International Surgery Case Reports
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Morgan E. Pegg, Michael Sistare *, Nir Hus
General Surgery, Larkin Community Hospital · Miami, USA
*Corresponding author: Michael Sistare, General Surgery, Larkin Community Hospital · Miami, USA
Received date: July 28, 2021
Accepted date: August 02, 2021
published date: August 06, 2021
Citation: Morgan E. Pegg, Sistare M, Hus N, (2021) “Preoperative Acute Ventricular Thrombosis During Induction of Anesthesia.”. International Surgery Case Reports, 3(1); DOI: http;//doi.org/03.2021/1.1035.
Copyright: © 2021 Michael Sistare. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A 68-year-old male restrained front-seat passenger presented to the emergency department following a motor vehicle collision. He had displaced fractures of the left distal fibular and tibial shafts, a non-displaced left medial malleolus fracture, multiple closed right rib fractures causing flail chest, a right clavicular fracture, mesenteric contusions, hepatic injury, splenic injury, and traumatic hemopneumothorax with subcutaneous emphysema. The patient underwent multiple procedures to correct his injuries, including placement of a right chest tube, an exploratory laparotomy to address hepatic lacerations and control bleeding with splenectomy, surgical exploration of a transverse colonic mesenteric hematoma, left tibial irrigation and debridement with external fixation, and a second-look laparotomy including abdominal washout and removal of laparotomy pads. Unfortunately, the patient ultimately expired as a result of intraoperative acute coronary syndrome causing standstill with intracavity coagulation and in situ thrombus formation during induction of anesthesia during the planned rib plating procedure.
Introduction
It is rare to rapidly develop acute aortic thrombosis during surgery. Aortic thrombosis usually develops in the setting of pre-existing aortic disease complicated by underlying atherosclerosis [6]. Even though Virchow’s triad (hypercoagulability, blood flow stasis, and vessel wall injury) are the major factors that promotes thrombus formation, the exact pathogenesis of aortic thrombosis is unknown [7]. Malignancy or hematologic diseases have been identified as one of the underlying causes of aortic thrombosis when it does occur [7]. Incidental aortic thrombosis is even rarer and is almost always detected after patient death.
Case Presentation
A 68-year-old male was a restrained passenger in the front passenger seat in a motor vehicle collision in which his side of the car was directly hit by another car at moderate speed (T-bone collision). Primary survey by Emergency Medical Services (EMS) in the field revealed decreased mentation and flail chest. EMS intubated the patient, administered ketamine and rocuronium, and performed needle decompression of the right chest. A cervical collar was placed on the neck for stabilization during transport and the patient was immediately transported to Delray Medical Center in Florida, where he was evaluated in the trauma emergency department. Upon arrival to the emergency department, the patient remained unresponsive and intubated. A chest tube was placed on arrival to the trauma bay to manage decreased breath sounds and subcutaneous crepitus of the right chest. The patient was initially hypotensive (systolic blood pressures ranging from 70-110 mmHg) and received two units of un-crossmatched blood in addition to fluid resuscitation. Subsequently, a right femoral multi-lumen access catheter (MAC), nasogastric (NG) suctioning tube, and Foley catheter were placed without complications. Arterial blood gas analysis was performed, and ventilation settings were adjusted appropriately. Further head-to-toe inspection revealed pale skin, an abrasion on the left forehead, a right eyebrow laceration, and an open deformity of the left ankle. Focused assessment with sonography in trauma (FAST) examination was performed twice, and were negative. Following stabilization in the emergency department, the patient was transported to the computerized tomography (CT) suite where a scan of the thorax and abdomen revealed abdominal free fluid concerning for a liver injury, residual pneumothorax in the right chest, bilateral rib fractures (more prevalent on the right side), and extensive mediastinal and extra-thoracic soft tissue emphysema. The patient was then taken to the operating room for an exploratory laparotomy, during which he underwent splenectomy, perihepatic packing with laparotomy pads, and control of bleeding from a transverse colonic mesenteric hematoma. An Abthera wound VAC was placed to allow for a second-look laparotomy two days later. Three days after he initially presented to the emergency department, the patient underwent surgical chest wall reconstruction and plating of multiple rib fractures on the right side. Shortly after placement of the double-lumen tube (DLT) by anesthesia the patient went into sudden cardiac arrest. The anesthesiologist called for vasopressors, troponins, and a 12-lead electrocardiogram (EKG). The anesthesiologist identified new-onset EKG changes in the inferior and anterior leads, including ST depression and inverted T waves. Advanced cardiovascular life support (ACLS) measures were initiated, but the patient continued to have recurrent episodes of unstable/pulseless ventricular tachycardia. The patient was defibrillated multiple times, but unable to return to spontaneous circulation. The patient ultimately expired, and an intraoperative transesophageal echocardiogram (TEE) revealed a pulmonary embolism and no cardiac activity. The anesthesiologist who performed the TEE reported his findings without images.
Discussion
Motor vehicle accidents are a leading cause of death worldwide. In the United States alone, motor vehicle accidents injure 2.9 million people and end the lives of 30,000-40,000 people [5].
Although aortic trauma most commonly occurs from penetrating trauma as a result of knife or gunshot wounds, blunt aortic trauma rarely occurs [1]. The overall incidence of blunt aortic injury following a motor vehicle is 0.00068%, with the risk increasing in elderly patients [2]. Sumpio et al. found that 72% of patients of patients with aortic thrombosis following blunt trauma were males presenting with seat belt and/or steering wheel injuries following motor vehicle accidents [1]. Blunt abdominal trauma following a motor vehicle collision may result in thrombosis of the aorta depending on many factors, such as the force and nature of the accident and the body type of the patient. Acute abdominal thrombosis following blunt trauma more commonly occurs in patients with underlying coronary atherosclerotic disease [1]. Another rare etiology of acute aortic thrombosis is improper application of the Heimlich maneuver [3]. Abdominal thrusts may dislodge an already formed thrombus or promote thrombosis. In both cases, thromboembolism of the aorta resulted in a fatal reperfusion injury [3].
Until this case, there have been no recorded incidences of acute development of ventricular thrombosis during pre-operative induction of anesthesia. Crawford et al. reported two cases of embolic aortic occlusion due to left ventricular thrombus formation, however development of these thrombi occurred outside of the operating room [8]. In one of the two cases, the patient had a history of atrial fibrillation not managed with anticoagulation medications [8]. Over 40% patients with an acute aortic occlusion had an underlying malignancy, regardless of the location of the occlusion or the origin of the embolus8. Historically, acute aortic occlusions occurred more frequently due to emboli than thrombi. In recent years, the etiology has evolved to be primarily thrombotic in nature. Crawford et al. speculates this may be due to improved prevention of cardioembolic events, thus increasing the number of patients with advanced aortic atherosclerosis [8]. Because acute aortic thrombosis normally has such high morbidity (74%) and mortality (35%) rates, when it spontaneously occurs during induction of anesthesia, it can prove rapidly fatal as in our patient [9]. This report serves as an example for providers so that this rare occurrence can be potentially avoided in the future. Further research into this phenomenon would prove beneficial.
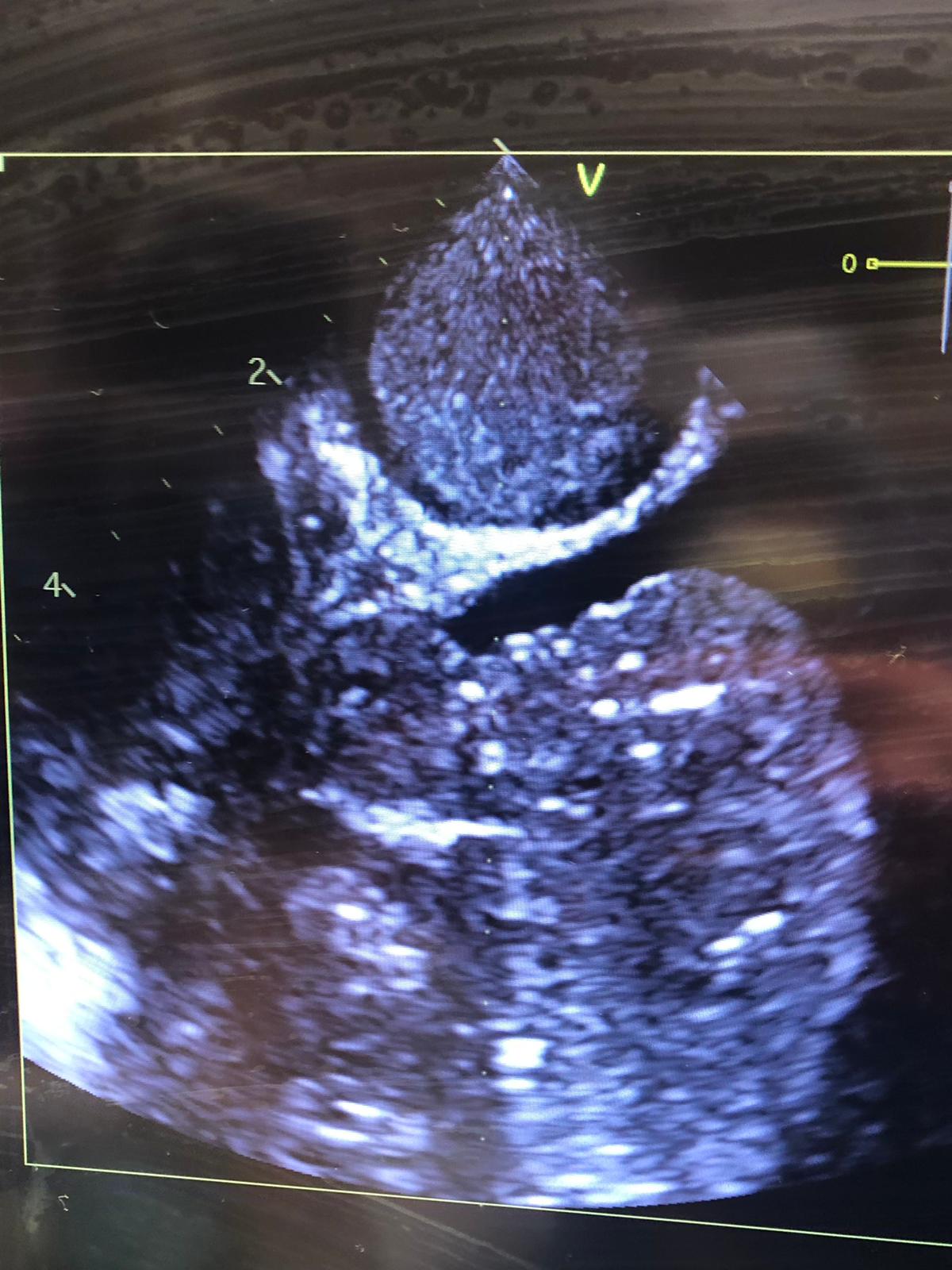
Figure 1: Intraoperative transesophageal ultrasound showing thrombus in the left ventricle
Conclusion
Acute-onset aortic thrombosis is a rare complication of blunt abdominal injury due to motor vehicle accidents, and pre-operative acute aortic thrombosis during induction of anesthesia has not yet been encountered. The pathogenesis is still unclear, and further research is needed to determine the exact etiology of such a condition