Suresh Kishanrao,
Family Physician & Public Health Consultant Bengaluru & Visiting Professor of Practice-MPH, Schools of Environmental Science, Public Health and Sanitation Management, Karnataka State Rural Development and Panchayat Raj University (KSRDPRU), GADAG, Karnataka India.
*Corresponding author: Suresh Kishanrao, Family Physician & Public Health Consultant Bengaluru & Visiting Professor of Practice-MPH, Schools of Environmental Science, Public Health and Sanitation Management, Karnataka State Rural Development and Panchayat Raj University (KSRDPRU), GADAG, Karnataka India.
Received date: February 27, 2023
Accepted date: April 21, 2023
published date: Juny 19, 2023
Citation: Suresh Kishanrao. (2023) “Epidemiology & Management of Cough in smaller settings – an Indian Case study”. International Journal of Epidemiology and Public Health Research, 3(1). DOI: http;//doi.org/01.2023/1.1042.
Copyright: © 2023 Suresh Kishanrao. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Nearly every person experiences at least one episode of cough every year in their lifetime. Common cold, runny nose and sometimes fever along with cough is common during winter months, most, people seek care outside home only after trying known home remedies, especially cough disturbs their sleep due to postnasal drip.
Available data suggest that an average Indian adult has 3 episodes of cough per year, while an average child has 7-10 such episodes every year. The COVID-19 pandemic has increased the magnitude of cough across the world since early 2020. The most annoying part about a cough is “phlegm or mucus.” Mucus forms a protective lining in certain parts of our body, protects our body from foreign invaders by trapping the irritants and expel them in a cough. Excessive Phlegm or mucus is produced as a response to an irritant from the environment like allergies, smoke, smoking, dust, and infections. Excess phlegm or difficulty to expel phlegm can be tackled as per its cause or origin.
No doctor or a health care worker, in his/her clinical practice has a day without seeing a patient with cough. The diagnostic tests are either not available, or unaffordable, if available and used take a long time for definitive diagnosis. Another problem is of self-medication with innumerable number of over-the-counter cough syrups. Most practitioners know about the types of coughs, their symptomatic treatment and over the counter cough syrups and mucolytics, but very few know, the Ideal rationale of managing cough. A simple symptoms based logarithmic approach helps in differentiating various conditions causing cough and managing them empirically. This article highlights such an approach for small settings.
Materials & Methodology: This review is based on the review of literature on the ideal rationale of managing cough, own learning from personal practice and practices observed among colleagues, in public sector teaching institutes and private sector hospitals. The article addresses the general practitioner’s dilemma of diagnosis and management by simple symptoms based logarithmic approach and managing empirically.
Introduction:
Cough is one of the commonest complaints a general practitioner or field level health workers comes across, and frequently presents as a troublesome symptom to tackle to clinicians working in both primary and secondary care. The diagnostic tests are neither available, or affordable, if available and used take a long time for definitive diagnosis. Another problem is of self-medication with innumerable number of over-the-counter cough syrups. Therefore, a simple symptoms based logarithmic approach helps in differentiating various conditions and managing empirically. What an average health practitioner knows about cough is the types, how to treat symptomatically most of the cases with cough syrups and mucolytics. The Ideal rationale of managing cough is not well understood {1].
Cough is a forced expulsive manoeuvre, usually against a closed glottis and which is associated with a characteristic sound.” Academicians classify cough into 2 categories: i) Acute cough, defined as one lasting less than 3 weeks ii) Chronic cough, defined as one lasting more than 8 weeks [1]. Acute cough is usually caused by a viral upper respiratory tract infection (URTI), pneumonia or aspiration of a foreign body. The duration of a single episode of URTI associated cough varies but is rarely more than 2 weeks. Incidence of Symptomatic URTI occur at rates of 2–5 per adult person per year, and school aged children suffering 7–10 episodes per year.
Chronic cough has a global prevalence of 5–10% in the general adult population (≥18 years). The National Health Portal of India-2019, reported, 41,996,260 cases and 3,740 deaths from respiratory infections across India in 2018. India contributes to 18% of the global population, with severe acute respiratory infection (SARI) as one of the prominent causes of mortality in children > 5 years of age. A cut off 2 months for chronic cough has been agreed in American, European, and Indian guidelines [2].
Shocking reports of deaths of children after using cough syrups in 2022, more than 300 children - mainly aged under 5 - in Gambia, Indonesia and Uzbekistan died of acute kidney injury, have opened a pandora’s box on management of both acute and chronic cough in smaller settings with the paucity of diagnostic tools. The reported deaths were associated with contaminated medicines, the WHO had said on 30 January 2023 [3]. It also fears that The Philippines, Timor Leste, Senegal, and Cambodia may potentially be impacted because they may have the medicines on sale. The World Health Organization's director reported that ingredients in four cold and cough syrups made in India may have been linked to acute kidney injuries and the deaths of 66 children in Gambia. The World Health Organization (WHO), investigating the deaths, linked the deaths to use of contaminated cough and cold syrups produced by an Indian drugmaker- New Delhi-based Maiden Pharmaceuticals Ltd. The announcement followed a laboratory analysis that confirmed “unacceptable” amounts of diethylene glycol and ethylene glycol, which can be toxic and lead to acute kidney injury. Cough syrups often have decongestants in them, that make consumers heart disease worse by increasing blood pressure and tachycardia. They may interfere with heart disease medicines if being taken from working right. Dextromethorphan (DXM), an antitussive is an ingredient in most cough syrups that decreases activity in the part of the brain that controls breathing, coughing, and heart function. When abused, high doses of DXM interfere with in receptors in the brain, causing hallucinations, euphoria, and loss of motor control.
Key progress in chronic cough research in recent years has been in the areas of- Effect of cough in the population and at the individual level, Development and validation of measures of cough and cough hypersensitivity, Continuous recordings of cough frequency on a portable app, Mechanisms and treatment of acute infective cough, Production of tussive lipids from Mycobacterium tuberculosis bacilli, Cough hypersensitivity: peripheral and central mechanisms, Cough hypersensitivity: neuroinflammatory mechanisms, Cough hypersensitivity: novel targets, Trials of new antitussives: P2X3 receptor antagonists (The restricted localizations of P2X3 and P2X2/3Rs on nociceptive neurons make them an attractive target for the management of chronic and refractory chronic cough (Gifaxin syrup/tablets, Sivopixant anti-tussive, BLU-5937), sodium channel blocker NTX-1175, opioid nalbuphine, Management of cough associated with gastro-oesophageal reflux disease and Management of chronic cough in children and adults [4]
Case Studies:
4. An adult Community Acquired Pneumonia Case:
A 36-year male reported at a private hospital in a small town of Chintamani, in Kolar district of Karnataka with the complaints of cough with sputum, fever, vomiting, mild diarrhoea, for 3 days on 12/5/2021. Based on Chest Xray and other investigations he was diagnosed as having pneumonia. His treatment consisted of multiple antibiotics and recovered completely after treatment for 5 days. In this case multiple antibiotics were against the standard protocol of pneumonia management recommended in India.
5. A case of CVA:
Third week of December 2023, Rakshana a girl of 17 years was brought to me with complaints of dry cough for over 7 weeks. A general practitioner had tried 2 antibiotics, Amoxicillin and Erythromycin for 5 days each and antihistamines and cough suppressant syrups. Detailed history revealed that the cough was initially productive but became dry cough after treatment with second cycle of antibiotics. Though intensity of the cough had come down, it lingered sometimes disturbing her sleep due to breathlessness. She also reported exaggeration of cough after 2 games of Badminton which she tried last week. An Xray done 3 weeks ago had given clear picture of the chest. Taking a clue from exercise induced Asthma, I put her on fast-acting bronchodilator inhaler, initially for three times a day for 3 days and slowly weaned over a period of one week relieving her of the cough. She was advised to use a corticosteroid inhaler if cough bothers again, but so far, no recurrence.
Covid 19 Cough cases:
We had managed about 23 cases of Covid 19 patients in our apartment complex setting up a covid care centre (CCC) in August 2021 (second wave of Pandemic), all but 3 of them had dry cough as one of the symptoms. Two of them needed hospitalization and Oxygen supplementation and antibiotics. Rest of 18 access the cough was managed by just steam inhalation and Rico fast plus (a combo drug anti-histaminic and antipyretic), thrice a day for the first 2-3 days followed by twice a day for 2 days and one tablet in the night for another 2 days. None of these patients spent more than INR 50 per day.
6. A case of COPD:
An elderly male of 68 years, father of one of the residents moved in our apartment complex in November 2022, was brough me around 2200 hrs. He complained periodical episodes of cough back home in the last 10 years. Clinical examination revealed emphysematous chest and RR was 40/minute and SpO2 was 89. He was put on Budesonide (Pulmicort Flexhaler) inhaler and oxygen supplementation from the Oxygen concentrator and Amoxycillin. The night tided, he was advised to continue inhaler, antibiotics for 5 days and stop smoking completely. Later he was advised use the inhaler regularly till winter lasted and is Off it’s use for last 2 weeks.
4. Discussions:
World Health Organization (WHO) estimates that respiratory infections account for 6% of the total global acute disease burden. The majority (81.7%) of the URTIs are of exclusive viral aetiology, as many as 200 common cold viruses are to blame for the and only 18.3% are of bacterial aetiology (bacteria alone or bacteria + viral co-infections). When an infected person coughs or sneezes, it is transmitted from him/her to the other persons through airborne respiratory droplets. Common Cold, Sinusitis, Pharyngitis, Epiglottitis and Laryngotracheitis are the common URTIs. Lower respiratory tract infections like Pneumonia, Bronchitis and Pulmonary Tuberculosis cause chronic cough and need to ne tackled by treating infections, that are not the focus of this discussion.
From the point of clinical management of cough in smaller settings, are discussed in following categories:
What a patient’s mucus might mean?
Magnitude of the problem of Coughs in India:
1. Acute Coughs:
Figure 1: Pyramid of Incidence of Acute Cough in India
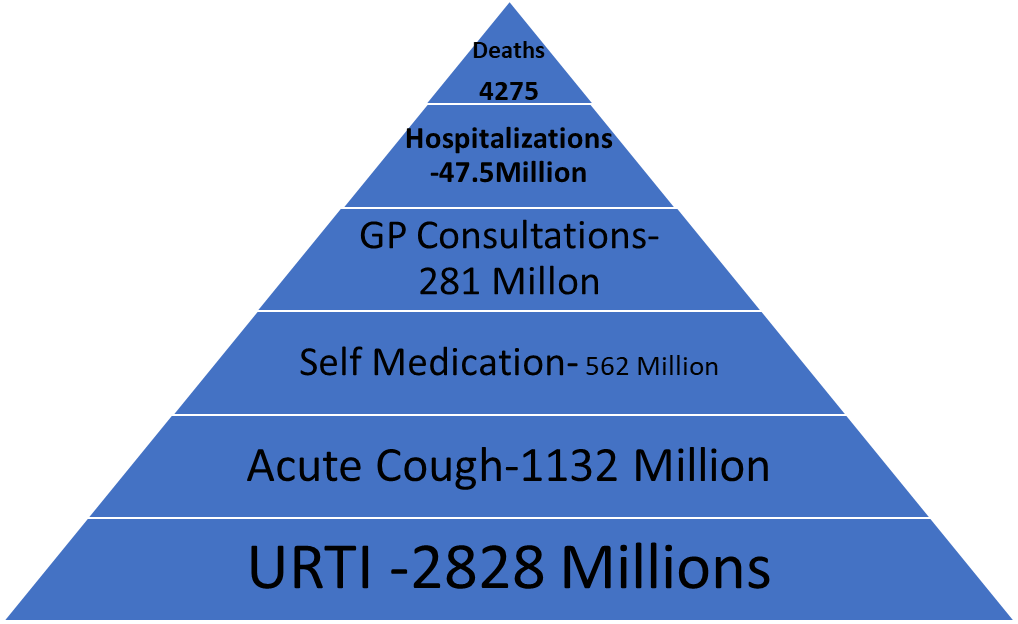
The base represents the population with an upper respiratory tract infection (URTI), some of whom will suffer from acute cough. Level 2 represents all those suffering from acute cough. Level 3 is the proportion of those suffering from acute cough who reach the threshold of severity of cough to trigger the purchase of a cough medicine. Level 4 is the proportion of those suffering from acute cough who reach the threshold of severity of cough to trigger a GP consultation. Level 5 is the proportion of those suffering from acute cough who are admitted to hospital. And Level 6 represent the estimated number of deaths among them. It is not possible to estimate the number of this latter 2 groups. If one accepts the lowest rate of URTI of two episodes per person per year, it works out to a conservative estimate of 1414x2 = 2828 million episodes of URTI in 2023 in India (fig 1). Proportions 120M/48M/24M/12M/2M.
The current population of India as of Monday, January 9, 2023, is 1,414,125,666 (source: Worldometer United Nations data). Considering the Indian population distribution in 2021, 25.78% children in the 0–14-year category, 67.44% in 15-64 age group and 6.78% over 65 years of age and considering an average of 4 episodes for each child and 2 per adult and 5 per senior citizens over the estimated number of episodes of URTI is shown in the table:
Estimated URTI episodes in 2023.
|
Age Group |
Est. Pop. - 2023 |
Epi/per/Year |
Total episodes |
Remarks |
|
0-14 years @ 25.78% |
36.45 million |
4 |
145.8 million |
|
|
14-65 Yrs.@67.45% |
1367.96 million |
2 |
2735.92 million |
|
|
>65 Yrs. @ 6.78% |
9.59 million |
4 |
38.36 million |
|
I. Management of Cough in Adults:
Causes of Acute Cough Box-1
1. Acute cough: Acute cough is defined as one lasting less than 3 weeks, is the commonest presentation in primary care and is most associated with viral upper respiratory tract infection. In the absence of significant co‐morbidity, an acute cough is normally benign and self‐limiting. OPD records of Primary health care facilities across India indicate that Common cold, sinusitis, Pneumonia, Bronchitis are common causes. About 12% are due to upper respiratory tract infection and 8% due to lower respiratory tract infections. Other non-infectious causes of cough are Asthma, CCF, and Pulmonary embolism.
Red Flags for Referral: Box-2
Cough Syncope among elderly population is of cardiac or neurological origin. It is the commonest symptom associated with acute exacerbations and hospitalisations with asthma and COPD [8].
Indications for further investigation include haemoptysis, prominent systemic illness, suspicion of inhaled foreign body, suspicion of lung cancer. Neonatal onset among children, abnormal voice or cough with crying or inability to feed or cough while feeding is red flags for referral.
Acute coughs are recommended to be treated unless red flag symptoms (Box 2) are noticed.
Managing Acute Coughs:
The most annoying part about catching a cold or a cough is “phlegm”, a type of mucus that is produced in the chest. Mucus forms a protective lining in certain parts of our body. In normal quantities protects by trapping irritants or foreign invaders and expel in a cough. More Phlegm or mucus is produced as a response to an irritant from the environment, like allergies, smoke, smoking tobacco and infections, leading to chest congestion, and more lung problems. Excess phlegm or difficulty to expel phlegm can be tackled as per its cause or origin.” steps to help eliminate excess mucus and phlegm are:
1.Avoid smoking: Exposure to smoking and second-hand smoke cause our body to produce more phlegm. Smoking cessation for active smokers is the most important intervention.
2.Drink more water: Staying hydrated is one of the best ways as sufficient hydration with fluids keep the phlegm loose in consistency and makes it easier to expel. At least 6-8 glasses of water every day to get rid of phlegm and mucus.
3. Avoid exposure to dust: People who have allergic tendencies or are asthmatics should avoid exposure to smoke and dust. It could lead to mucus dripping from the back of the nose to the throat and persistent coughing. It is best to avoid places with too much dust and smoke that can reach your lungs, and cause problems.
4. Steam can help: Steam therapy has been a sure-shot remedy practised by many people for decades. This helps even when anti-histaminic fail to reduce congestion, as I experienced in recent episodes. Steam inhalation, controls the running nose and nasal drip leading to reduction in the production of phlegm in the chest as well.”
5. Medicine for Therapy: If none of the above work, opt or doctors should prescribe therapies like nasal decongestants, nebulized medications, or inhalers that help individuals. Advise on techniques to loosen the mucus and provide devices and medicines called expectorants help in productive coughs. Treatment also depends on the cause of the problem, investigating the cause of excess phlegm in individual cases is warranted.
2. Sub-acute Cough: Duration between 3-8 weeks:
Subacute cough following a non-specific viral infection lasting 3–8 weeks is common. However, despite many treatment options there are no systematic reviews evaluating these. A systematically searched PubMed/MEDLINE and the Cochrane Central Register of Controlled Trials in March 2017 for RCTs in adult patients with subacute cough. Six eligible RCTs including 724 patients had assessed montelukast, salbutamol plus ipratropium bromide, gelatine, fluticasone propionate, budesonide, and nociception opioid 1 receptor agonist and codeine. Five studies reported effects on various cough severity scores at various timepoints. No treatment option was associated with a clear benefit on cough recovery or other patient-relevant outcomes in any of the studies or in meta-analyses for cough outcomes at 14 days and 28 days. Reported adverse events were rather mild and reported for 14% of patients across all treatments. Therefore, currently the evidence on treatment options for subacute cough is weak [4].
3. Chronic cough: Chronic cough is defined as one lasting more than 8 weeks. It is reported by 10–20% of adults, commoner in females and obese and accounts for 10% of respiratory referrals to secondary care. Most patients present with a dry or minimally productive cough. The presence of significant sputum production usually indicates primary lung pathology. In chronic cough a heightened cough reflex is the primary abnormality [6,7].
Clinical evaluation of chronic cough: a) A detailed history including a thorough occupational history should be performed in all patients, b) Physical examination should concentrate on the afferent sites identified as most associated with cough and an assessment of health status in general and cough severity. c) Upper airway investigations: Examination of ear, nose and throat should be performed in preference to sinus imaging in patients suspected of having rhinosinusitis, but with persisting cough despite an adequate trial of treatment directed at the upper airway. d) Assessing airway inflammation by is advised: 1. The demonstration of sputum eosinophilia in blood is important for treatment implications and must be attempted. 2. Induced sputum after exclusion of the other common causes. 3. Chest radiograph and 4. Spirometry are mandatory. 5. Bronchial provocation testing be advised /referred to be performed in patients without a clinically obvious aetiology. 6. Bronchoscopy be advised by referral to all patients with chronic cough in whom inhalation of a foreign body is suspected. 7. High resolution computed tomography (CT scan) may be of used in patients with chronic cough when other investigations are normal.
Management of aggravates: Most cases of troublesome cough reflect the presence of an aggravates (asthma, drugs, environmental, gastro‐oesophageal reflux, upper airway pathology), but no single existing diagnostic protocol can be recommended. Cough is unlikely to be due to eosinophilic airway inflammation if there is no response to a two-week oral steroid trial. One of the commonest causes of persistent cough is smoking, that is dose related, and smoking cessation is accompanied by significant remission, therefore must be insisted.
Gastro‐oesophageal reflux disease (GORD)
Rhinosinusitis is commonly associated with chronic cough. There is an association between upper airway disease and cough but a poor association between the various symptoms and cough. There is disparity in the reported efficacy of antihistamines. In the presence of prominent upper airway symptoms, a trial of topical corticosteroid is recommended.
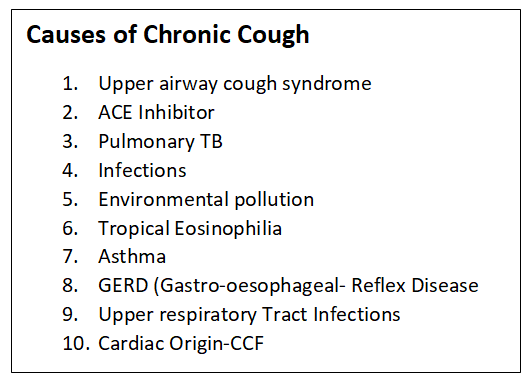
Algorithms (Figs 2 & 3) on next page would help in assessing the chronic cough and manage:
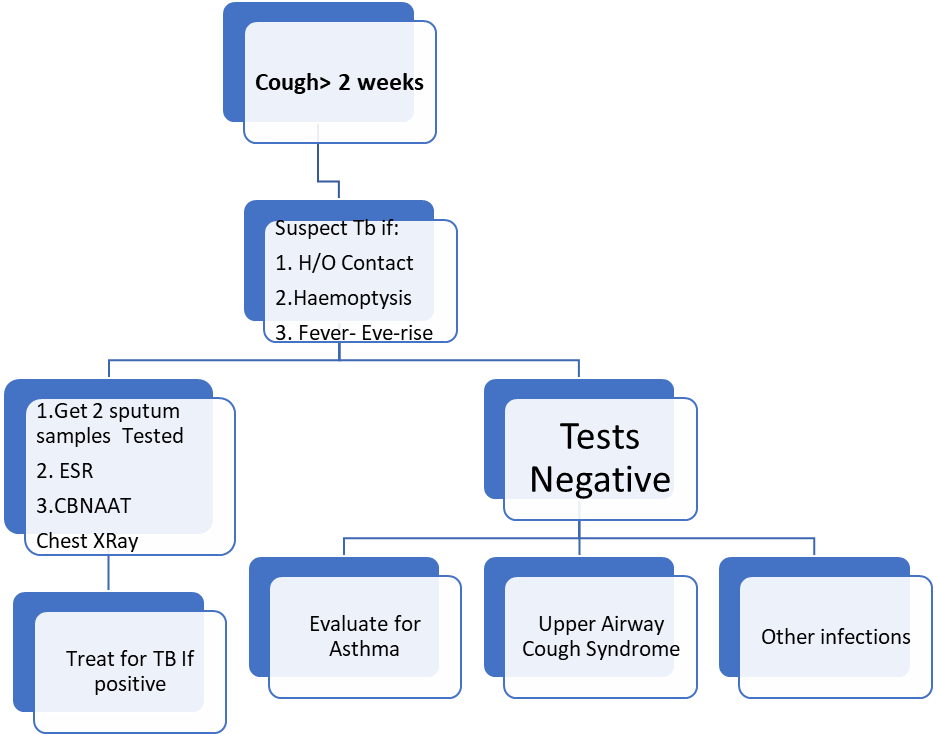
Figure 2: Algorithm for Diagnosis & Treatment of PULMONARY TUBERCULOSIS
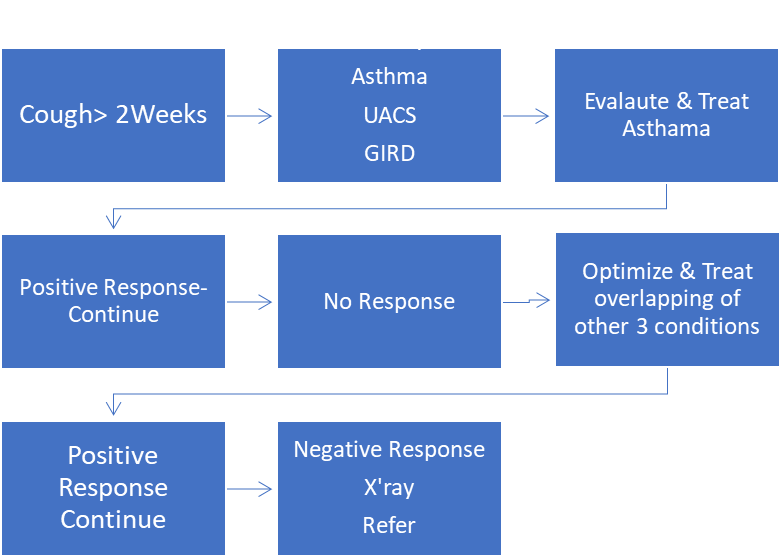
Figure 3: Algorithm for Treatment of ASTHMA, GORD UACS
The most common causes of chronic cough in India are:
Viral Causes of Chronic Cough:
Human Respiratory Syncytial Virus
Human respiratory syncytial virus (HRSV)/RSV is the most common viral cause of ALRI-related death. It is estimated to have 33.1 million cases globally, with about 10% hospitalizations and death of 59,600 children below 5 years of age every year. This amounts to about 22% of all episodes of ALRI and is the cause of the highest childhood mortality in low- and middle-income countries among all respiratory viral infections [3]
Human Parainfluenza Virus
Human parainfluenza virus (HPIV) is a virus from the family Paramyxoviriae with two genera: Respirovirus (HPIV-1 and HPIV-3) and Rubulavirus (HPIV-2 and HPIV-4). Literature from Asia reported a variable prevalence of HPIV ranging from 1 to 66%, with 6.95% as the Indian average prevalence. Estimates for the parainfluenza virus- No data.
Human Metapneumovirus
Respiratory virus infections are highly prevalent in Southeast Asian countries, a preliminary report on the first detection of hMPV in India from a paediatric patient in July to August 2003 by reverse transcription PCR.
Influenza Virus
Infection with the influenza virus is prevalent worldwide and is known to cause around 39 million episodes annually. India, with a tropical climate and variable hygiene practices, experiences a significant number of cases every year. Two strains of this virus are mainly detected: influenza A (INF-A) and influenza B (INF-B). Multiple strains of influenza have emerged in due course, and subtypes H3N2 and H1N1, belonging to INF-A, are the significant ones. Although influenza virus infections are reported throughout the year, a higher number of cases are reported during the rainy season in India. Hence, the higher relative humidity has a role to play in its incubation and spread Influenza B, which is diverse from INF-
Human Rhinovirus
Rhinovirus, although belonging to the Enterovirus family, causes respiratory infections along with gastroenteritis and has been a causal factor for community outbreaks and paediatric respiratory infections in many countries across the globe.
Human Adenovirus
Adenoviruses cause a wide range of illnesses in children and immunocompromised individuals. They start from respiratory symptoms such as the common cold, sore throat, bronchitis, and pneumonia to gastrointestinal disorders such as diarrhoea, vomiting, nausea, and stomach pain.
1. Cough is a forced expulsive manoeuvre, usually against a closed glottis and which is associated with a characteristic sound.
Upper airway pathology
Rhinosinusitis is commonly associated with chronic cough and disparity in the reported efficacy of antihistamines. In the presence of prominent upper airway symptoms, topical corticosteroid can be tried.
Undiagnosed or idiopathic cough
A chronic cough is considered idiopathic following thorough assessment at a specialist cough clinic. The clinical history of reflux cough is often present in patients with idiopathic cough. A typical lymphocytic airways inflammation is seen.
Specialist cough clinics
As no single existing diagnostic protocol can be recommended, A combination of selected diagnostic testing and empirical trials of treatment is likely to be most cost effective. Specialists use fibreoptic laryngoscopy and Bronchoscopy. Specialists may investigate by Bronchial provocation testing in patients without a clinically obvious aetiology for chronic cough and normal spirometry. A negative test excludes asthma but does not rule out a steroid responsive cough. Empirical treatment is offered to patients with cough and typical reflux symptoms before oesophageal testing. Induced sputum should be requested after exclusion of the other common causes. There is insufficient evidence to recommend the routine use of exhaled breath measurements in the clinical evaluation of chronic cough. The demonstration of sputum eosinophilia has important treatment implications and should be available in cough clinics.
For research purposes, standardisation of methodology is required and accurate data on the distribution of cough responsiveness within the population are needed.
Measurement and monitoring of cough
Accurate measurement of cough helps determine cough severity, assess treatment efficacy, and may provide diagnostic information. Ambulatory cough recording currently offers most promise in the objective assessment of cough.
II Chronic Obstructive Pulmonary Diseases (COPD):
There is a lack of national-level estimates on the magnitude of COPD in India. However, a meta-analysis of community-based cross-sectional studies reporting data on the prevalence of COPD among adults based on spirometry, from eight identified studies, (pooled sample of 8,569 individuals), the estimated prevalence was 7.4%. The prevalence was higher among males, in the urban area, and the northern region[8].
Diagnosis: Using spirometry as a diagnostic test for demonstrating non–fully reversible airflow obstruction with a post-bronchodilator FEV1/FVC of < 0.7. Spirometry also establishes the severity of airflow limitation, as defined by the percentage of predicted post-bronchodilator FEV1. This defines the stage of COPD from stage 1 to stage 4.
Treatment decisions, however, are not based on spirometry or stage of airflow obstruction but on symptom burden and the history of exacerbations drive treatment decisions. Severe exacerbations are defined as having required an emergency treatment or hospitalization. Moderate exacerbations are those that require systemic steroids and/or antibiotics but not an ED or hospital admission.
The main treatment goals are reduction of symptoms and the future risk for exacerbations. Two types of inhalers for COPD: i) Bronchodilators are either LAMAs (long-acting muscarinic antagonists) or LABAs (long-acting beta agonists) and ii) Anti-inflammatory inhalers are ICS. Algorithm for patients is identified in groups A, B, and E. Groups A and B represent patients with very few exacerbations — one or fewer moderate exacerbations and no COPD-related hospitalization. Group E included patients who have had significant exacerbations — two or more moderate exacerbations requiring systemic steroids and/or antibiotics, or a hospitalization or ED visit for a COPD exacerbation. Patients in group A have relatively mild symptoms, and a bronchodilator is recommended. Patients in group B have a higher symptom burden and it is recommended to start with dual bronchodilator therapy. Dual-bronchodilator therapy in patients with significant symptoms and escalate to triple therapy if patients have a significant exacerbation burden, meaning two or more outpatient exacerbations or even a single hospital-level exacerbation.
Smoking cessation and vaccination for COVID, influenza, pneumococcal disease, and pertussis (dTaP/dTPa) as well as zoster for patients over 50 years old.
Emphasis on exercise, activity, pulmonary rehabilitation, and oxygen therapy for patients with severe resting chronic hypoxemia.
1. Cough Profile and Trends in Cough Management in Children Across India:
A hospital OPD based survey of 1998 children ((58% males; 41% females, 1% not mentioned) conducted in six cities of Bengaluru-350, Ahmedabad-249, Delhi-403, Mumbai-301, Lucknow -397 and Hyderabad-298 in winter months from October to December 2017 involving 200 paediatricians across India. Data was collected on children having cough, categorized under 6 groups ranging from age 1-2 years to 11-12 years, visiting paediatric OPD / clinics with cough as the chief complaint. The analysis indicated that, over 69% children presented with cough for 5 days prior to OPD visit while only 3% had symptoms lasting over 10 days. ii) Almost half of the children reported 4 to 6 similar episodes of cough in preceding 12 months. More than half of the children had more than 6 bouts of cough per day. iii) 25% of the children were having dry cough whereas 61% had wet cough with no or scanty expectoration. iv) Fever was present as associated symptom in 62.9% cases, v) Majority (77%) of children had no family history of asthma, allergic rhinitis, or tuberculosis. vi)None of them were diagnosed either as pneumonia or tuberculosis on further investigation. vii) First- and second-generation antihistamines were prescribed in 76% and 78% children respectively. viii) Antibiotics (50%) and nutritional supplements (12%) were prescribed ix) mucolytics (62%) and expectorants (63%) were given. x) 83% of children preferred oral medicine. xi) Use of self-medication was however low [7,9].
Decongestants, antitussives, mucolytics, expectorants and first- and second-generation antihistamines were commonly prescribed in management of paediatric cough with a view to decrease mucosal oedema, secretions, and allergy. Due caution needs to be observed while prescribing multiple and multi-combination preparations so that same molecule is not present in different preparations, to avoid overdosing.
For children under 5 years the National Health Mission advocates use of IMNCI strategy, that was designed jointly with the help of UNICEF India country office. Most of the country’s public health system was trained in early 2002-2005.However the strategy is partially successful for want drugs and logistics and on job supportive supervision. The summary of the strategy is narrated in following paragraphs.
ASK ABOUT MAIN SYMPTOMS: Does the child have cough or difficult breathing? IF YES, ASK: • For how long?
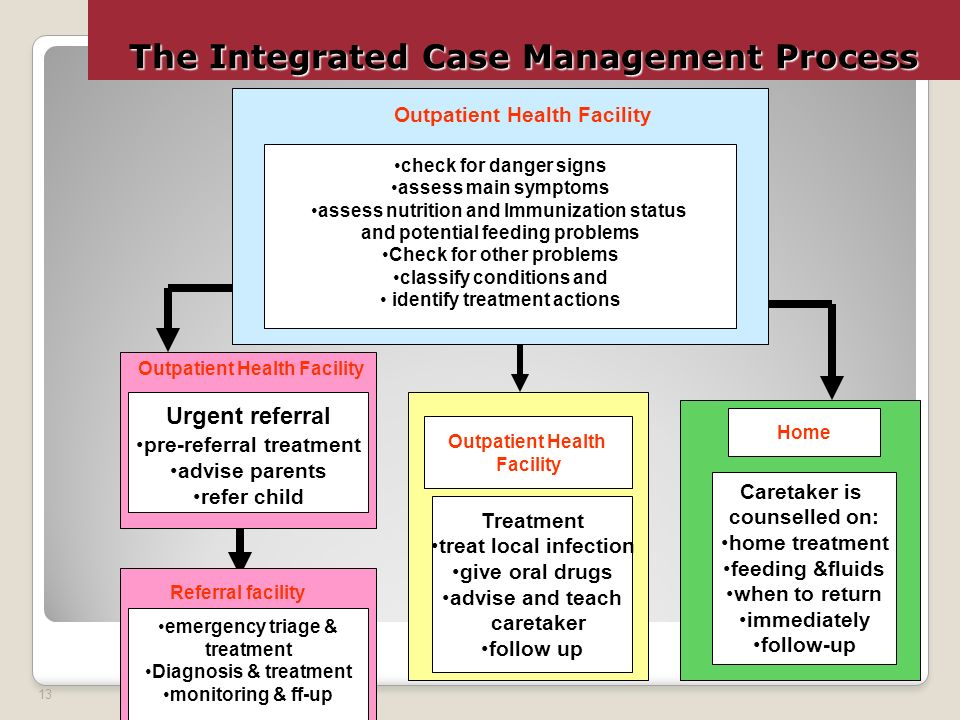
I Child Younger than 2 Months Old:
I Child Younger than 2-60 Months Old: Physical Examination after making CALM.
If NO: i) Count the breath for 1 minute ii) Look for chest indrawing 3. Look & listen for Stridor.
Fast breathing Yes, if i) up to 2 months age up to 12 months 50 breaths per minute or ii) If the child is >12 months to 5 years - up 40 breaths per minute or more.
If Fast breathing- Yes Diagnosis> PNEUMONIA
Treatment: Give Amoxycillin for 5 days. Soothe the throat and relieve the cough with a safe remedy if child is 6 months or older. Advise mother when to return immediately. Follow-up in 2 days.
3) If no fast breathing or other signs of pneumonia, diagnosis is - NO PNEUMONIA: COUGH/ COLD
If coughing more than 30 days, refer for assessment. Soothe the throat and relieve the cough with a safe home remedy if child is 6 months or older. Advise mother when to return immediately. Follow-up in 5 days if not improving.
Acute respiratory infections (ARIs) continue to be the most important cause of morbidity and mortality among under-five children. A recent study conducted in 16 selected clusters from the rural areas and densely populated urban slum areas of the two districts- Pune & Sangli in Maharashtra, India. A total of 3,671 under-five children were surveyed. The prevalence of ARIs for the preceding month was 50.4%. It was higher among the children living in the rural areas (54.2%) compared to the children living in the urban areas (46.7%) (p = 0.01). The prevalence of ARIs was reported to be 51.4 and 49.4% in boys and girls, respectively. In the multivariate analysis, the researchers found that living in rural areas (p = 0.01) and parental smoking (p = 0.04) were significantly associated with the ARIs. An intervention such as reducing parental smoking habits at the household level may reduce ARIs. Structured and validated proforma was used for collecting the data on the sociodemographic and household environmental risk factors [5].
III. Cough in Pregnancy- Causes and Management:
1. Gastroesophageal Reflux (Acid Reflux): About two-thirds of pregnant women develop indigestion and acid reflux. It is the most common cause of cough in pregnancy, contributing to almost 77 % of the cause. Backward movement of the food and acidic contents of the abdomen into the food pipe and the throat, leaving bitterness in the mouth. It occurs due to extra-abdominal pressure or due to lower physical activity and improper diet.
2. Bronchial Asthma: Bronchial asthma is the second most common cause of cough in pregnancy, contributing to 12% of the cases. The hormonal and physical changes are the causes of bronchial asthma during pregnancy.
3. Bronchitis: The compromised immunity during pregnancy, exposes pregnant women to bronchioles' inflammation / infections resulting in cold and bronchitis, and contributes to 7 % of all the causes of cough in pregnancy.
4. Allergic Rhinitis: The prevalence of all types of rhinitis during pregnancy is 10 to 30 %. The hormonal imbalances / compromised immunity are the contributors to rhinitis in pregnancy.
Home Remedies for Cough During Pregnancy:
Due to improper diet, inadequate sleep, and physical activity, compromised immunity is the main underlying cause of infections and allergies leading to coughing in pregnancy. Home remedies for cough include eating a healthy diet rich in antioxidants, vitamins, and minerals such as zinc and increasing physical activity in the form of exercises and yoga. Quality sleep is an essential component in improving overall immunity. Using a mask, preferably made of cotton cloth, to avoid allergens such as dust and other pollutants also help. Regular Exercise that improves blood circulation and increases immunity and prevents the risk of infections. Dehydration during pregnancy increases the risk of constipation, infections therefore appropriate rehydration periodically is necessary to help body fight infections. Avoiding heavy meals that increases the risk of acid reflux, and aggravation of cough during pregnancy is also advocated. Similarly, avoiding direct or indirect (using shared clothes and towels) contact with people including spouse /child having Flu-like Symptoms prevents from contracting the cough and cold. Other home/ ISM remedies recommended in India include:
When to refer:
A pregnant women with cough needs to be referred if she has danger signs like i) Inability to sleep or feeling sleepy frequently, ii Not feeling to eat anything, iii) Suffering from a 1020 F- fever, iv) Facing chest tightness and pain while coughing or v) Blood mucus from cough
Acute Coughs: Diagnosis of the cause of the acute cough is important not only for the patient’s treatment, but also to limit the spread of infection [5,10]. Acute Rhinitis, Rhinosinusitis, Laryngitis, Tracheobronchitis, Pneumonia are common causes.
1. Acute Rhinitis and Rhinosinusitis: Cough is induced by inflammation or irritation of the Nostrils, Pharynx, larynx, trachea, if the infection extends into lower respiratory tract, it either stimulates mechanically or chemically to produce cough. Postnasal Drip (PND) is the cause of cough in acute rhinitis and rhinosinusitis. The viruses that commonly infect the nose and upper respiratory tract are rhinovirus, adenovirus, and coronavirus.
In a prospective study of patients aged 60–90 years with RTIs, LRTIs as defined by the presence of cough, wheezing and/or chest pain, and URTIs by their absence; 65% of patients had LRT symptoms and 98% URT symptoms. Thus, 66% of patients with ‘rhinitis’ also had LRTI including the symptoms of cough. The commonest pathogens were rhinovirus (52%), coronavirus (26%) and influenza virus (10%). About bacterial infections, 70% are due to Streptococcus pneumoniae or Haemophilus influenzae, Moraxella catarrhalis [5,10].
2.Acute Laryngitis: URTI frequently, leads to cough or expiratory efforts. If the cough is dry, the ‘urge to cough’ may be due to the irritation of the laryngeal sensory receptors.
3.Acute Viral Tracheobronchitis: The viruses that usually cause acute rhinitis (rhinovirus, adenovirus, and coronavirus) but not LRT, contribute frequently to LRTI, in the elderly. Rhinovirus infection is the most common cause of acute exacerbation of asthma, and a major cause of acute exacerbation in COPD and CCF.
4.Bacterial Pneumonia: About 5–10% of elderly patients with acute tracheobronchitis develop pneumonia (CAP) with a bacterial infection deep in the lungs. The most common agents for pneumonia in elderly patients are Mycoplasma pneumoniae, Chlamydia pneumoniae and B. pertussis, H. influenzae, M. catarrhalis and Staphylococcus aureus. S. pneumoniae and H. influenzae are the most frequent bacterial pathogens causing acute bronchitis in elderly patients.
Diagnosis: In the great majority of patients, is by history and physical examination and only a small minority of patients, may require more sophisticated tests as the symptoms may be masked and more detrimental due to aging processes.
Treatment: Hospitalisation and ventilatory support may be urgently required, with or without chemotherapy. It should be noted that repeated and vigorous coughing may have adverse effects on the elderly patient. These effects include incontinence (especially in females), rib fractures and vagally mediated cardiac instabilities.
B. Chronic Coughs in Elderly People:
Cough >3 few weeks, thick, greenish-yellow phlegm, wheezing and with a fever in elderly need attention. Postnasal Drip (PND) is considered as an important aetiological factor in chronic cough. Chronic night-time coughing is a symptom of heart failure, as well as bronchitis, pneumonia, and COPD. Lung cancer / blood clots in the lungs are less common, causes of severe coughs.
Assessment: Clinical examination and patient history, supplemented by chest X-ray, viral and bacterial culture and serological testing are essential. Specific antibacterial therapy after culture and sensitivity tests, but in cases of uncertain diagnosis not advocated.
Management: Antibacterial, Bronchodilators (β-adrenoceptor agonists), shorten the duration of cough in patients with bronchial wheezing, but are not effective in the absence of airflow limitation. Corticosteroids, humidified air, and drug guaifenesin have no effect. Non-specific antitussive (opioids and dextromethorphan) therapy is common, and desirable to prevent the adverse effects of repeated coughing. The first-generation antihistamines may have a stronger antitussive action than the second-generation drug.
Prevention and prophylaxis for influenza and S. pneumoniae infections are useful in the elderly, especially those in communities [6].
V. Cough in Covid 19 Patients:
Since early 2020 Covid 19 infection has been the most common cause of Cough. It manifested both in acute stage and in Long Covid 19 and started in 2-14 days after exposure to the virus. As both COVID-19 and the common cold are caused by viruses spread in similar ways and cause many of the same symptoms and it is difficult to differentiate clinically. Most people experienced dry cough with a tickle in the throat or as irritation in their lungs in the initial infection. Some people continued to have a cough with phlegm in what is called Long Covid for as long as 6 months if contracted Omicron variant of Covid 19 as it is more airway dependent than the original strain. Such cough was managed by keeping hydrated with lukewarm water, broths, soups, herbal teas and Kadha. If the cough was productive steam inhalation at least thrice a day to loosen the phlegm congested in lungs was promoted. Cough suppressants medicines (antitussives), like dextromethorphan (Robitussin, Delsym), were prescribed to control cough reflex. They usually work better for a “dry” (non-productive) cough, which usually results from irritation. Medicines containing expectorants like guaifenesin, such as Robitussin, Mucinex, and Vicks 44E were prescribed for promoting expectoration. People with asthma and other lung diseases needed to cough as it brought out mucus from the lungs and helped prevent bacterial infections. The clinicians either investigated in detail or referred a cough for more than 3 weeks, if cough was severe or there was blood in sputum or patient experienced shortness of breath, breathing difficulties or chest pain. Then a CT scan of the chest, that revealed opaque spots in lungs that soon started connecting to each other, confirmed pneumonic consolidation. As COVID-19 are contagious; disposal of sputum is very important and ensuing that the sink where you dispose of your sputum is regularly disinfected. Lie on either the left or the right side, instead of lying on your back as it helps to drain the phlegm faster [11].
VI. Cough Variant of Asthma (CVA):
Cough-variant asthma is a type of asthma in which the main symptom is a dry, non-productive cough lasts longer than 6-8 weeks. People with cough-variant asthma often have no other "classic" asthma symptoms, such as wheezing or shortness of breath. The coughing with asthma can occur during the day or at night interrupting sleep often complaining that cough increases with exercise, (exercise-induced asthma). Coughing increases on exposure to asthma triggers- dust / strong fragrances, or cold air. Though anyone can get cough-variant asthma at any time, it is common in young kids with childhood asthma, before leading to the development of "classic" asthma. A cough that begins after a person has begun taking beta-blockers to treat high blood pressure, heart disease, heart failure, migraines, palpitations, and other conditions is likely to be cough-variant asthma. Beta-blockers are also found in eye drops to treat glaucoma and other eye problems. Aspirin-sensitivity is another cause of coughing with asthma.
Asthma medications such as i) fast-acting bronchodilator inhaler, which expands the airways in the lungs and offers quick relief, or ii) a corticosteroid inhaler, used daily relieves inflammation and helps to relieve the coughing attacks [12].
VII. Drug Induced Cough:
Angiotensin converting enzyme (ACE) inhibitors, such as Cardace, Envas, Coversyl, Ramistar, and Ramipril are prescription drugs used to treat high blood pressure have one of the most common side effects as chronic dry cough. The only effective treatment for ACE inhibitor-induced cough is the cessation of treatment with the offending agent [13].
Recent advances:
Extracellular adenosine 5’-triphosphate (ATP) acts as an autocrine and paracrine agent, the actions of which on affected cells are mediated by P2 receptors (P2R). In the lungs and airways, ATP activates P2X3, and P2X2/3 receptors (R) localized on vagal sensory nerve terminals resulting in bronchoconstriction, and cough, and localized release of pro-inflammatory neuropeptides via the axon reflex. Currently, several P2X3R and P2X2/3R antagonists are being developed as drug-candidates for the treatment of chronic cough. P2X3 Receptor Antagonist Eliapixant (200 and 750 mg) produced plasma concentrations that cover the predicted therapeutic threshold over 24 h, with good safety and tolerability, enabling it to progress to clinical trials in patients with refractory chronic cough[13].
Merck’s Gefapixant was approved for use in USA in September 2020. In mid-June 2022, the Japan Ministry of Health, Labour, and Welfare (MHLW) approved LYFNUA® (gefapixant) Tablets 45 mg BD, for adults with refractory or unexplained chronic cough.