International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Mariano Votta1*, Bianca Ferraiolo 2, Maira Cardillo 3, Neda Milevska-Kostova 4
1Director of Active Citizenship Network, c/o Cittadinanzattiva APS. Via Cereate, 6 - 00183 Rome, Italy
2Head of the Representative Office to the EU, Senior Manager EU Affairs Active Citizenship Network, Rue Philippe Le Bon 46, 1000 Brussels, Belgium.
3Junior Project Manager, Active Citizenship Network, c/o Cittadinanzattiva APS, Via Cereate, 6 - 00183 Rome, Italy.
4President of IAPO Patients for Patient Safety Observatory, Vice Chair of International Alliance of Patients Organizations & Vice President of Health First Europe, 49-51 East Road London, United Kingdom.
*Corresponding author: Mariano Votta, Director of Active Citizenship Network, c/o Cittadinanzattiva APS. Via Cereate, 6 - 00183 Rome, Italy.
Received Date: March 28, 2022
Accepted Date: March 04, 2022
Published Date: April 11, 2022
Citation: Votta M, Ferraiolo B, Cardillo M, Neda Milevska-Kostova. “Encouraging Across Europe the Civic & Patient Advocacy Groups’ Engagement in The Implementation of National Resilience and Recovery Plans to Reduce the Burden of Covid-19 Pandemic on Ncds Patients’ Therapeutic Adherence”. International J of Epidemiology and Public Health Research, 2(1). DOI:http;//doi.org/03.2022/1.1028.
Copyright: © 2022 Mariano Votta. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
In 2002, Active Citizenship Network (ACN) [1], together with organizations from 15 EU countries, established the European Charter of Patients’ Rights [2]. Since then, the Charter has become a reference for establishing and strengthening EU citizens’ rights in nations’ healthcare , linking the adherence to therapy to several of the 14 fundamental patients’ rights listed by the Charter: the right to access to care, the right to information, the right to preventive measures, the right to consent and the right to personalized treatment. Furthermore, the Charter has acted as a milestone for the drafting of the “European Charter on Adherence to Therapy” [3] in November 2016, recognizing not only the fundamental role of Europe and its Member States in increasing the level of adherence to treatment to improve the citizens’ quality of life , but also making explicit that adherence to treatment is a basic right of chronic patients. Properly training and informing chronic patients includes them in a process of empowerment that allows them to follow at their best the treatment given by the physician and, at the same time, to prevent any worsening of their condition. Cittadinanzattiva [4], through its European branch Active Citizenship Network, has decided to actively commit on the topic of therapeutic adherence [5] by carrying out, in the second half of 2021, a EU online survey [6] with the aim to better contribute, starting from citizens’ and patients’ perspective, on understanding the impact that the COVID-19 pandemic has had on the therapeutic plans for chronic patients across Europe. The data and recommendations collected, showing the inadequate attention of institutions and the main stakeholders in relation to access and continuity of care for non-Covid-19 patients, are hosted in the following article. In the latter, a hypothesis is advanced recognizing how the economic resources provided by the National Resilience and Recovery Plans (NRRPs) can also play a key role in enhancing the therapeutic adherence for patients with chronic disease.
Introduction
As highlighted by the Charter on Adherence to Therapy, by 2025, over 20% of the Europeans will be 65 or older and the number of octogenarians will rapidly increase [7]. The raising life expectancy obviously represents a positive effect of the progress in prevention and care, but also implies a challenge for Health Services, due to the complexity of health needs of the elderly. Rising life expectancy makes care and, in particular, access to medicines and appropriateness in their use a challenging task at different levels: individual, societal and institutional. We know by now that the fundamental conditions for active and healthy aging include not only prevention and adoption of healthy lifestyles, but also adherence to medical treatment and pharmaceutical prescriptions. Typically, the elderly reveal co-existence of multiple chronic and clinical conditions that can’t be ascribed to a specific disease and frequently have multiple causes, exposing the patient to the great issue of polypharmacy [8].
Among patients with chronic illnesses, approximately 50% do not take medications as prescribed. This high level of non-adherence results in higher healthcare costs, lower quality of life and poorer health outcomes, which make this phenomenon a major concern for public health. It is estimated that each year the poor adherence to medication in Europe causes about 200,000 deaths and burdens on health expenditure up to 80 billion euro [9]. These data were collected prior to the Covid-19 pandemic, which has only worsened the already critical situation, triggering multiple problems for individuals suffering from non-communicable diseases (NCDs) and chronic conditions. These patients living were indeed more likely to suffer more severe consequences of Covid-19 compared to healthy individuals, including a higher risk of hospitalization, complications, and mortality. The infection-control measures furthermore led to difficulties for these patients to access adequate treatment, medication, and care. During the first wave of the Covid-19 pandemic in 2020, many nonurgent outpatient services were closed to patients with NCDs and chronic conditions and appointments were cancelled or postponed to both reduce the risk of infection for patients and healthcare personnel and to ease the burden on national healthcare systems [10]. These infection- control protocols had direct and indirect relevant implications for short- and long-term health, disease management, and quality of life of patients with NCDs, leading to higher chances of poorer clinical outcome. Poor medication adherence to drugs treating NCDs, especially, increased because of the pandemic-related circumstances, including lack of medications, reduced access to pharmacies, and a decrease in healthcare professionals’ services for medication control and adjustment [11]. Indirectly, the negative impact has affected the national healthcare systems as a whole, including more outpatient visits and higher use of healthcare costs, among others.
Prior to the COVID-19 pandemic, the topicality and urgency of therapeutic adherence had been highlighted during the 12th European Patients’ Rights Day [12], promoted by Active Citizenship Network on May 23, 2018, in the European Parliament in Brussels. The event was an occasion to foster communication among different actors in the healing and caring process to improve adherence to therapies and commit to increase the respect of patients’ rights and their involvement as fundamental active partners with health professionals in their own care, respecting the fundamental values recognized by the European Charter of Patients’ Rights. Starting from concrete experiences, good and failed practices, the conference provided patient associations, healthcare professionals, scientists, industry and representatives of national and European institutions with the opportunity to work together in identifying main necessary changes to address non-adherence to treatment plans. Soon after the celebration of the 12th European Patients’ Rights Day, on February 15, 2019, the European Parliament called for a motion for a resolution on the establishment of a ‘European Adherence to Therapy Day’ [13] in order to raise awareness of the negative impact of a lack of adherence to therapy and the benefits of greater adherence as a key aspect of quality, personalized healthcare. The proposal was advanced having in mind how much recent demographic trends pose a challenge to health systems, with a growing proportion of elderly citizens having to manage comorbidities and chronic diseases. The adverse impact of the lack of adherence to therapy on patients’ quality of life, which increases the risk of undesirable events and hospital admissions, and its economic impact, causing inappropriate health spending, were also considered. On these bases Cittadinanzattiva, through its European branch Active Citizenship Network (ACN), has decided to realize an European communication campaign titled “From Therapeutic Adherence to Therapeutic Alliance” [14] with the direct involvement of 11 national advocacy groups and patients associations’ leaders, as well as of two umbrella organizations. Keeping in mind the worsening impact of the Covid-19 pandemic on therapeutic adherence across Europe, ACN has also investigated the topic through a civic survey titled “The impact of the Covid-19 pandemic on non- communicable and chronic patients’ therapeutic adherence across Europe”, carried out at the European level during the second half of 2021.
Poster realized in occasion of the 12th European Patients’ Rights Day, promoted by Active Citizenship Network, on May 23, 2018, in the European Parliament in Brussels and focused on therapeutic adherence
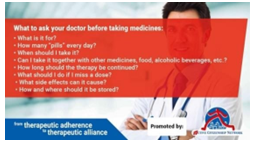
Banner realized in 2018 in occasion of the European communication campaign titled “From Therapeutic Adherence to Therapeutic Alliance”.

Leaders of patients’ advocacy groups involved by Active Citizenship Network in the 2018 European communication campaign “From Therapeutic Adherence to Therapeutic Alliance”.
YouTube video realized in 2018 in occasion of the “From Therapeutic Adherence to Therapeutic Alliance” European communication campaign.
Cover image of the EU civic survey titled “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe” realized by Active Citizenship Network in the second half of 2021.
Methods
In line with its long-term commitment on therapeutic adherence, ACN has launched during the second half of 2021 an EU project with the aim to better contribute –from citizens’ and patients’ perspective – to the understanding of the impact of the COVID-19 pandemic on the therapeutic plans for chronic patients. This project, titled “Therapeutic adherence during the COVID-19 pandemic across Europe: impact, experiences and perspectives from PAGs & relevant stakeholders”, consisted of creating, implementing, and disseminating an EU online survey, with the contribution of a scientific committee, to collect information from patients’ advocacy groups (PAGs) and patient organizations from different European countries. The questionnaire comprised of questions about the impact that Covid-19 has had on the adherence to therapies of patients with chronic conditions and NCDs and their access to healthcare systems in the different national contexts across Europe. The decision for implementing this survey was taken with several objectives: hear directly from patient associations and PAGs about the needs and difficulties experienced by patients with whom they are in touch; enhance actions and reactions implemented by all the relevant stakeholders due to the restrictions that the pandemic imposed; intercept problems and phenomena that still didn’t emerge or on which there is not enough attention in the public debate, in order to present them to experts and institutions.
The anonymous questionnaire was structured in four parts: Part 1 - General information; Part 2 – Continuity of care during the Covid-19 pandemic; Part 3 – Actions and re-actions during the pandemic on continuity of care & therapeutic adherence; and Part 4 – Patient engagement & concrete proposals for the coming years. Questions were structured as multiple-choice or open- ended, asking respondents to take into consideration necessities of their entire association, as well as their own experiences.
Although the activity was carried out at the European level, the results also included the extra European perspective of Israel, which has been acting as a positive example by distinguishing itself for its exceptional management of Covid-19 in the healthcare sector.
Results
PART 1 – General info on the respondents
The survey was opened between 14 November and 9 December 2021 during which it was completed by 38 organizations, mostly patient-led (45%), patient advocacy organizations (29%), or civil society organizations working with and for patients (21%), from 18 different EU plus one extra-EU (Israel) countries. Of all respondents, 79% mainly work or advocate for the protection of the rights of patients with chronic conditions, not excluding however a focus on rare conditions or on patients without any specific health condition. Among the chronic conditions, the most represented were chronic pain (45%), cardiovascular diseases (39%), rare diseases (37%), diabetes (34%), arthritis or osteoporosis (32%), and so forth. Most of the associations which took part in the survey work on more levels: 84% at the national level, 37% at the local, and, in a smaller percentage, also abroad: international (26%) and European (21%) levels were also present.
The Israeli civil society organization, whose results were used as a main point of reference, works at a national level and deals with patients affected by chronic diseases in the field of reproductive health, pregnancy, and childcare.
Part 2 – Continuity of care during the Covid-19 pandemic
As a first question, respondents were asked to share their experience with the continuity of care during the Covid-19 pandemic. As per their views, patients’ main difficulties during Covid-19 pandemic were, above all, three: getting an appointment with a specialist (84%), communicating with their GPs and specialists for urgent matters (65%), and updating their therapeutic plans (59%). These were followed by communicating regularly with their GPs (57%) and accessing emergency centers (40%). Israel, in these factors, only encountered slight difficulty
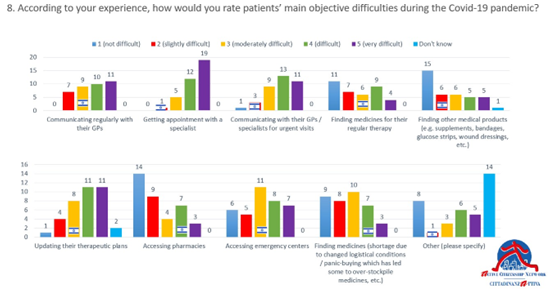
Regarding obtaining medicines for regular therapy, main objective difficulties were linked to: patients not wanting to go to the pharmacy due to Covid-19 risk (46%), an issue also shared by Israel, or, to a lesser extent, due to other health reasons (35%), difficulty of obtaining a prescription (40%), as well as patients hindered by financial reasons (35%). A smaller share stated pharmacies being too busy (24%), or lack of access such as due to unavailability of the medicine at the pharmacy (21%).
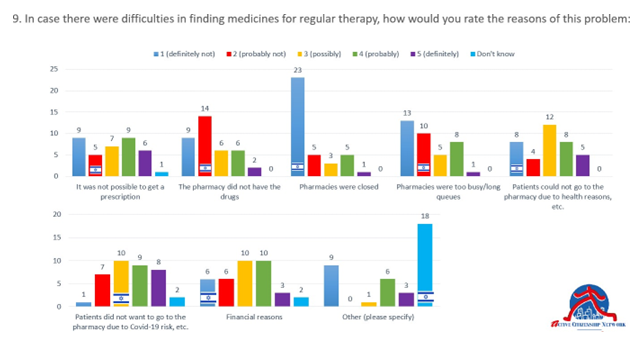
Besides objective difficulties related to the reduced possibility of access to treatment or obtaining medicines, patients’ main worries and concerns during Covid-19 were also taken into consideration by the survey. The biggest concern of patients regarded the impact that Covid-19 could have on their own pathology (78%), immediately followed by the necessity of being hospitalized or receiving a surgical procedure (76%) and the repercussions it might have on their mental well-being and self- care (73%). Not being able to continue their regular treatment, poor access to laboratory/diagnostic testing for their conditions, difficulty to access home care professionals or GPs for their own condition were also highly reported concerns from the patients including Israeli one, with all answers being
“high” and “very high” when asked to rate their concerns.
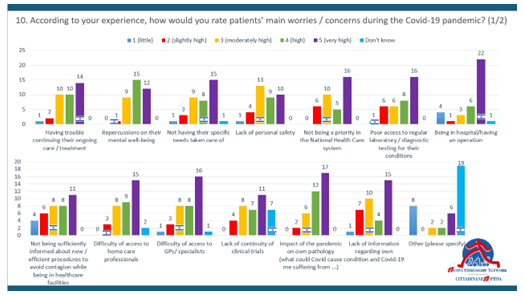
According to more than half of the respondents (51%), the concerns and difficulties mentioned above emerged mostly during the entire pandemic, whereas slightly less of them think it was mostly during the first wave (41%) and much less during the second wave (8%). Moreover, regarding the influence of Covid-19 on therapeutic adherence, while one third thought it could not be generalized, more than half of the respondents (52%) thought that patients are less adherent due to objective (26%) or subjective (26%) reasons.
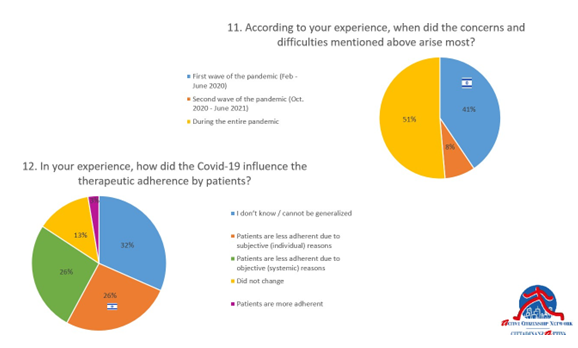
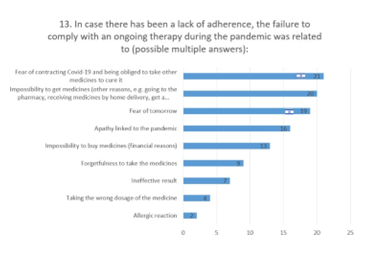
The ACN survey also highlighted how the difficulty in interacting with doctors, especially specialists, has led to an increase in problems related to adherence with therapies already in progress. In these cases of a lack of adherence, the failure to comply with an ongoing therapy was largely related to: fear of contracting Covid-19 and having to take other medicines (58%), impossibility to get medicines not because of financial reasons, but because of not being able to go to the pharmacy or lacking home delivery services (50%), and fear of tomorrow (50%). To a lesser extent financial reasons (34%) and apathy linked with the pandemic (39%) influenced the therapeutic adherence.
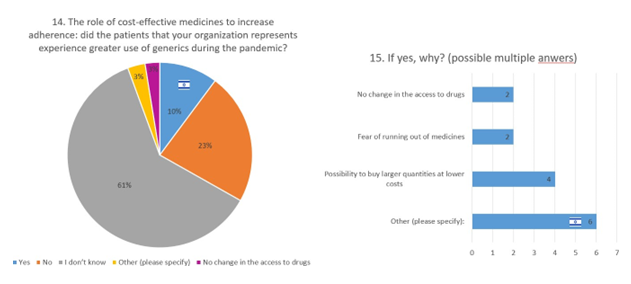
Regarding the use of generic medicines, respondents did not have very specific knowledge on the impact of the Covid-19 pandemic on the use of these medicines. However, of those which knew about the role of cost-effective medicines for therapeutic adherence (10% including Israel), it was noticed that the pandemic did not so much provoke a change in what were the buying habits of patients between branded and unbranded medicines, with 23% of respondents not experiencing a greater use of generics during the pandemic in contrast to 10% who did. Interesting to notice is that, most of the times, the patients’ switch to generics was due to the possibility of buying larger quantities at lower costs. To a lesser extent, reasons were also fear of running out of medicines or no change in the access to medicines.
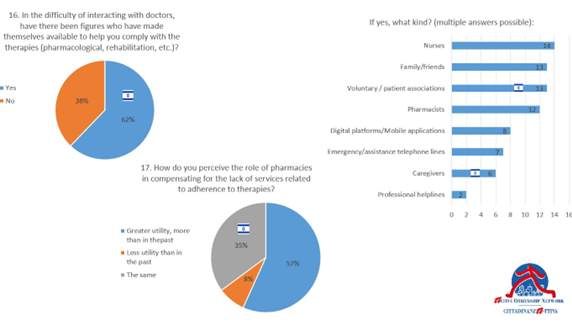
On the topic of difficulty of interacting with doctors, other figures made themselves available to help patients comply with their therapies in 62% of cases, as opposed to a little more than one third who did not think there was anyone else to help them (38%). In this context, the role of pharmacies was praised, with 57% of patients recognizing their greater utility in compensating for the lack of services related to adherence to therapies, compared to the past. 35% of answers claimed the pharmacies’ role remained the same and only 8% thought that pharmacists were of less utility than in the past. For what concerns the presence and availability of other relevant figures, most help was perceived to have been received from nurses (37%), followed by family and friends (34%) and voluntary patient associations (34% including Israel), as well as pharmacists (32%). An interesting data concerns the development and greater use of mobile apps and digital platforms, whose utility was recognized by one fifth of respondents (21%) as a way to fill the gap due to the social distancing measures needed to counteract the increase in infections as much as possible. Lastly, 18% of them felt the help was offered by staff on emergency telephone lines and general caregivers.
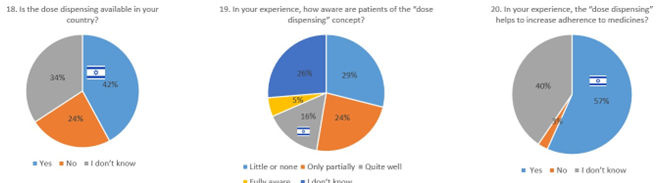
Further in the questionnaire, and related to some available solutions for therapeutic adherence, respondents were asked about the dose dispensing concept and practices. Of all, 42% of respondents declared that dose dispensing was available in their country, as opposed to 24% where it was not available. When asked how aware patients were of the ‘dose dispensing’ concept, most responses highlighted the general lack of awareness of its potential for the benefit of the patient, with 29% of them knowing very little or none of the concept, 26% of them not knowing anything at all, and 24% being only partially aware. Only 5% of patients were fully aware of dose dispensing and 16% knew the concept “quite well”, which is also the category under which the Israelian respondent falls under. When asked of their opinion on whether ‘dose dispensing’ can help to increase adherence to medicines, 57% of respondents answered positively, and only 3% had negative response. A large share (39%) did not have an opinion or knowledge.
Part 3 - Actions and re-actions during the pandemic on continuity of care & therapeutic adherence
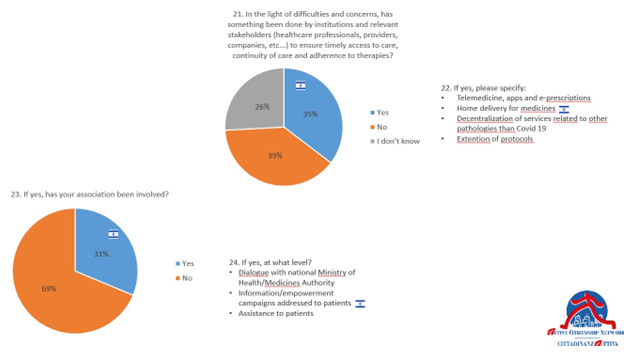
In this section of the survey, respondents were asked to report their experience and knowledge regarding governments’ policies as well as their involvement in the processes. When asked if something has been done by institutions and relevant stakeholders, including healthcare professionals, providers, companies and others to ensure timely access to care, continuity of care and adherence to therapies, 39% of respondents answered negatively, opposed to 35% who confirmed that there were actions taken (Israel included). Those who responded positively specified that the actions taken by institutions and stakeholders regarded primarily: telemedicine, apps and e-prescriptions; home delivery for medicines; decentralization of services related to other pathologies than Covid-19; and extension of therapeutic plans. In this perspective, for instance, the Italian Medicines Agency (AIFA) [15] welcomed and agreed with the proposal launched in March 2020 during the first wave of the pandemic by the Italian Scientific Society of Internal Medicine (FADOI) [16] and Cittadinanzattiva to extend for 3 months the validity of the therapeutic plans created by specialists. Without this decision, 10 million Italian chronic patients would have remained without life-saving medicines. In addition to saving time for doctors involved in emergency management, this measure prevented many patients, especially the elderly, from crowding waiting rooms and clinics [17].
Furthermore, in most cases in which activities have been undertaken, these have been carried out, most of the time, without involving patient associations. This issue was stressed by 69% of respondents. In the few (31%) of cases in which associations were involved, their actions consisted of dialogue with national Ministry of Health/Medicines Authority, information dissemination and empowerment campaigns addressed to patients, and direct assistance to patients
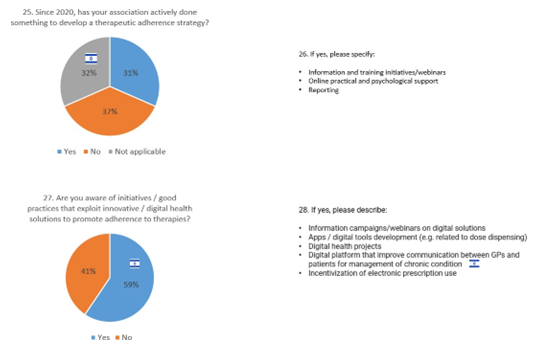
The same share of respondents (31%) has also recognized how their association has actively done something to develop a therapeutic adherence strategy since 2020, mainly referring to initiatives such as information and training initiatives/webinars, online practical and psychological support, and reporting. On the other hand, 37% responded negatively and 32% were not aware of any strategy.
Fortunately, a moderate increase is underlined in the good practices that exploit innovative or digital health solutions to promote adherence to therapies, with 59% of respondents being aware of initiatives involving information campaigns on digital solutions, apps and digital tools development, digital health projects, digital platforms that improve communication between GPs and patients for management of chronic condition, as well as incentivization of e- prescription use.
Part 4 - Patient engagement, therapeutic adherence & the Next Generation EU Fund
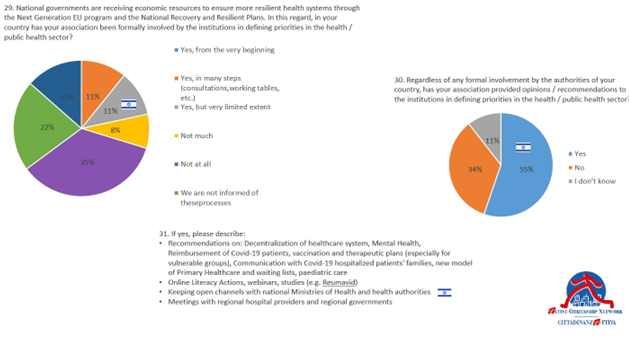
National institutions are receiving a huge number of economic resources to ensure more resilient health systems through the Next Generation EU Fund [18] and thus the National Recovery and Resilience Plan (PNRR). However, from what emerged, in most cases there was no involvement of civic and patient associations by the institutions in defining the priorities of the targets of funding in the public health sector. The majority responded that they were not at all involved (35%) or were not informed of these processes (22%), while 35% responded positively. However, of those who responded positively, it must be noted that only 13% were involved from the very beginning in the process, while 11% were involved with very limited extent and the same share (11%) were involved in many, but not all, of the steps. Interesting to note is that also for Israel’s case, regarding the resources allocated for the management of the health sector, the association was involved to a very limited extent, despite it declared to be one on the few national PAGs involved in activities carried out to ensure timely access to care, continuity of care and adherence to therapies.
Despite this and regardless of any formal involvement by the authorities, more than half of the respondents (55%) confirmed that their association has provided civic recommendations to the institutions in defining priorities in the public health sector, as opposed to 34% who did not. Those who responded affirmatively described the following examples of recommendations provided: decentralization of health system; mental health support; reimbursement of Covid-19 patients; vaccination and therapeutic plans for vulnerable groups in particular; communication with Covid-19 hospitalized patients' families; new models of primary healthcare and management of waiting lists; online health literacy actions; trying to keep open communication channels with national Ministries of Health and other health authorities; and meetings with regional hospital providers and regional governments.
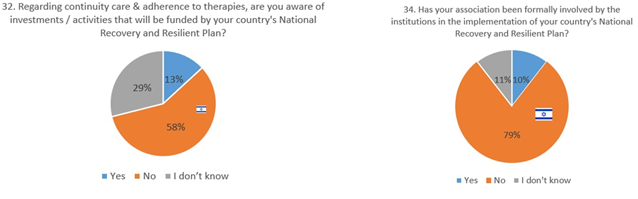
With regard to investments and activities funded by the National Recovery and Resilient Plan on continuity of care and adherence to therapies, these are foreseen only in a minimal percentage and, again, patient associations were only minimally involved. 58% of respondents, including Israel, were not aware of investments and almost one third (29%) did not know anything about this issue.
Opposed to this, only 13% gave positive answer and specified increasing the efficiency, availability, and quality of the healthcare system through more financial resources on infrastructures, employment, and digitalization. To this end, a large majority of respondents (79% including Israel) stated that their organization was not formally involved by the institutions in the implementation of the country’s National Recovery and Resilient Plan, whereas only 10% confirmed their involvement through participation in debates, public consultations, and promotion of new healthcare models.
The data shown above suggest a twofold perspective. On the one hand, they confirm how the NRRP is mainly focused on infrastructural investment and not on operational procedures. On the other, it must also be remembered that, for instance, the NRRP approved in Italy on last April 2021, foresees the realization within 2026 of 1,288 Health Community Houses (Case della Comunità in Italian). According to the Plan, the aim of these Community Houses is to enable them to become a tool for coordinating all the services offered on the territory, with particular reference to chronic disease patients [19]. We are confident that this measure will most likely ensure evident benefits for their caring treatment and the improvement of therapeutic adherence.
Discussion and Conclusion
PAGs have publicly reported, especially during the first wave of the pandemic, an inadequate attention of institutions and the main stakeholders to access and continuity of care for non-Covid- 19 patients.The Covid-19 pandemic has certainly influenced the access and availability of healthcare services and medicines’ access, especially affecting patients with chronic conditions. The lack of access to care has in fact impacted the adherence to regular check-ups as well as therapies taken for management of those chronic conditions.
The key findings from our survey showed that, during the Covid-19 pandemic, patients’ main difficulties concerned the access to specialists’ outpatient visit, communicating with their GPs and specialists for urgent matters, and updating their therapeutic plans. The fear to go to the pharmacy due to Covid-19 risk, difficulty of obtaining a prescription, and financial reasons were the reported barriers to medicines access, exacerbating the adherence dimension of the issue. The survey also highlighted the dramatic impact on the psychological status of these patients that developed fear for a further worsening of their clinical conditions without the possibility to access quality healthcare services.
The negative implications of these disruptive events will be tangible in years with a dramatic spike in chronic disease prevalence increase (due mainly to reduced screenings and missed checkups) as well as morbidity-related adverse events. An increase in excess mortality has already been registered and will probably be more evident in the months to come. Our data also highlighted the need of an enhanced collaboration between patient’s associations and institutions to develop policies and initiatives.
We are aware of the limitations of the survey both from a methodological and statistical perspective, as well as of the value of the production of civic information. The main objective of this article is to highlight the importance of a synergic approach of civic organizations in integrating and complementing the institutional activities that in the emergency context failed to address primary needs of chronic patients. Our preliminary analysis represents a first step to collect and analyze real- world data that could support policy making to improve the access and use of essential medicines and ensure the continuity of care in NCDs patients.
One more point we want to stress is the key role that civic organizations have on the empowerment of patients and their families. through the information services and health literacy initiatives they provide. Empowerment of the patients is critical for adherence to therapies but is, unfortunately, often underestimated. Patients with chronic diseases in particular, not only have to cope with the clinical management of their condition, but also with caring, social, relational, psychological and financial aspects of their disease, factors that often have as much weight as the disease itself on the quality of their lives. The added value of civic organizations consists in a global approach to the patient’s health by offering support, information, education, and training , to help them deal with the many difficulties of their daily lives. This global approach is necessary to make patients strong enough to collaborate with their physicians in personalizing the treatment plan, participating actively in the management of their disease, and using healthcare services more effectively. In the current health emergency context what seems to be urgent is the necessity to balance the needs of Covid-19 patients with those of non-Covid-19 patients, starting from the ones suffering from chronic conditions.
Also fundamental is ensuring high attention to the needs of chronic patients with regard to the direct and indirect opportunities linked to the Next Generation EU Fund and the National Recovery and Resilience Plans (NRRPs). In fact, thanks to the NRRPs, each Member State has a great chance to guarantee more resilient healthcare systems in the coming years. At the same time, it is necessary to encourage a larger involvement of all healthcare stakeholders to co-define key priorities. Looking forward to an increase in research funds to be directly allocated in improving adherence, one of the main follow-ups of the XVI European Patients’ Rights Day (EPRD) [20], also focusing on the health mission within the National Recovery and Resilience Plans across Member States, can hopefully be a greater use of tailored digital health solutions to increase therapeutic adherence for the benefit of chronic patients.

Logo of the 2022 Edition of the European Patients’ Rights Day.
Declarations
Each of the authors confirms that this manuscript has not been previously published by another international peer-review journal and is not under consideration by any other journal. Additionally, all of the authors have approved the contents of this paper and have agreed to the submission policies of the journal.
Authors’ contribution
Each named author has substantially contributed to conducting the underlying research and drafting this manuscript. Additionally, to the best of our knowledge, the named authors have no conflict of interest, financial or otherwise.
Conflict of interest
The authors listed on the first page declare that they do not have any conflict of interest.
Acknowledgements
The EU project “Therapeutic adherence during the COVID-19 pandemic across Europe: impact, experiences and perspectives from PAGs & relevant stakeholders” has been realized by Cittadinanzattiva/Active Citizenship Network with the unconditional support of Viatris. The authors also thank: Franco Maria Pio Mondello Malvestiti, Regional Medical Lead of Viatris, Rome, Italy; Shaantanu Donde, Head – Portfolio Management of Viatris, London, UK; and Alessandro Monaco, International Executive MBA at HEC Paris.
Figures
Fig. 1: Poster realized in occasion of the 12th European Patients’ Rights Day, promoted by Active Citizenship Network, on May 23, 2018, in the European Parliament in Brussels and focused on therapeutic adherence.
Fig. 2: Banner realized in 2018 in occasion of the European communication campaign titled “From Therapeutic Adherence to Therapeutic Alliance”.
Fig. 3: Leaders of patients’ advocacy groups involved by Active Citizenship Network in the 2018 European communication campaign “From Therapeutic Adherence to Therapeutic Alliance”.
Fig. 4: YouTube video realized in 2018 in occasion of the “From Therapeutic Adherence to Therapeutic Alliance” European communication campaign.
Fig. 5: Cover image of the EU civic survey titled “The impact of the Covid-19 pandemic on non- communicable and chronic patients’ therapeutic adherence across Europe” realized by Active Citizenship Network in the second half of 2021.
Fig. 6: Graph representing the responses given to question n.8 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 7: Graph representing the responses given to question n.9 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 8: Graph representing the responses given to question n.10 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 9: Graphs representing the responses given to questions n.11 & 12 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 10: Graph representing the responses given to question n.13 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 11: Graphs representing the responses given to questions n.14 & 15 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 12: Graphs representing the responses given to questions n.16 & 17 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 13: Graphs representing the responses given to questions n.18, 19 & 20 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 14: Graphs representing the responses given to questions n.21, 22 & 23 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 15: Graphs representing the responses given to questions n.25, 26, 27 & 28 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’
therapeutic adherence across Europe”.
Fig. 16: Graphs representing the responses given to questions n.29, 30 & 31 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 17: Graphs representing the responses given to questions n.32 & 34 of ACN’s EU civic survey “The impact of the Covid-19 pandemic on non-communicable and chronic patients’ therapeutic adherence across Europe”.
Fig. 18: Logo of the 2022 Edition of the European Patients’ Rights Day.