Thierry Sibomana1, Daniel Nduwayo2, Ramadhan Nyandwi3, Romeo Irankunda4, Jean Claude Mbonicura5, Davy Carmel Iraduhezagiye1, Kamamfu Gaspard1
1Department of Pneumology,University of Burundi,Faculty of Medicine,Bujumbura,Burundi
2Department of Neurology, University of Burundi,Faculty of Medicine,Bujumbura,Burundi
3Department of General Laboratory, University of Burundi,Faculty of Medicine,Bujumbura,Burundi
4Department of Nephrology, University of Burundi,Faculty of Medicine,,Bujumbura,Burundi
5Department of General Surgery, University of Burundi,Faculty of Medicine,,Bujumbura,Burundi
*Corresponding author: Thierry Sibomana,University of Burundi,Faculty of Medicine,Pulmonology department.
Received date: February 21, 2023
Accepted date: May 20, 2023
published date: July 17, 2023
Citation: Sibomana T, Nduwayo D, Nyandwi R, Irankunda R, Jean C Mbonicura. (2023) “ Epidemiological, Therapeutic and Evolutionary Analysis of Tuberculous Pneumothorax in Bujumbura Hospitals. Case of the Chuk ”. International Journal of Epidemiology and Public Health Research, 3(2). DOI: http;//doi.org/01.2023/1.1042.
Copyright: © 2023 Thierry Sibomana. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Aim: To determine the epidemiological, therapeutic and evolutionary aspect of the pneumothorax and pleuropulmonary tuberculosis association at the CHUK.
Patients and Methods: This is a retrospective descriptive study over a period of 5 years from January 1, 2017 to May 1, 2021 and prospective over a period from May 1, 2021 to April 1, 2022 carried out in the internal medicine (IM) and anaesthesia-resuscitation departments of the University Hospital Center of Kamenge (CHUK),
Results: During the study period, 250 cases of pleuropulmonary tuberculosis were collected, of which 20 presented an association of tuberculosis and pneumothorax, i.e. 8% frequency. The majority were men (n = 13) with a sex ratio of 1.8 and an average age of 41.5 years. The treatment combined antituberculosis chemotherapy (n = 20), chest drainage (n = 19), respiratory physiotherapy (n = 13), and oxygen therapy (n = 11). The use of therapeutic surgery was indicated in 3 cases but only one patient was operated on by pleural decortication. The evolution was favorable in 13 patients (65%) of which 12 however kept sequelae of pachypleuritis; and it was unfavorable in 6 patients: 2 cases of recurrence, one of whom also developed complications such as pyopneumothorax with parietal suppuration and fall of the drain and 4 cases of death.
Conclusion: The association pneumothorax and pleuropulmonary tuberculosis remains a real public health problem. However, it is a serious complication associated with pleuropulmonary sequelae; it is most often secondary to a delay in management or inadequate treatment of the tuberculosis disease. Its treatment remains difficult, marked by invasive treatments and sometimes late recourse to surgery, hence the need for its prevention and good care.
Introduction
Tuberculosis is still a public health problem today. A third of the world's population is affected, eight million people develop tuberculosis every year. Two to three million patients die of tuberculosis each year [1, 2]. also in some developed countries. This progression is related to the increase in poverty in the world and the emergence of HIV infection.
Spontaneous pneumothorax is a public health problem[3] and remains a significant condition in respiratory pathology, often being associated with pulmonary tuberculosis. Despite the fact that literature data on pneumothorax are rare in sub-Saharan Africa, according to studies already done in Mali[4], Cameroon[5] and Senegal[6] , pulmonary tuberculosis, which is an endemic disease in this region, the etiologies of secondary spontaneous pneumothorax dominate, hence the pneumothorax-tuberculosis association becomes an interesting subject for research
Indeed in Burundi, also, tuberculosis is still a major public health problem and is rampant in endemo-epidemic form; during the year 2020, 7,215 cases of tuberculosis of all forms were detected throughout the country[7]. But concerning pneumothorax, to date there is no data relating to it in the country, hence the strong interest of our study.
Our study aimed to study the epidemiological, therapeutic and evolutionary aspects of the association of pleuropulmonary tuberculosis and pneumothorax in a hospital environment in Bujumbura.
Methodology
This is a retrospective descriptive study over a period of 5 years from January 1, 2017 to May 1, 2021 and prospective over a period from May 1, 2021 to April 1, 2022 carried out in internal medicine departments (MI) and Anesthesia-Resuscitation of the Kamenge University Hospital Center (CHUK)
Were included, all patients hospitalized in these services and suffering from pneumothorax whose association with pleural and/or pulmonary tuberculosis was confirmed bacteriologically (positive bacilloscopy and/or positive culture) or by a good evolution under anti-tuberculosis treatment of test. The information collected focused on socio-demographic, therapeutic and evolutionary aspects. They were entered and analyzed using Microsoft software and epi-info 7
Results
During the study period, 250 cases of pleuropulmonary tuberculosis were collected, of which 20 presented an association of tuberculosis and pneumothorax, i.e. 8% frequency and 60.6% of all pneumothorax treated in the same period. (33 Cases of pneumothorax). The majority were men (n = 13) with a sex ratio of 1.8 and an average age of 41.5 years. The treatment combined antituberculosis chemotherapy (n = 20), chest drainage (n = 19), respiratory physiotherapy (n = 13), and oxygen therapy (n = 11). The use of therapeutic surgery was indicated in 3 cases but only one patient was operated on by pleural decortication. The evolution was favorable in 13 patients (65%) of which 12 however kept sequelae of pachypleuritis; and it was unfavorable in 6 patients: 2 cases of recurrence, one of whom also developed complications such as pyopneumothorax with parietal suppuration and fall of the drain and 4 cases of death.
Table I: Distribution of patients according to age group
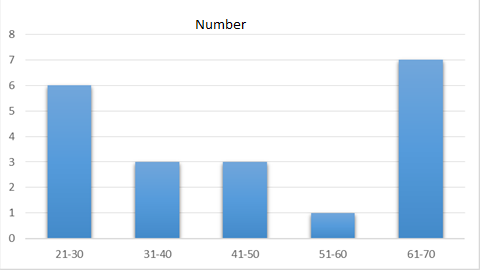
Table 2: Evolution under treatment
|
Evolution |
Number |
Percentage(%) |
|
Favorable |
13 |
65 |
|
Death |
4 |
20 |
|
Recurrences |
2 |
10 |
|
Pyo pneumothorax |
1 |
5 |
Discussion
In our study, cases of pneumothorax-pleuropulmonary tuberculosis association represented 8% of all cases of pleuropulmonary tuberculosis who were hospitalized in the department during our study period (250 cases of tuberculosis). In the series by Singh et al.[8], it represented 33.33% of the patients in the study.
Compared to pneumothorax, this pneumothorax-tuberculosis association represented 60.6% of all pneumothorax treated during the same period (33 cases of pneumothorax). These data are similar to those of Razafindrakoto et al.[14] who objectified that tuberculosis was the main cause of pneumothorax; it represented 65% of pneumothorax treated during the period of their study, which makes this condition a public health problem and a brake on economic development
The male predominance found in our study (Sex-ratio=1.8) resembled those of Mezghani et al.[9] and those of Taleb et al.[10]. This predominance follows the epidemiology of the pneumothorax-tuberculosis association in most African countries and other data in the literature. In our study, the average age found was 41.5 years and was close to that noted by Singh et al.[8] and that of Ben Saad et al.[11]
Curative treatment of pneumothorax combines general treatment based on antituberculous drugs and local treatment using pleural drainage and respiratory physiotherapy. Surgery is reserved for cases of failed drainage and other complications. . In our study, 95% benefited from chest drainage and the effectiveness of drainage (return of the lung to the wall) is variable during tuberculous pneumothorax. In our series, a return of the lung to the wall was obtained in 75% of drained patients, in that of Mezghani et al[9], it was obtained in two thirds. The duration of the drainage varies from a few days to a few weeks and essentially depends on the permanent maintenance of the lung against the wall. In our series the average duration of drainage was 5.3 days (extreme 1 to 15 days) while in that of Mezghani et al [9], the average duration of drainage was 29 days (extreme 3 and 90 days)
Poly general anti-tuberculosis chemotherapy constitutes the etiological therapy without which the results of the management of tuberculous pneumothorax would be uncertain. In our study, all the patients received anti-tuberculosis chemotherapy and we did not face the problem of resistance to anti-tuberculosis drugs.
The value of respiratory physiotherapy during pneumothorax, even in its simple form (without associated fluid effusion) is certain for many authors [12] [13]. In our study, respiratory physiotherapy was performed in 13 patients ( 65%). It gave fairly good results in the 13 patients, but 12 of them retained fairly significant pachypleuritis. In the series by Mezghani et al[9], it was undertaken in 18 patients (78.2%) with satisfactory results in two thirds of the cases.
The sequelae of pachypleuritis can be explained by poor patient compliance or by partitioning and rapid thickening of the pleura during the acute period.
In our study, the surgical treatment was indicated in 3 cases, but only one patient benefited from a surgical treatment by pleural decortication but with recurrence, the 2 other patients died before the intervention. These 2 patients presented a strongly altered general condition and preoperative assessments (non-encouraging coagulation assessment) which did not allow the realization of a decortication. In the series by Ben Saad et al.[11] the surgical intervention was indicated in 10.7% and was carried out in 9.2%, one patient having refused to undergo the intervention; in the series of Mezghani et al.[9] it was performed in 5 cases (21.5%) including 4 for drainage failures
In our study, the evolution was more or less favorable in 13 patients (65%) but 12 patients (60%) of them kept quite a lot of pachypleuritis but were discharged. There were 2 cases of recurrence, of which 1 patient also developed complications such as pyopneumothorax with parietal suppuration from the point of drainage and fall of the drain, 4 cases (20%) of death were recorded, 1 case (5 %) lost sight of. We also find cases of loss of sight in other series such as that of Mezghani et al[9] and that of Sebbar et al[14], with respectively 8.5% and 25% of loss of sight.
Conclusion
The association pneumothorax and pleuropulmonary tuberculosis remains a real public health problem. However, it is a serious complication associated with pleuropulmonary sequelae; it is most often secondary to a delay in management or inadequate treatment of the tuberculosis disease. Diagnosis and early management of tuberculosis disease will certainly reduce this prevalence and limit their complications.