International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Melania La Verde 1, Margherita Ferrante 1, Fresta Lucia 1, Chiara Copat 1, Gea Oliveri Conti 1, Salvatore Caruso 2, Agnes Higgins 3, Maria Fiore 1*
1Department of Medical, Surgical and Advanced Technologies "G.F. Ingrassia". University of Catania. Catania. Italy. Via Santa Sofia. 87 – 95123 Catania.
2Department of General Surgery and Medical Surgical Specialties, Obstetric and Gynecological Clinic, "Policlinico G. Rodolico – San Marco". University of Catania. Catania. Italy. Via Santa Sofia. 78 – 95123 Catania.
3School of Nursing and Midwifery, Trinity College, 24 D'Olier Street, Dublin, D02 T283, Ireland
*Corresponding author: Maria Fiore, Department "G.F. Ingrassia". University of Catania. Catania. Italy. Via Santa Sofia. 87, 95123 Catania.
Received: August 23, 2021
Accepted: August 30, 2021
Published: September 18, 2021
Citation: Melania La Verde 1, Ferrante M, Lucia F, Copat C, Gea Oliveri Conti, “The Management of Perinatal Mental Health Problems: Gaps Still Exist Between Theory and Practice”. International Journal of Epidemiology and Public Health Research, 1(3); DOI: http;//doi.org/03.2021/1.1018.
Copyright: © 2021 Maria Fiore. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Perinatal mental disorders (PMDs) affect up to 20% of women. Healthcare professionals’ (HPs) play a key role in the early detection, prevention and treatment of PMDs.
Objective: To investigate: (1) HPs’ knowledge, skills, current practices; (2) availability of services within maternity ones and barriers to access to mental health support; (3) finally HPs’ skills and current practices were compared to women’s experience of care.
Methods: We recruited a total of 54 HPs and 200 women who had recently given birth. Data were collected using two anonymous and self-completed questionnaires; both included a combination of binary (yes/no) and Likert five-point scale questions.
Results: HPs had a lack of knowledge on suicide in the perinatal period (1.94±1.22) and screening tools (1.72±0.86). Comparing women with HPs discrepancies emerged in "provide information on mental health" (women: 9.5%, HP: 31.5%, p = 0.00) and "ask about mental health" (women: 15.5%, HP:55.6%, p=0.00), while both reported low "use mental health screenings" (women:11.5%, HP:16.7%, p=0.36). In addition, during the interview the HPs lacked to ask about suicide thoughts or behaviors (women: 0.5%, HP: 41.5%, p=0.00). Again, unlike mothers, most of them reported to include mental health as a dimension in their clinical practices assessment (21.6% vs 77.8%, p=0.00). Nurses perceived the organizational/structural barriers more than their collegues, no differences were observed for individual/sociocultural barriers.
Conclusions: Due to the high PMDs prevalence, outcomes and costs, their underestimation can be a serious failing in public health. Appropriate training, organizational support and collaborative care may be central for successful screening and management.
1. Introduction
Perinatal mental disorders (PMDs) affect up to 20% of women [1] in addition to be recognized by the World Health Organization as a major public health issue [2]. The focus of research and policy has largely centred on postnatal depression, but PMDs include a wide range of disorders [3]. Moreover, untreated PMDs are associated with severe adverse maternal outcomes including suicide risk [4], obstetric complications [5] and severe mental illness [6] In particular, perinatal suicide is considered one of the leading causes of maternal death [7] and rates may be underestimate [8]. Furthermore, a history of mental illness is predictors of PMD [1] even if the evidence is not consistent with the relapse rate of women with prior depression and bipolar disorder during pregnancy [7].
PMDs also affect offspring outcomes increasing in risks of pre-term birth low birth weight [9], pre-eclampsia [10] and psychopathology in adolescent years even independently of parental lifetime psychopathology [11].
Furthermore, a substantial economic impact is associated with untreated PMD due to its effects on both women and children [12]. The burden of PMDs in low-and-middle-income countries is even higher than high-income countries, due to low levels of detection, inadequate service provision and treatment in resource-constrained settings [13].
In 2014, the National Institute for Health and Care Excellence [14] recommended that a general discussion on mental health and wellbeing take place with all women both at the first contact in pregnancy and in the early postnatal period [1]. Clinical staff in obstetric practices is ideally positioned to detect and manage mental distress, but evidence suggests that midwives and primary care nurses lack knowledge as well as encounter many barriers addressing PMDs issues [15]. As far as we are aware, no studies have been carried out to assess knowledge and skills of gynecologists in perinatal mental health management. In addition, few studies exist that explore women’s experiences of perinatal mental health care and those available identify a need for greater support, information and assessment of mental health and emotional well-being during the perinatal period [16].
To date, the urgent need to prevent perinatal mental disorders increases the interest in studies to tackle existing gaps in its management. Therefore, this study aimed to investigate: (1) healthcare professionals’ knowledge, skills, current practices regarding perinatal mental health; (2) availability of perinatal mental health services within maternity ones and barriers to access to mental health support; (3) finally healthcare professionals’ skills and current practices were compared to women’s experience of care.
2. Materials and Methods
2.1. Study design, setting and participants
This study was based on a hospital survey conducted from January to June 2019. We recruited both healthcare professionals (gynecologists, midwives and nurses, all working in obstetric field) and women that had recently given birth and who were still hospitalized (usually the hospitalization period was 2-3 days).
2.2. Data collection
Data were collected using two anonymous and self-completed questionnaires, one for healthcare professional and one for women that had recently given birth. These questionnaires were based on a questionnaire used in similar studies [15, 17] and adapted with permission by the research team. In particular, we prepared the questionnaires by translating from English into Italian and adapting some of the questions for the women in order to compare their answers with healthcare professional’s ones. Questions not applicable to women were excluded. Regarding the women’s survey, a panel of experts, with backgrounds in psychology, medicine and public health, reviewed the draft of the questionnaire. Then revisions were made based on the expert panel’s comment. Finally, a pilot study with 15 women was carried out to check the understanding of the questions and the answers’ accuracy. Both questionnaires included a combination of binary (yes/no) and Likert five-point scale questions (from 1 “not knowledgeable at all/not skilled at all”, to 5 “very knowledgeable, very skilled”). The questionnaire aimed to healthcare professionals included: demographic data (gender, age at recruitment, marital status, occupation and prior experience working in mental health settings), questions related to knowledge (19 items), skills (35 items), current practices in perinatal mental health (22 items), and perceive barriers (26 items) identified at four levels: individual (e.g, stigma, poor awareness), organizational (e.g. resource inadequacies, service fragmentation), sociocultural (e.g. language/cultural barriers) and structural (e.g. unclear policy) levels (Sambrook Smith et al. 2019). Finally, “current practices” were indagated by the use of two questions. The first question was "In your clinical practice, do you...(possible answers: yes/no)" (Table 4) and the second question was "In your clinical practice do you asks women about ..." (possible answers: never = 0, only to women at risk = 1, to all women = 2) (Table S7).
The questionnaire aimed to women included: demographic data (age at recruitment, marital status and educational status), questions on their current and past mental health, their evaluation on healthcare professionals’ current practices and skills in perinatal mental health.
2.3 Recruitment
Healthcare professionals (gynecologists, nurses and midwives) and women that had recently given birth, aged 18 years or over, were recruited without other exclusion criteria. The study protocol has been approved by the concerning ethical committee (n.121/2018/PO), written informed consent was obtained from all participants. Participating to the study was entirely voluntary without any form of compensation. All participants were provided of a paper copy of the questionnaire. The healthcare professionals filled out the questionnaire during a break and the women filled it while the infant was sleeping. Fifty-four out of the 70 contacted healthcare professionals and 200 out of the 210 women agreed to participate in this investigation (77%, and 95% response rate), respectively. Reasons for refusal were pain or breastfeeding and work-engagement for women and health professionals, respectively.
2.4. Statistical analysis
Descriptive analysis was carried out using frequencies (absolute and relative) and mean ± standard deviation (SD) for qualitative and quantitative (single item score) variables, respectively. We summed the scores regarding to knowledge, skills and barriers to obtain their indexes. The internal consistency of these index variables was estimated using Cronbach’s alpha reliability test. Values of Cronbach’s alpha above 0.70 were considered acceptable, between 0.90 and 0.95 were considered “optimal”, and above 0.95 were interpreted as indicative of “item redundancy” [18].
We used box-plots and contingency tables to visualize the distribution comparison of the indexes belonging to the work experience in mental health (yes/no) and occupation groups (nurses, gynecologists, midwives), respectively. We compared healthcare professionals’ current practices by work experience in mental health and women’s perception using the Chi-square test. Finally, Kruskall-Wallis H test was used to compare healthcare professionals’ knowledge, skills and current practice indexes among the occupation categories and for multiple comparisons we used Bonferroni post hoc test. Statistical analyses were performed using statistical software SPSS for Windows (Statistical Package for the Social Science, version 21.0; SPSS Inc., Chicago, IL, USA). Findings were reported as significant at p<0.05.
3. Results
3.1 Principal characteristics of participants
3.1.1 Healthcare professionals
The healthcare professionals’ characteristics, stratified by occupation, are reported in Table 1.
|
Characteristics |
Total N=54 |
Gynecologists N=14 |
Midwives N=22 |
Nurses N=18 |
|
|
n(%) |
n(%) |
n(%) |
n(%) |
|
Sex |
|
|
|
|
|
Female |
47 (87.0) |
8 (57.1) |
22 (100) |
17 (94.4) |
|
Male |
7 (13.0) |
6 (42.9) |
0 (0) |
1 (5.6) |
|
Median age (IQR*) |
29 (24-44) |
29 (27-30) |
23 (22-32) |
47 (44-50) |
|
Marital status |
|
|
|
|
|
Married |
16 (29.6) |
2 (14.3) |
4 (18.2) |
10 (58.6) |
|
Unmarried/single* |
38 (70.4) |
12(85.7) |
18 (81.8) |
8 (44.4) |
|
Women with PMDs cared for in the last 6 months |
|
|
|
|
|
0 women |
41 (75.9) |
9 (64.3) |
19 (86.4) |
13 (72.2) |
|
1-5 woman |
11 (20.4) |
5 (35.7) |
2 (9.1) |
4 (22.2) |
|
6+ woman |
2 (3.7) |
0 (0) |
1 (4.5) |
1 (5.6) |
|
Work experience in mental health settings (Yes) |
13 (24.1) |
1 (7.1) |
2 (9.1) |
10 (55.6) |
*Single: only two nurseTable 1: Characteristics of healthcare professionals, by occupation.
3.1.2 Women that had recently given birth
A total of 200 women, aged 31±5 years, were recruited for the study. Seventy percent were married, 43% were educated to diploma level and 39% had a university degree. All the women reported not having suffered from mental health problems during pregnancy. Unfortunately, the questionnaire did not include questions regarding women's employment.
3.2 Healthcare professionals’ knowledge, skills, and current practices in perinatal mental health (PMH)
3.2.1 Healthcare professionals’ knowledge of PMH
Healthcare professionals reported an average knowledge on most PMDs topics, being highest in perinatal anxiety (2.89±1.06) and lowest in suicide in the perinatal period (1.94±1.22) and screening tools (1.72±0.86) (Table 2).
|
How would you rate your knowledge (score 1-5) on: |
Mean |
SD* |
|
Perinatal anxiety |
2.89 |
1.06 |
|
Perinatal Depression (antenatal and postnatal) |
2.63 |
0.88 |
|
Impact of maternal mental health on mothering |
2.63 |
1.08 |
|
Risk factor for developing mental health problem in the perinatal period |
2.63 |
1.09 |
|
Eating disorders and pregnancy |
2.63 |
1.19 |
|
Psychotropic drug use during pregnancy and breastfeeding |
2.61 |
1.20 |
|
Post-Traumatic Stress Disorder |
2.59 |
1.17 |
|
Substance misuse in the perinatal period |
2.50 |
1.10 |
|
Alcohol misuse in the perinatal period |
2.46 |
1.08 |
|
Obsessive thinking related to perinatal mental health |
2.39 |
0.94 |
|
Psychosis in the perinatal period |
2.39 |
0.98 |
|
Personality disorders |
2.33 |
1.17 |
|
Impact of maternal mental health on the foetus/baby |
2.31 |
0.82 |
|
Obsessive compulsive or ritualistic behavior |
2.20 |
1.14 |
|
Services available to support women with PMD |
2.19 |
0.91 |
|
Bipolar Disorder |
2.17 |
1.26 |
|
Legal aspect of caring for women experiencing PMD and their babies |
2.11 |
1.06 |
|
Suicide in the perinatal period |
1.94 |
1.22 |
|
Screening tool for PMD |
1.72 |
0.86 |
*SD: standard deviation
Table 2: Healthcare professionals’ self-rated knowledge about perinatal mental health.
The overall knowledge about PMH, rated by the sum of each item in the “knowledge index” (score: min 19 – max 95), had an "optimal" internal consistency (Cronbach's alpha = 0.94). Comparing the overall knowledge about PMH among the three groups of healthcare professionals we didn’t observe significant differences (p=0.57) (Figure 1).
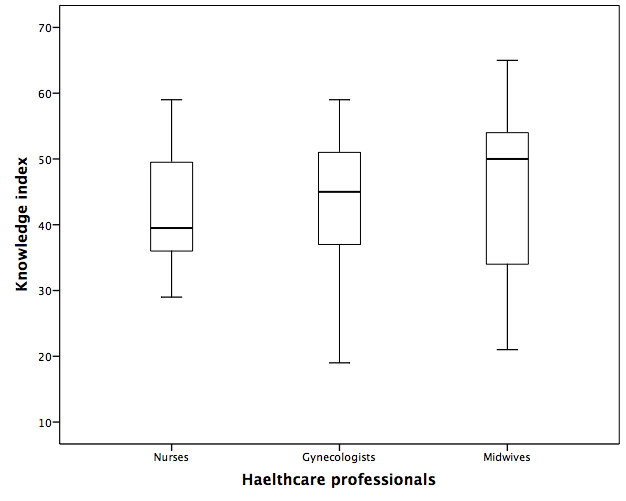
Figure 1: Knowledge index about perinatal mental health, by occupation
3.2.2 Healthcare professionals’ skills in perinatal mental health activities
Table 3 shows healthcare professionals’ self-rated skill indexes in undertaking perinatal mental health activities. In particular, health professionals reported being most skilled in “opening a discussion and asking women about anxiety…” (18.3±6.2) and in “discussing with women the need to consult with and/or refer to…” (16.0±6.5). However, they reported an average score also in the other skills. The answers to the single skill items are reported as Supplementary materials (Tables S1- S6).
We didn’t observe significant differences in the overall healthcare professionals’ skills in undertaking perinatal mental health activities, rated by the sum of each item in the “skills index”, among the healthcare professional groups (nurses, gynecologists, midwives).
|
Skill Indexes |
Mean ± SD |
Cronbach’s alpha* |
|
Skill in opening a discussion and asking to women about: anxiety, mood, alcohol and substance use, eating behaviours, psycosis, suicidal thoughts/behaviours, sexual abuse/ sexual violence, and intimate partner violence. Index score: min 8 - max 40 |
18.3±6.2 |
0.92 |
|
Skill in discussing with women the need to consult with and/or refer to: primary care, mental health services (nurse, psychiatrist, psychologist, counsellor), perinatal mental health services (midwife, psychiatrist, nurse), social worker, child protection services, drug and alcohol services. Index score: min 6 - max 30 |
16.0±6.5 |
0.93 |
|
Skill in developing a plan of care with women who: have thoughts about harming their baby, have thoughts about harming themselves, are experiencing severe anxiety, are experiencing depression, have obsessive thinking, are hearing voices, are having strange or unusual thoughts (delusions). Index score: min 7 - max 35 |
14.9±7.1 |
0.95 |
|
Skill in providing support to partner/family members who are concerned about: the safety of the baby, own mental health, the woman’s safety, the woman’s mental health, impact of maternal mental health problems on foetus/baby. Index score: min 5 - max 25 |
14.3±4.7 |
0.93 |
|
Skill in providing support to women who are: traumatized by their birth experience, concerned about taking psychotropic medication while pregnant or breastfeeding, concerned that they may develop mental health problems, emotionally distressed, concerned about hereditary nature of mental health problems. Index score: min 5 - max 25 |
12.5±4.4 |
0.88 |
|
Skill in asking for advice or assistance on mental health issues from: colleagues, managers, perinatal mental health services and mental health services. Index score: min 4 - max 20 |
11.7±3.4 |
0.85 |
* Values of Cronbach’s alpha above 0.70 were considered acceptable, between 0.90 and 0.95 were considered “optimal”, and above 0.95 were interpreted as indicative of “item redundancy”.
3.2.3 Perinatal mental healthcare professionals’ current practices
Tables 3: Healthcare professionals’ self-rated skills in undertaking perinatal mental health activities.
Results on perinatal mental healthcare professionals’ current practices are reported in Table 4 and as Supplementary materials (Table S7). The majority of healthcare professionals (77.8%) reported that they include mental health as a dimension of the assessment in their clinical practice. Only, 16.7% reported to make use of mental health tools in their clinical practice. Comparing the healthcare professionals by work experience in mental health we found a significant difference (p=0.05) in “identifying women at risk of PMDs” (30.8% vs 65.9%) (Table 4)
|
|
Total n(%) Yes identify |
Work experience in MH* |
p-value |
|
|
Yes N=13 n(%) |
No N=41 n(%) |
|||
|
Include mental health as a dimension of the assessment you complete with women |
42 (77.8) |
12 (92.3) |
30 (73.2) |
0.254 |
|
Identifies women’s protection/ defense strategies for maintaining mental health |
35 (64.8) |
8 (61.5) |
27 (65.9) |
1.000 |
|
Discuss women’s concerns about psychopharmacology during pregnancy and/or breastfeeding |
33 (61.1) |
8 (61.5) |
25 (61.0) |
1.000 |
|
Identify women at risk of PMDs |
31 (57.4) |
4 (30.8) |
27 (65.9) |
0.051 |
|
Ask women about their mental health past history/diagnosis |
30 (55.6) |
9 (69.2) |
21 (51.2) |
0.343 |
|
Refer women with PMDs to child protection services |
29 (53.7) |
7 (53.8) |
22 (53.7) |
1.000 |
|
Develop a care plan with women who have a pre-existing mental health diagnosis |
19 (35.2) |
4 (30.8) |
15 (36.6) |
1.000 |
|
Provide information about PMDs to women’s partners/family |
17 (31.5) |
4 (30.8) |
13 (31.7) |
1.000 |
|
Discuss the nature of PMDs with women |
16 (29.6) |
5 (38.5) |
11 (26.8) |
0.493 |
|
Use mental health tools to screen for or assess mental health problems |
9 (16.7) |
2 (15.4) |
7 (17.1) |
1.000 |
*MH: mental healtTable 4: In your clinical practice, do you:
Regarding the question "In your clinical practice do you asks women about..." (possible answers: never = 0, only to women at risk = 1, to all women = 2 "), a number of key issues were not asked to women, for example more than 50% of all professionals did not ask about “past trauma, grief or loss experiences”, “experience of mood disorders”, “experience of intimate partner violence”, “usual mental health coping strategies”, “suicidal thoughts or behaviors” (Supplementary materials Table S7).
Besides we calculated two current practice indexes, each adding the items of the following questions: (1) "In your clinical practice, do you..." and (2) "In your clinical practice do you asks women about...", respectively. Then, comparing their median values among the healthcare professional groups we observed significant differences (Figure 2A and Figure 2B). In particular, a Kruskal-Wallis H test showed that there was a significant difference in current clinical practices made (question 1) between the healthcare professionals, χ2(2) = 10.858, p = 0.004, with a mean rank current practices score of 23.17 for nurses, 20.04 for gynecologists and 35.80 for midwives. Post hoc tests using Bonferroni correction revealed that midwives had higher current practices score than nurses (p = 0.032) and gynecologists (p = 0.009) (Figure 2A). We observed significant differences also in the current practice to ask women about … (question 2) between the healthcare professionals, χ2(2) = 6.296, p = 0.043, with a mean rank current practices score of 25.92 for nurses, 20.25 for gynecologists and 33.41 for midwives. Post hoc tests using Bonferroni correction revealed that midwives had significant higher current practices score than gynecologists (p = 0.042) (Figure 2B).
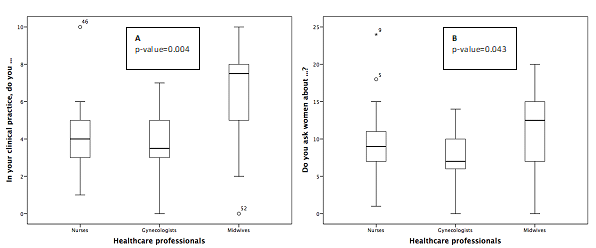
Figure 2: Healthcare professionals’ current practices indexes, by occupation (nurses, gynecologists, midwives).
3.3 Perinatal mental health services and barriers
Overall, the availability of services, policies and education in relation to perinatal mental health was reported to be low by the healthcare professionals. Only 13.0% reported to have a designated place in women’s medical records to document a mental health plan of care for women and 18.5% reported the presence of in-service education in the field of mental health (Supplementary materials Table S8).
Healthcare professionals were also asked to rate a series of topics that could be considered as barriers to quality perinatal mental health care. The barriers rated most were “organizational” issues such as “heavy workload” (35.2%), “time allocated too short” (35.2%), “not seeing regularly to build relationship” (33.3%), “perinatal mental health services not available” (33.3%), “lacks knowledge of how to access mental health services” (31.5%). Among “individual/sociocultural” barriers the “lack of knowledge on perinatal mental health and women from different culture” had the highest score (37.0%) followed by the “lack of knowledge on perinatal mental health” (31.5%), (Supplementary materials Table S9).
A Kruskal-Wallis H test showed that there was a statistically significant difference in perceived organizational/structural barriers score between the healthcare professionals, χ2(2) = 5.964, p = 0.05, with a mean rank organizational/structural barriers score of 34.33 for nurses, 27.11 for gynecologists and 22.16 for midwives. Post hoc tests using Bonferroni correction revealed that nurses perceived higher organizational/structural barriers than midwives (p = 0.048) (Figure 3A). Conversely, we did not observe difference in perceived individual/sociocultural barriers score between the healthcare professionals, χ2(2) = 0.688, p = 0.709, with a mean rank individual/sociocultural barriers score of 25.58 for nurses, 30.21 for gynecologists and 27.34 for midwives (Figure 3B).
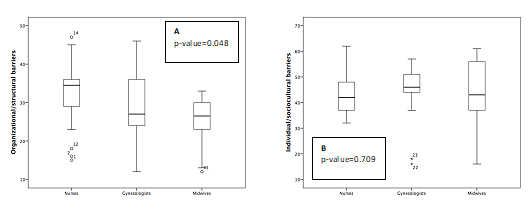
Figure 3: Organizational/structural (A) and Individual/Sociocultural (B) barriers to discussing mental health with women, by occupation (nurses, gynecologists, midwives).
3.4. Women’s perception of PMDs issues management compared to healthcare professional answers.
Women, unlike healthcare professionals, reported that most health professionals did not include mental health as a dimension of the assessment, especially as regards perinatal mental health (Tables 5).
|
|
Women |
Healthcare professionals |
p-value* |
|
|
n (%) |
n (%) |
|
|
Discuss your concerns about psychopharmacology during pregnancy and/or breastfeeding? |
44 (22.0) |
33 (61.2) |
0.00 |
|
Include mental health as a dimension of the assessment? |
43 (21.6) |
42 (77.8) |
0.00 |
|
Ask you about your mental health (past history/diagnosis)? |
31 (15.5) |
30 (55.6) |
0.00 |
|
Use mental health tools to screen for or assess mental health problems? |
23 (11.5) |
9 (16.7) |
0.36 |
|
Discuss the nature of PMD’s with you? |
19 (9.5) |
16 (29.6) |
0.00 |
|
Provide information about PMD’s to you and your partner/family? |
19 (9.5) |
17 (31.5) |
0.00 |
*Chi-square test
Table 5: During your interview, do healthcare professionals:
From the comparison between the women’s answers, about what healthcare professionals ask to them during the interview, and the healthcare professionals’ ones differences emerged regarding every issues (Table 6).
|
|
Women |
Healthcare professionals |
p-value |
|
|
n (%) |
n (%) |
|
|
Past or current alcohol use |
119 (59.5) |
48 (90.6) |
0.00 |
|
Past or current substance use |
117 (58.5) |
45 (84.9) |
0.00 |
|
Experience of eating disorders |
39 (19.5) |
39 (73.6) |
0.00 |
|
Experience of anxiety, panic, OCD* |
36 (18.2) |
46 (86.8) |
0.00 |
|
Past trauma, grief or loss experiences |
30 (15.0) |
31 (58.5) |
0.00 |
|
Psychological support available to them |
26 (13.0) |
33 (62.3) |
0.00 |
|
Experience of psychosis |
11 (5.5) |
32 (60.4) |
0.00 |
|
Experience of intimate partner violence |
4 (2.0) |
23 (43.4) |
0.00 |
|
Experience of sexual abuse/violence |
3 (1.5) |
27 (50.9) |
0.00 |
|
Suicidal thoughts or behaviours |
1 (0.5) |
22 (41.5) |
0.00 |
*Obsessive-compulsive disorder.
Table 6: During your interview, do healthcare professionals ask you about:
Women rated healthcare professionals’ skill in asking them about a number of issues giving a very poor mean score (less than 1.5) in asking women about alcohol and substance use, mood, anxiety, eating behaviors, psychosis, suicidal thoughts, intimate partner violence and sexual abuse/ sexual violence (Supplementary materials Table S10). Conversely, they rated professionals as having better skills in providing support to women who are concerned regarding the safety of the child (3.55±1.39), and their owns safety (2.81±1.45). However, healthcare professionals’ skill in providing support to partner/family in relation to their mental health was not rated as high (1.93±1.45) (Supplementary materials Table S11).
4. Discussion
This is the first Italian survey on the perinatal mental health management both from HPs' and women’s who gave birth perspective. The main findings of our survey lay in lacks both in knowledge, skills and current practices of some perinatal mental health issues (suicide, ask/discuss about mental health, screening tools), in the low case-load of women with PMDs in the last six months reported by HPs, as well as in the discrepancies between the reported opinions of women compared to HPs ones.
The HPs, without differences among the categories, perceived their knowledge and skills on perinatal suicide little close to average. These results need to be improved because perinatal depression and anxiety represent a major risk factor for suicide, but despite growing attention to this field very little is known about suicide, that is considered one of the leading causes of maternal death [7, 4]. Moreover, in our survey 53.8% of HPs reported never asking women if they have any suicidal thoughts or behavior. In many societies suicide is an extremely controversial topic and this is particularly true in perinatal period that it is supposed to be one of the most joyful times in a woman’s life [8, 19, 20]. Our results could reflect this situation but detection of suicidal ideation among pregnant women should be a priority. Few studies have investigated knowledge, skills and current practices of midwives and nurses in perinatal mental health management and as far as we are aware, no data about gynecologists are available [15, 21-23]. In particular, these studies show that midwife reported lower scores than ours in self-rated knowledge and skills about PMDs, especially compared to their knowledge in other professional tasks, even if they have more awareness of depression and anxiety [15, 22, 23]. These differences could be attributed to the non-homogeneity of the studies, as well as to the different training / education of the recruited health professionals.
We also found both an inadequate knowledge and use of mental health tools to screen for or assess PMDs. This result is in line with past research, which has recognized that HPs may not utilize screening tools because of time constraints, lack of training, and lack of knowledge of diagnostic criteria [24]. The lack of routine mental health screening is a main barrier to early identification of PMD’s 25, although universal screening of pregnant and postpartum women for depression is now recommended by numerous professional organizations [26-28] and many states legally mandate perinatal depression screening [28-30]. Reinforcing the findings from other studies, we also found that HPs reported they were not adequately prepared for the use of screening and diagnosis tools in their clinical practice and they rated their knowledge and skills in this field as very low. A number of mental health screening questionnaires have been created over the last two decades, most of them developed to detect depression, but PMDs include a wide range of disorders that need to be addressed [25]. While screening alone is not enough to improve perinatal outcomes [31], different studies reported that the majority of women identified screening as beneficial and reported that it made them feel that their provider cared [32-35].
Moreover, we found that midwives' current practice indexes (referring to the following questions: (1) "In your clinical practice, do you..." and (2) "In your clinical practice do you asks women about...") had higher scores than nurses and gynecologists. It could be due to a greater focus of obstetric training courses on issues related to perinatal mental health of women, as well as a more confidential relationship between midwife and woman than other health professionals, more often males, which allows them to discuss such complex and delicate topics.
The low caseload of women with PMDs in the last six months reported by HPs may be an underestimate of women experiencing PMDs considering that about one in five women will experience a perinatal mental health problem [14]. Likewise, all the women in our survey declaring they did not suffer from any mental disorders during pregnancy might be related to the stigma of being considered an incompetent mother, the shame for guilt for not feeling happy [36-39] and the pressure to be ‘good mothers’ [40]. A meta-synthesis highlighted that women may not understand the significance of their symptoms [40] and another recent study reported women not knowing what were ‘normal’ or ‘abnormal’ emotions in pregnancy and the postnatal period [41].
This survey also indicates the need to fill the widespread deficiencies reported by HPs regarding services, first of all to "designed place in women's medical records to document a mental health plan of care for women" and "in-service education on mental health issues". Such deficiencies, in fact, have been shown to impact the practices of HPs [42-44].
Previous studies identified barriers at four levels: individual (e.g, stigma, poor awareness), organizational (e.g. resource inadequacies, service fragmentation), sociocultural (e.g. language/cultural barriers) and structural (e.g. unclear policy) levels [39]. Consistent with previous findings [17] in our study the barriers rated with highest scores were organizational barriers such as lack of perinatal mental health services, absence of care pathways, heavy workload, lack of time, lack of privacy and not seeing women regularly enough to build a relationship.
Finally, our survey highlighted discrepancies between women’s and HPs’ opinions on “ask about mental health”, infact in contrast to the HPs the maiority of women’s reported that they were not asked. A national survey in UK showed that most women recalled being asked about their mental health in pregnancy (82 %) and in the postnatal period (90 %) [45]. Nagle et al. found that all women were asked about their mental health at least once in the most recent pregnancy, mainly by a midwife at the antenatal booking visit [41]. On the other hand, Redshaw et al. found that non-white women and those living in deprived areas are less likely to be asked about mental health [45]. Our results about discussing on psychopharmacology during pregnancy and/or breastfeeding and on past history/diagnosis conflict with previous study which reported that women who disclosed a history of mental health problems were asked about their mental health more frequently[41]. But sadly, our findings highlighted women's reluctance to disclose about their mental health. In addition, they declared to not suffer from any mental disorders during pregnancy and this raises further suspicion because health professionals’ answers did not confirm these statements. Differently with literature [46,47] our results showed that substance and alcohol use during pregnancy were addressed by healthcare professionals, although not all women confirm this. On the other hand, accordingly to literature [41], we found that the percentage of women who declared to have been interviewed on issues relating to more delicate items/less common disorders such as psychosis, eating disorders, personality disorders or Post Traumatic Stress Disorders and suicidal thoughts was lower than “alcohol and substance use”. Finally, one of the most neglected item was ”experience of intimate partner violence”, which is of concern as previous studies showed that intimate partner violence frequently escalates during pregnancy [31, 48].
5. Study limitation and strengths
This study had some limitations, which must be acknowledged. First, it was based on a survey design therefore respondents might not feel encouraged to provide accurate, honest answers. For example, there is no way of knowing if the self-reported practices by HPs actually reflected clinical practices and how much social desirability impacted the findings. However the inclusion of the women helps towards triangulation of data. Second, despite the high response rate of healthcare professionals, our sample size was small. But nevertheless, we chose to conduct a single-center survey to study a homogeneous sample. Third, we lacked information about HPs’ type and duration of work experience in perinatal mental health settings. It was beyond the scope of this study to address these questions, but it may be a suggestion for future study.
6. Conclusions
Our findings may have important implications not only for the setting in which the survey took place. It was clear that good knowledge, skills and current clinical practices represent a key role in the prevention of PMDs. Based on these findings, the promotion of appropriate training and education on identifying and managing PMD’s, organizational support and investment into perinatal mental health services with clear protocols and standards of care are recommended. Also, it should be improve the knowledge on the adequate use of screening tool for PMDs, which will be helpful to identify women suffering from PMDs. Finally, it is appropriate to provide for a designed place in women’s medical records to document a mental health plan of care for women