International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
*Corresponding Author: Magdi Al Daari, Departement of Public Health, School of Health, shiraz University of Medical Sciences, Yemen Sana.
Received Date: December 25, 2021
Accepted Date: January 03, 2022
Published Date: January 06, 2022
Citation: Magdi Al Daari, Sami Al Haidari, Mohamad Al Amad, (2022) “Epidemiology of Cutaneous Leishmaniasis in Yemen, 2019-2020”. International Journal of Epidemiology and Public Health Research, 2(1). DOI: http;//doi.org/03.2022/1.1026.
Copyright: © 2022 Magdi Al Daari. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: This study aims to describe the pattern, incidence of CL in Yemen and provide recommendations for interventions.
Methods: A descriptive analysis for CL surveillance data that collected by electronic Integrated Diseases Early Warning System during the period from Jan.2019 to Jun 2020. Data included age group for five and ≥ five year, sex, and residency variables. The population of a central statistical organization used to calculate the incidence rate (IR) per 100,000 population.
Results: 6,416 cases of CL reported, 68% were in 2019, 59% were males, 77% were among age group ≥ five years and 37% reported during winter months. The overall incidence rate (IR) was 19.6/100,000 population, significantly higher among under five years than ≥ 5 years (35.8 vs 17.3, P-value <0.001), in males than females (22.6 vs 16.6, P-value <0.001) and in six governorates; Lahj, Al-Jawf, Amran, Dhamar, Sa'adah, Rayma than the rest (17) of Yemeni governorates (45.7 vs 12.3 /100,000, P-value < 0.001).
In conclusion: The high incidence of CL among < 5 years indicates the endemicity of CL in Yemen. Decreasing IR of CL through vector control measures and health education are crucial, including clinical features and age by years instead of age groups to improve surveillance of CL and further analytical study to identify the risk factors for geographical difference are recommended.
Leishmaniasis is a vector-borne disease caused by the genus Leishmania (1) and the disease is divided into three forms: cutaneous leishmaniasis (CL), visceral leishmaniasis (VL), and mucocutaneous leishmaniasis (MCL). Each form is caused by many species.CL is the commonest form while VL is the most severe form and MCL is the most disabling form of the disease. (2, 3) Poverty and malnutrition play a major role in the increased susceptibility to leishmaniasis, the movement of susceptible populations into endemic areas, Children are the most affected than adults in endemic areas, and incomplete therapy of the initial disease is a risk factor for recurrence. Males have an increased incidence of infection, about double those females. (4)
Globally Leishmania first identified in India in 1885 by Cunningham and confirmed its existence in 1903 in Germany by Donovani, Leishman, and Marchand (5)
In 2018, out of 200 countries, Eighty-eight (44%) were endemic for CL and 3 (2%) had previously reported CL cases, and 69 (35%) were endemic for both CL and VL.
Of all the endemic countries, 12 countries considered to be a high burden (>2500 CL cases) since 2014. One country for both (CL&VL). (6) All other endemic countries categorized as having a low burden. (7)
In the Eastern Mediterranean Region (EMR), Leishmaniasis represents a major public health problem. Cutaneous and visceral leishmaniasis mainly seen in 14 of the 22 countries of the region. In EMR, where the reporting system becomes better than before, there was a slightly decreasing trend in CL cases, from a peak of 71,866 cases in 2005 to 46,265 cases in 2018. (6)
In Yemen, cutaneous leishmaniasis is widespread and seems to be endemic. (8) the first reported cases in the country were in Sana’a city. (9) In April–August 2013 the study conducted in the Regional Leishmaniasis Control Center in Central Yemen reported Al Bayda was the most endemic governorate (59.9%), children and adult females most affected people. (5) L. tropica is the common causative agent of CL in Yemen (10)
The true incidence rate of leishmaniasis in Yemen not well reflected, as only a few published documents are available. (11) This aims to describe the epidemiology trend of cutaneous leishmaniasis in Yemen.
We conducted a descriptive analysis for surveillance data of CL. A soft copy of data in excel sheet format was obtained from National Leishmania Control Program in the Ministry of Public Health and Population (MoPHP). Data collected by electronic Integrated Disease Early Warning System eIDEWS during the period from Jan.2019 to Jun 2020, where the standard WHO case definition used:(12)
The data contained the variables of age, sex, address. The data was cleaned and analyzed by an excel program. The population of a central statistical organization (CSO) used to calculate the incidence rate (IR) per 100,000 population. P-value < 0.05 used as a cutoff point for significance.
We used World Health Organization indicators to determine the classification of governorates by cases and incidence rate as follow: (Annex 1)
Ethical approval of data analysis obtained from MoPHP.
The total of reported CL cases from Jan 2019- Jun 2020 were (6416) cases, 68% were in 2019, and (32%) were in the first half of 2020. The highest peak of cases was in Epi Week No, 6, (Figure 1) and the majority of reported cases were from Dhamar governorate (19%). According to gender, males formed 59% of cases, and the age group > five represented 77% of cases. The overall incidence rate was 19.6/100,000. (Table 1) The incidence rate of Cutaneous Leishmaniasis was higher in Lahj governorate 61.7 / 100,000 population, and the lower incidence rate was in Aden, Al Mahra, and Socotra governorates < 1 / 100,000. According to WHO indicators, Lahj governorate was at a medium level for incidence rate indicators. (Figure 2)
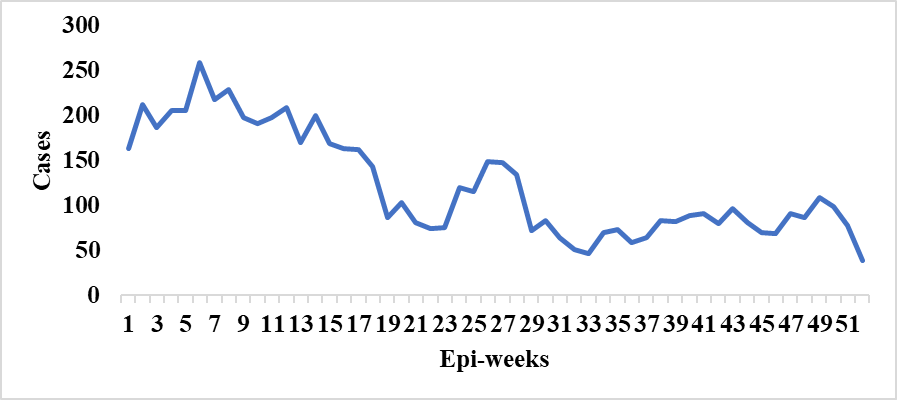
Figure 1: Distribution of Cutaneous Leishmaniasis cases by Epi. weeks, Yemen, Jan 2019- Jun 2020
*half of 2020 cases
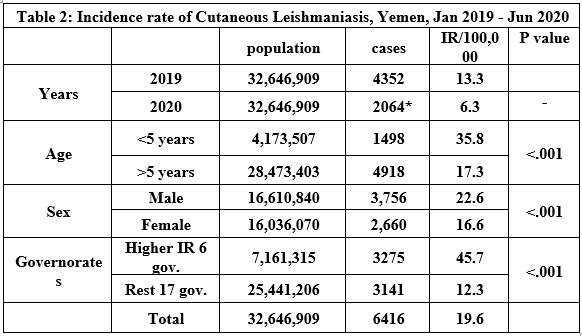
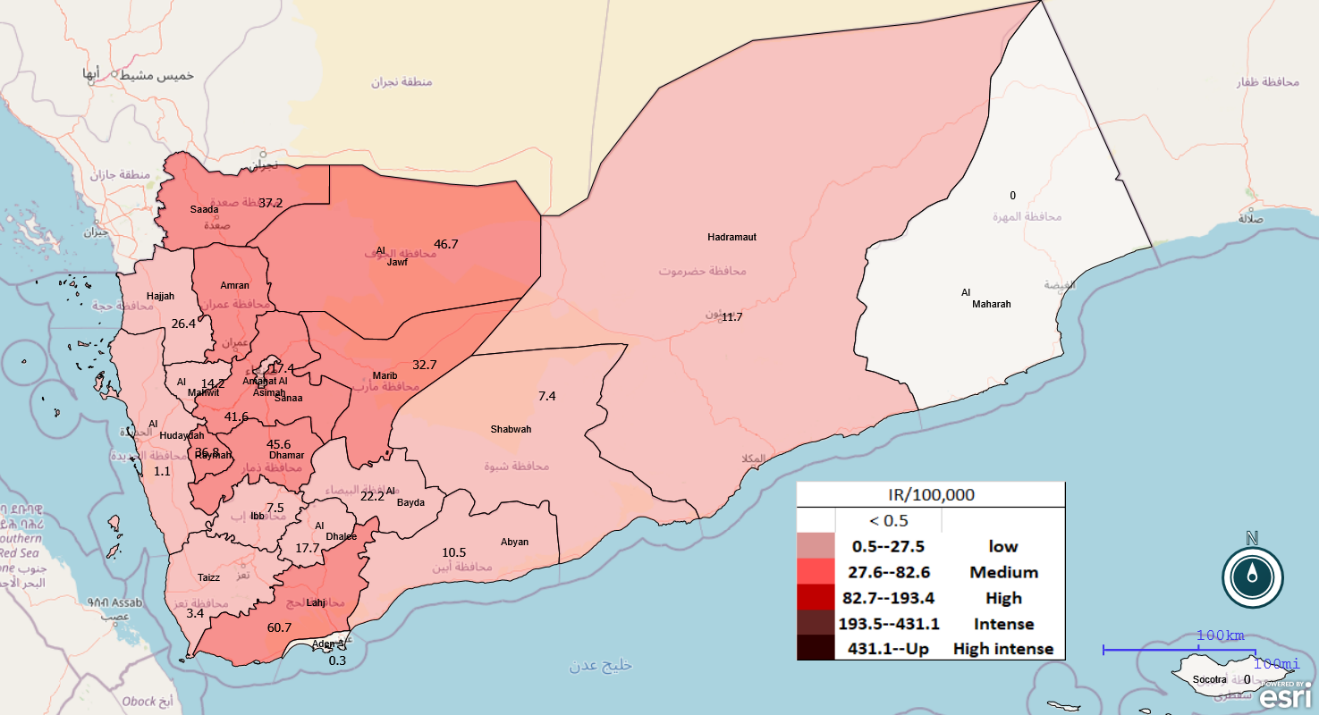
Figure 2: Distribution of Cutaneous Leishmania incidence rate according to WHO indicators, Yemen Jan.2019-Jun2020
Discussion
Cutaneous leishmaniasis is one of the most important infectious diseases in the Eastern Mediterranean Region. (13) It is the most prevalent infectious disease of the skin in Yemen. (5, 14)
In our study, most cases were distributed in mountainous governorates such as Dhamar and Al Amanah governorates, this result agrees with the result of many previous studies conducted in Yemen, (14, 15) and a study conducted in Asir, Saudia Arabia. (16)
The overall incidence rate in our study was 19.6/100,000 slightly higher than a previous study conducted in Yemen during 2013 and a study conducted in Iran that revealed an overall incidence rate of 13/100,000 and 12.6/100,000 respectively. (13, 17) this due to our measured incidence rate to total cases from 2019- the first half of 2020, and population size.
At the level of the governorate, our study showed a higher incidence rate in Lahj governorate (60.7 / 100000) this attributed to the mountainous area and rainy weather, and water barrier, all of this increasing incidence of Leishmaniasis. Compared with 42/100,000 in a previous study conducted in 2013 by the National Leishmania Control Program. (17) These differences due to our measured incidence rate to total cases from 2019- the first half of 2020.
Regarding gender, our findings revealed that males more affected than females. This explained by the males is more involved in outdoor activities, such as, working in the field and sleep sometimes in open places, which exposes them to bite of vectors of leishmaniasis. Other reasons could be the greater exposure of the body surface of men to the vector bites that commonly do not cover their skin as women. (15, 18) This result was similar to studies conducted in the Sharab district Taiz governorate, and western high land of Yemen,(15, 19), and studies conducted in Ethiopia during 2018, and a study conducted in west Iran (13, 20).
According to the age group, our study showed more infection among the age group > 5 years compared to the age group < 5 years old. This due to the most active age group and consume most of their time outdoors. This result agrees with a previous study conducted in the whole of Yemen in 2013 and another study conducted in Hajjah. (17, 21) Many international studies such as the study conducted in west Iran (>20 years) most affected, and in Ethiopia >15 years most affected, another study conducted in Seri Lanka revealed that age group >15 most affected. (13, 20, 22)
Our finding revealed the seasonality of cases with an increase during the winter months. This result agrees with a study conducted in west Iran,(13) and disagreed with a study conducted in Seri Lanka that showed no seasonal variation in some regions of the country. (22) This disagreement might be due to the vectors of Leishmaniasis affected by weather and temperature variation. (23)
Limitation
Only four variables were included in the line list, a long interval of age groups e.g. only two groups < 5 years and ≥5 years and there is no clinical variable in the line list.