International Surgery Case Reports
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Henrique Moura Braga
Holy House of Mercy of Belo Horizonte, Basil.
*Corresponding author: Henrique Moura Braga, Holy House of Mercy of Belo Horizonte, Basil.
Received date: November 13, 2021
Accepted date: November 18, 2021
published date: November 24, 2021
Citation: Henrique M Braga, (2021) “Percutaneous Biopsy of Lesion in The Cavernous Sinus Region Through the Foramen Ovale – Case Report.”. International Surgery Case Reports, 3(2); DOI: http;//doi.org/11.2021/1.1040.
Copyright: © 2021 Henrique Moura Braga. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
A 51-year-old woman presented with cavernous sinus syndrome due to a petroclival lesion which was suspected as malignant lesions. The diagnosis of this lesion was made through immunohistochemistry from a percutaneous trans-foramen ovale biopsy. The purpose of this report is to expose the role of biopsy through the foramen ovale.
Case Report
M.C.F, 51 years, female, without comorbidities, clinical illness has begun in January of 2018 with headaches in the left frontoparietal region, associated to hacking dizziness episodes. In February of 2018 has suddenly involved strabismus convergent in the left eye and left peripheral facial paralysis. On examination, in May 2018, the patient has presented facial paralysis on the left side, complete eyelid ptosis and left ophthalmoplegia with preserved visual acuity in both eyes. An MRI of the brain was made study and showed an expansive lesion with a left petroclival epicenter, infiltrating Meckel cavum and cavernous sinus. At the time of brain tumor diagnosis, the diagnosis hypothesis raised was of a meningioma in the left petroclival region. Thus, in May 2018, a biopsy guided by radioscopy of a petroclival tumor by the left foramen ovale was taken without complications. The anatomopathological study showed low differentiated neoplasia suggestive of metastatic carcinoma and immunohistochemical diagnosed neuroendocrine carcinoma. At hospitalization the patient was submitted to a oncological screening that has showed lung injuries. Due to the progress of the clinical situation the pacient came to death in two weeks without accomplishing the adjuvant treatment.
Discussion
Percutaneous biopsy through the foramen ovale approach is the last minimally invasive diagnostic option for the 15% of patients in whom etiology remains unclear despite extensive neuroradiological imaging, clinical assessment and laboratory evaluation. [1] It is particularly necessary in patients with rapid progression of symptoms, which is often associated with inflammatory, infectious or malignant lesions. [2] This method can be indicated for and performed on lesions of the central base of the skull located in the Meckel cave, cavernous sinus or upper part of the petroclival region, particularly when there is insufficient information to define an etiologic diagnosis and proceed with a treatment course using imaging-guide methods.[3]
In the case report, we had a swift evolution in the patient’s symptoms, with an inconclusive image that showed a lesion in the cavernous sinus with a low possibility of resection. Biopsy through foramen ovale was important for defining the diagnosis with less morbidity for the patient. The effectiveness and safety of biopsy of the foramen ovale is well reported in the literature, and in a recent meta-analysis, Dellaretti M. et al, brought together 14 studies with 75 cases in the literature. Diagnosis was obtained in 65 of the 75 cases (86,6%). In all series, only three patients had permanent deficits. No individual studies reported mortality [3].
Another relevant point of the case report was the immunochemical diagnosis. The result of neuroendocrine carcinoma of the central nervous system was in a certain way surprising, considering that besides the fast progress of the clinical situation the images dind’t suggest a metastatic lesion.
After the result of neuroendrocrine carcinoma it was verified a primary lung lesion such as showed by literature that the primary source of these lesions are usually from other sites, usually at respiratory and gastrointestinal tract [4].
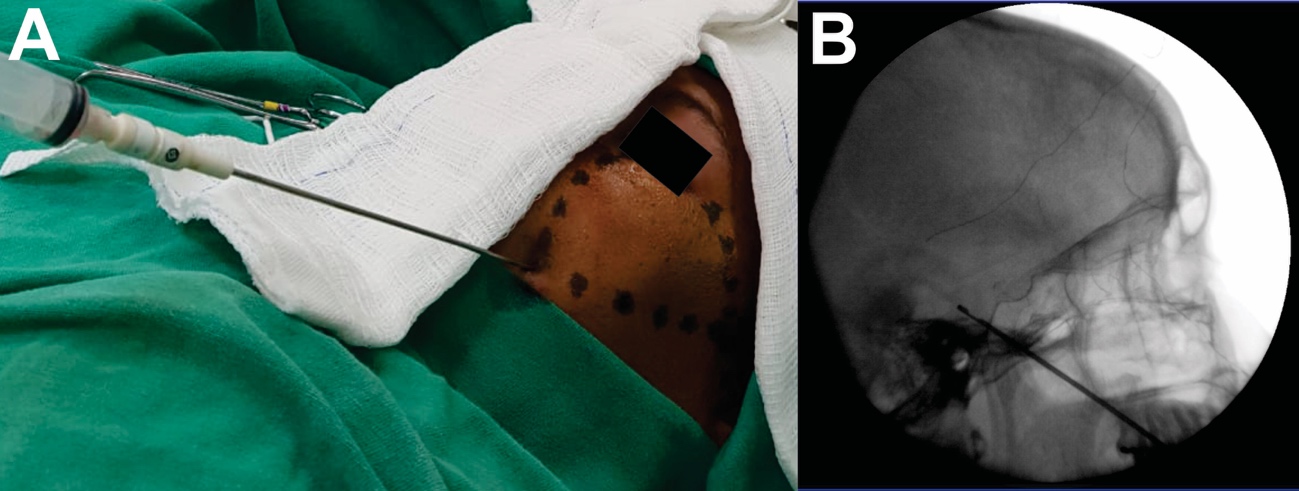
Figure 1: A. Intraoperative. B. Intraoperative fluoroscopy
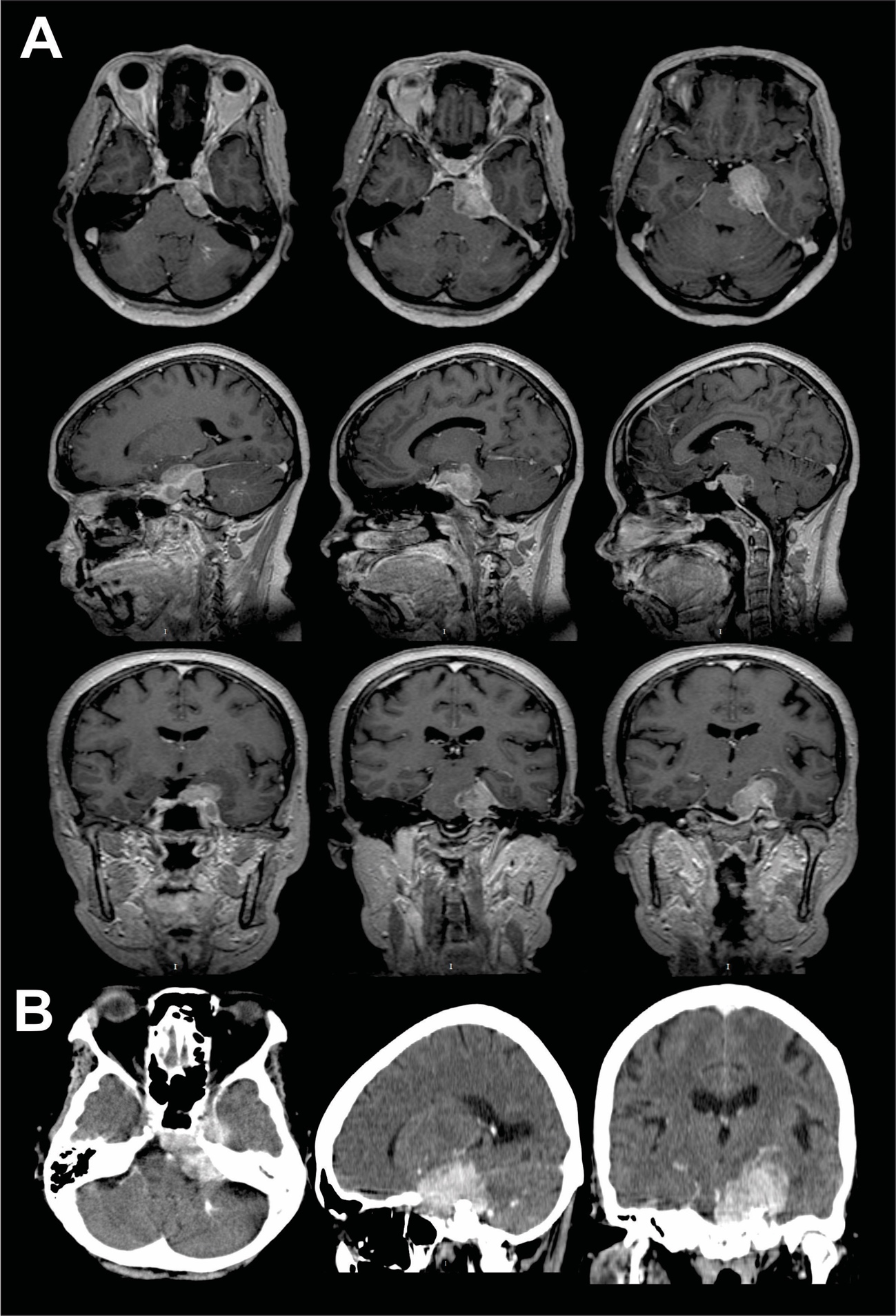
Figure 2: A. Preoperative T1 contrasting MRI B. Preoperative CT contrasting
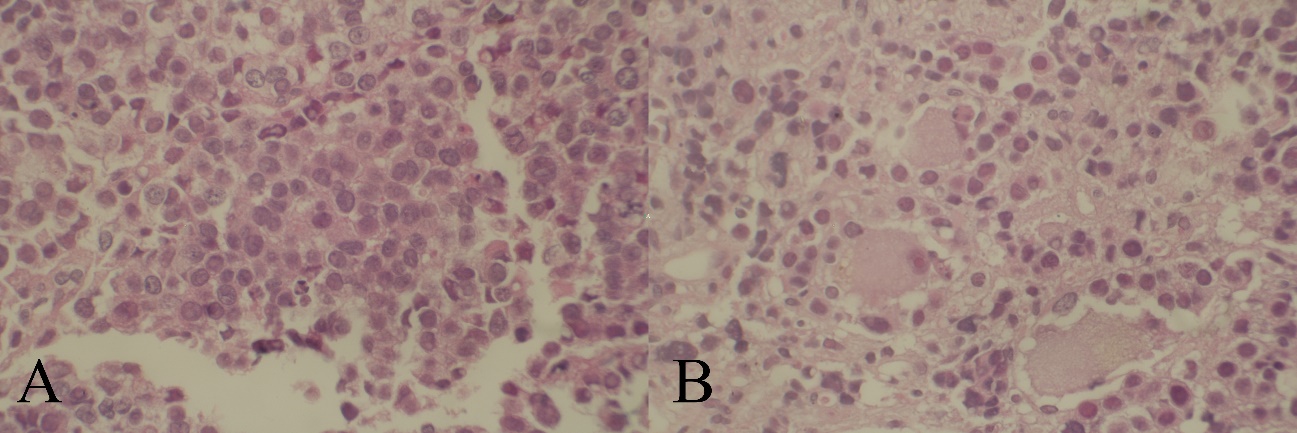
Figure 3: Histopathology of metastatic carcinoma. A. Cells with large and hyperchromatic nucleus B. Big cells big eosinophilic cytoplasm forming solid blocks.
Conclusion
The percutaneous biopsy of lesions in the cavernous sinus region is efficient for the diagnosis with low morbidity described in the literature. This procedure can be accomplished in the Meckel cave, cavernous sinus or upper part of the petroclival region, especially in cases where neuroimaging is inconclusive or insufficient on the histological pattern of the lesion.