moderately severe COVID-19 infection.
Case Presentation
A 54-year-old man with no previous surgical and medical history presented to the emergency room with acute onset, severe, periumbilical, non-colicky, non-radiating pain for 3 days which aggravated after meals, with non-passage of stools and flatus for 2 days but no abdominal distention. He had 2 episodes of vomiting with altered blood as content. As per the institutional protocol, all emergency patients were considered COVID-19 suspects and were admitted to a COVID-19 suspect area pending the COVID-19 report. Therefore, the patient was evaluated in a COVID suspect area. He was afebrile, dehydrated, tachycardic with a regular rhythm, hypotensive with a 92% oxygen saturation (SpO2). There was diffuse abdominal tenderness and guarding, but no distention, rebound tenderness or rigidity. Bowel sounds were absent. Initial diagnosis of acute abdomen was made with differential diagnosis of suspected hollow viscus perforation, bowel ischemia and acute pancreatitis. Resuscitation was started with oxygen supplementation and intravenous crystalloids.
Investigations
Blood tests revealed neutrophilic leukocytosis of 17.6x109/L, hematocrit of 46%, serum creatinine of 1.4mg/dl with normal serum electrolytes. Serum amylase and lipase were normal. The arterial blood gas analysis revealed metabolic acidosis with raised lactate levels of 8.0 mmol/L (Normal range- 0.5-1 mmol/L). An electrocardiogram revealed sinus tachycardia without arrhythmia. A chest X-ray was normal and a plain erect abdominal X-ray did not reveal air-fluid levels or pneumoperitoneum. In view of the pain out of proportion to the examination findings, a CECT scan of the abdomen and pelvis was performed with screening CT chest for COVID. The CECT showed a hypodense filling defect occupying 90% of the lumen of the superior mesenteric artery (SMA) at its origin, with reduced distal flow, and a segment of ileum showing loss of mural enhancement with pneumatosis, indicative of bowel gangrene (Figure 1 and 2), without pneumoperitoneum.
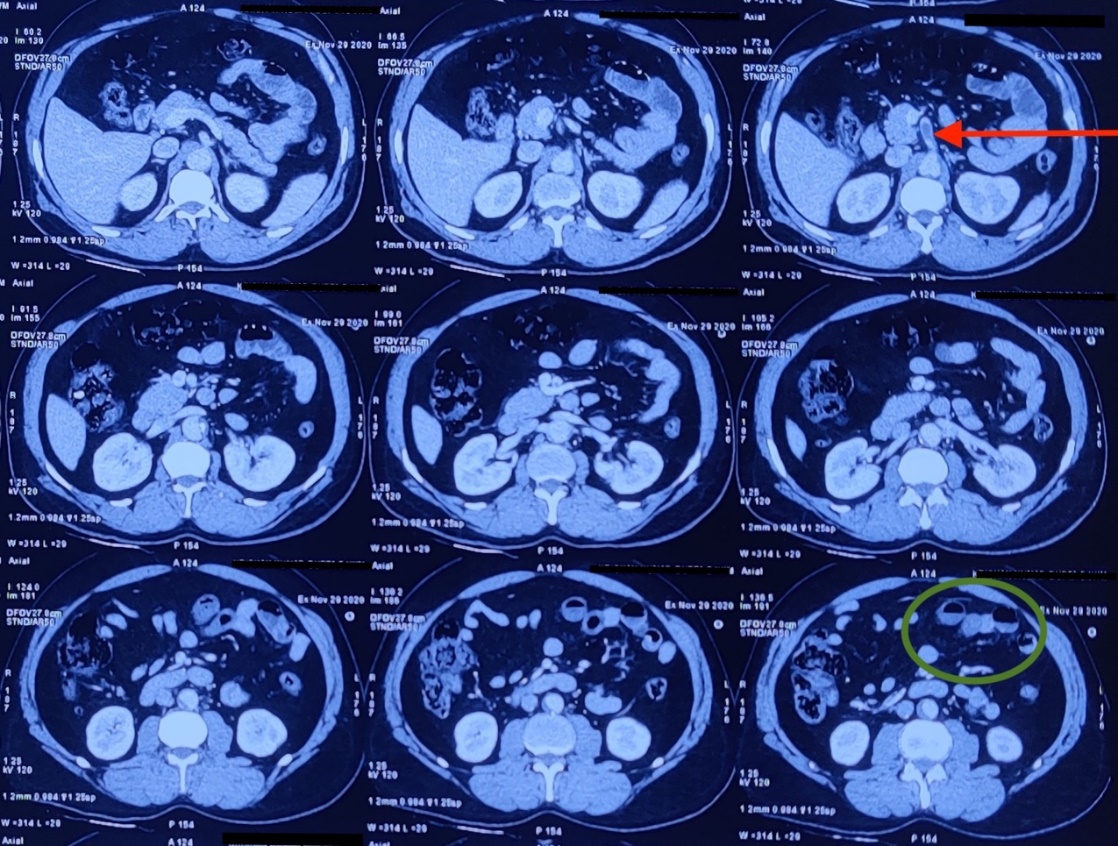
Figure 1. Abdominal CT scan with thrombus in superior mesenteric artery 1 cm distal to origin occupying >90% of lumen, with few small bowel loops showing loss of mural enhancement and pneumatosis suggestive of small bowel gangrene.
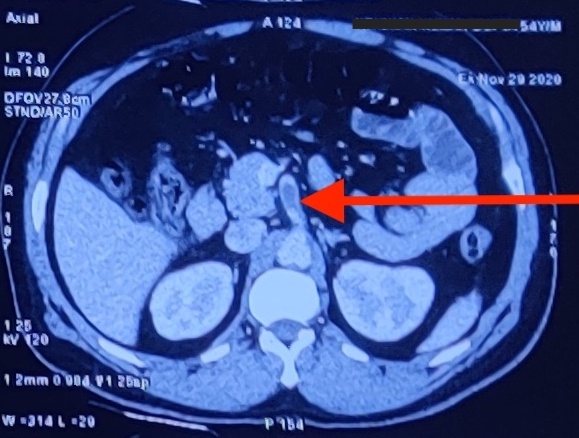
Figure 2. 25cm of resected small bowel with thinned out wall with gangrenous changes ad mesenteric fat stranding seen, which on cut opening correspond to brownish black papery thin mucosa however no perforation was seen.
CT scan of the chest showed bilateral minimal pleural effusion with bilateral lower lobe ground-glass opacities suspicious for COVID-19 infection with coronavirus disease 2019 Reporting and Data System score 4 (CO-RADS 4), which implies a high level of suspicion for COVID-19. CO-RADS is the assessment scheme for pulmonary involvement in COVID-19 with good performance for predicting COVID-19[11]. Meanwhile, a positive COVID-19 Cartridge Based Nucleic Acid Amplification Test (CBNAAT) report was obtained.
Differential Diagnosis
The initial diagnosis at emergency department was acute abdomen with suspicion of perforation of the hollow viscus, bowel gangrene and acute pancreatitis. In the erect abdominal X-ray, there was no free air and the possibility of hollow viscus perforation was ruled out with CECT scan. As amylase and lipase were normal, acute pancreatitis was unlikely.
CECT confirmed the diagnosis of acute mesenteric ischemia with bowel gangrene, so the patient was planned for emergency surgery with ongoing evaluation to determine the exact cause of SMA thrombosis.
Treatment
The patient was transferred to the COVID facility for emergency surgery. After resuscitation with intravenous crystalloids, supplemental oxygen, and administration of intravenous antibiotics, emergency laparotomy was performed. There was a 25cm long ischemic segment of the ileum with multiple dusky infarcts about 120 cm proximal to the ileocecal junction. SMA pulsations were present but feeble. Hot mops were applied to the affected segment of the bowel with 100% oxygen for 20 minutes but no change in perfusion was observed. The gangrenous segment was resected (Figure 3) and healthy, bleeding ends were brought out as double barrel ileostomy. Hematological workup for hypercoagulable states including Protein C and S, Factor VIII, Factor V Leiden, Paroxysmal nocturnal hematuria (PNH), anti-phospholipid syndrome (APLA) were within normal limits. Serum ferritin, fibrinogen, and D-dimer (for COVID prognostication) were significantly elevated.

Figure 3. 25cm of resected small bowel with thinned out wall with gangrenous changes ad mesenteric fat stranding seen, which on cut opening correspond to brownish black papery thin mucosa however no perforation was seen.
2-D echocardiography was normal and did not reveal any thrombi in the heart. Treatment of moderate severity COVID infection was started, including injection Enoxaparin sodium 40mg subcutaneous on a postoperative day (POD) 1. The patient had an uneventful postoperative recovery. COVID-19 RT-PCR (Reverse Transcriptase-Polymerase Chain Reaction) was negative on POD10. A CT angiography performed on POD 15 revealed a reduction of thrombus size in SMA with a 30% occlusion, good distal flow, few aortic plaques, and the rest of the study was normal (Figure 4).
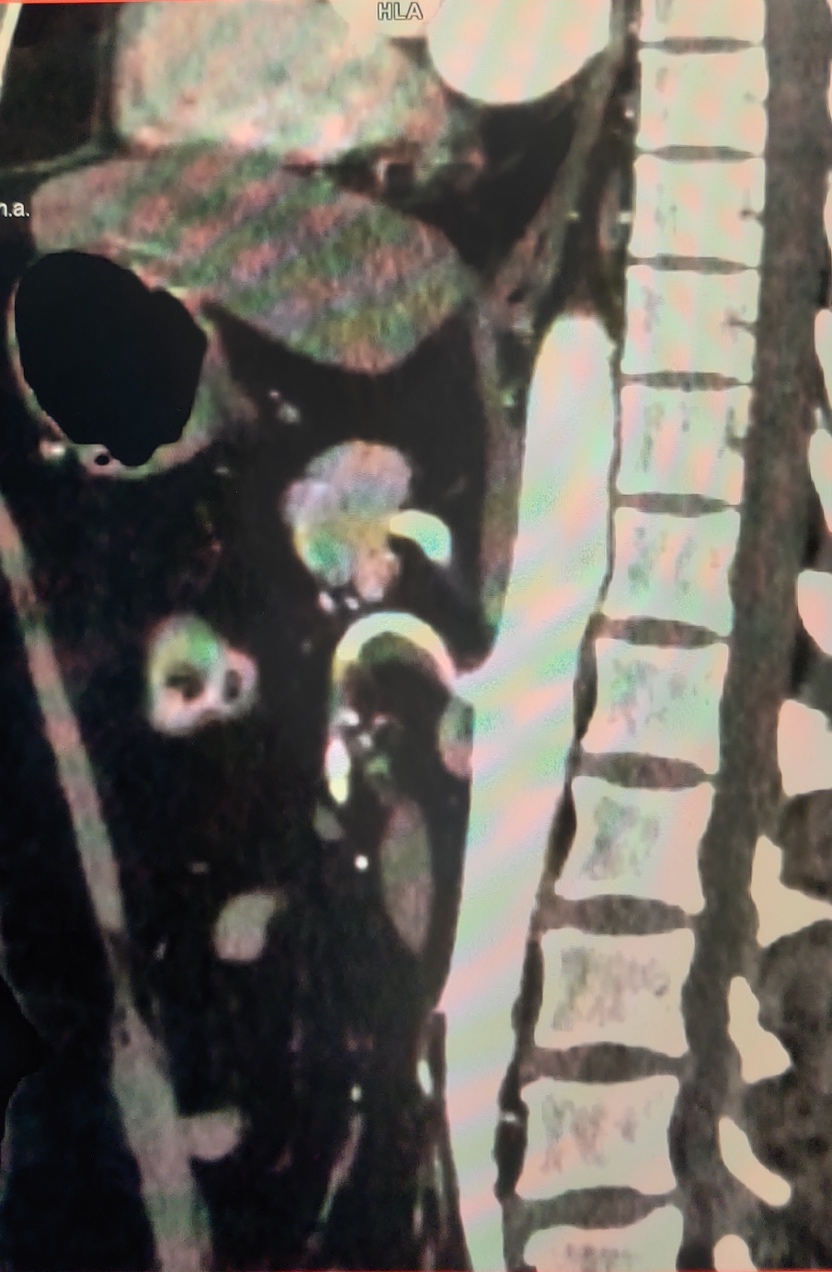
Figure 4. Follow up CT angiography showing peripheral superior mesenteric artery thrombus with 30% occlusion but a good distal flow seen.
Given the response to ongoing anticoagulation therapy, oral anticoagulation with Warfarin 2mg once daily was started and the patient was discharged on POD 15 with an International Normalized Ratio (INR) of 2.8.
Outcome And Follow-Up
The patient visited the emergency department twice on POD 24 and POD 42 with decreased oral intake and dehydration with high output from ileostomy which was managed conservatively with intravenous crystalloids. After 6 weeks, restoration of bowel continuity was done, following which the patient is doing well.
Discussion
Acute mesenteric ischemia is a rare but life-threatening abdominal emergency that requires prompt diagnosis and treatment. COVID-19 causes gastrointestinal manifestations in 15% of infected patients. Symptoms include anorexia, nausea/vomiting, diarrhea, and abdominal pain. In a review of 13 cases of mesenteric ischemia in COVID infected patients by Singh B et al, no prior comorbidities were reported in 6 patients whereas 7 patients had comorbidities like HTN, essential thrombocytosis, obstructive sleep apnea, diabetes, etc. Mortality was seen in 4 of 11 case reports, which is consistent with a reported mortality of AMI but 50% mortality was seen in patients who did not have any comorbidity[12], thus, COVID-19 induced procoagulant state seems to be an independent factor for thrombosis.
AMI can occur as a presenting feature[10,13] or a delayed complication[9,14] of COVID-19 infection. The nature of COVID-19 as a critical illness entails a hypercoagulable state due to immobilization, nutritional deficiencies, mechanical ventilation, prolonged venous access devices, etc. ACE-2 receptors which are binding sites for the SARS COVID-19 virus are abundantly present on enterocytes of the small intestine and vascular endothelium which sparks a cycle of inflammation and thrombosis in small bowel vasculature[5].
In absence of risk factors of acute mesenteric ischemia, the local hypercoagulable state induced by COVID-19 infection may be a possible cause, and a suspicion of mesenteric ischemia should be kept in mind in patients with acute abdomen and COVID-19 infection. As the virus targets vascular endothelium, causing widespread endothelial dysfunction[4] along with inflammation, hypoxia, and immobilization, both venous and arterial thromboembolic events may be predisposed[13,15-17]. The present case is unique as even on extensive workup, no hypercoagulable etiology other than COVID-19 infection could be identified. The majority of the reported cases have indirectly attributed the AMI to COVID-19 in absence of co-morbidities.
Due to the delay in detection of mesenteric ischemia, especially in Indian settings, the addition of CECT abdomen in patients undergoing CT chest should be considered in the COVID era for patients with clinical symptoms or signs of acute abdominal pain. Early diagnosis and prompt radiological or surgical intervention are pivotal for improved outcomes in acute mesenteric ischemia. The delay in diagnosis and intervention of COVID positive patients due to logistic issues in isolation and transport does pose a challenge and an emergency physician should be aware of these obstacles, as time is crucial for a better outcome.
Learning Points
Patient’s Perspective
Following severe abdominal pain and vomiting, I went to the hospital. I was terrified seeing the ongoing COVID-19 pandemic. I had no fever and respiratory symptoms. My COVID-19 report was positive. I was told about a block in my blood vessel and emergency surgery will be done. I am currently doing well, happy with the management. I want to thank all the doctors and hospital staff.