International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Sheeehama J 1*, Shivute Justina 2, Haufiku D 3
1UNAM School of Medicine,
2MoHSS Namibia,
3UNAM School of Public Health
*Corresponding authors: Jacob Angara Sheehama, School of Medicine Windhoek Khomas, University of Namibia, Namibia.
Received: March 26, 2021
Accepted: April 02, 2021
Published: April 04, 2021
Citation: Sheeehama J, Justina S, Haufiku D “The Increase Sexually Transmitted Infections Among the Youth Treated at Ongwediva Health Centre, Oshana Region, Namibia”. International Journal of Epidemiology and Public Health Research, 1(2); DOI: http;//doi.org/03.2021/1.1006.
Copyright: © 2021 Jacob A Sheehama. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction: Sexually Transmitted Infections (STIs) also known as Sexually Transmitted Diseases (STDs) which in recent years are more diagnosed among the youth (Cooper, 2010). We do not know what the factors are contributing to the increase of STIs among the youth treated for STIs at Ongwediva Health Centre. This study aimed to identify the contributing factors to the increase of STIs among the youth. Investigate the factors contributing to the increase of STIs among the youth treated for STIs at Ongwediva HC. Analyse the economic and social factors that contribute to the increase of STIs among the youth treated at Ongwediva HC. Identify the strategies implemented by Ongwediva HC to reduce the increase of STIs within their health centre catchment area.
Methods: The research instrument for data collection was done through quantitative method followed the triangulation of questionnaire as a tool. The information gathered were analysed using the SPSS data analysis software. A total number of 30 youth seeking health services on STIs have participated and completed a self-administered questionnaire.
Results: The results of the study show that all 30 respondents were sexual active and 24 (80%) were currently in relationships. Only 17(57%) of the respondents used condom always, 10 (33%) used condom at some points while 3 (10%) had never used a condom. The study finding indicates that 80% of the respondents are sharing toilets either with their family members or with other tenants. Out of 18 male respondents only 7 (39%) that are circumcised, 11 (61%) of the male respondents are not circumcised. Less than half of the respondents 40% of had sex under the influence of alcohol and 10% had sex in order to get something.
Conclusion and recommendations: Active health promotion regarding the benefit of male circumcision and condom use should be made a priority and youth programmes should take cognisance of the issues uncovered in this study and ensure that they are addressed. Youth programme should also address the issues identified in this study such us: having multiple sexual partners, having sex under the influence of alcohol, as well as having sex in order to get something.
Introduction
Sexually Transmitted Infections (STIs) also known as Sexually Transmitted Diseases (STDs) in recent years have been increasingly diagnosed among the youth (Cooper, 2010). STIs are infections that spread through sexual contacts, including vaginal, anal or oral sex but some of them can also be transmitted through non-sexual methods such as via transfusion of blood or blood products. These STIs include HIV, Syphilis, and Trichnomoniasis. These STIs have a range of signs and symptoms or some cases are asymptomatic (Lewis, 2011). That’s why they may go unnoticed until complications occur or a patient is diagnosed. Signs and symptoms may appear few days after the exposure or it may take years before someone notices that they have a problem, it depends on the organisms (Lewis, 2011). Due to the fact that the correlation between the spread of conventional STIs and HIV transmission is so strong, the presence of HIV has changed and increased the importance of STI control. High transmissions of HIV is continued for example with cases of ulcerative STIs, where the broken skin continuity creates an easy port of entry for the HIV virus and other infections. The causes of STIs have also been affected by the presence of HIV, causing for instance an emergence of viral STIs such as herpes simplex to increase, due to immune suppression (Iipinge & Pretorius, 2012). Background, STIs are a significant cause of morbidity among the youth with multiple of consequences and some increase the risk of HIV transmission, STIs caused death through AIDs, cervical cancer, infertility, congenital syphilis and ectopic pregnancy (Lewis, 2011). STIs are on the increase and are some the most rapidly spread infections globally. Therefore surveillance of infections such as STIs is a strategy that is considered important for prevention of the spread, especially among the high risk group (Cooper, 2010). According to UNAIDS (2017) 190 000 people from the age of 15 and above in Namibia are living with HIV. In 2005 Human Immuno-deficiency Virus/Acquired Immuno- Deficiency Syndrome was the leading cause of death in the country (IHME, 2018). In the past it has been proven that good STI control can reduce HIV transmission in situation with cases whereby bacterial STIs are high and the HIV epidemic on the rise (Jooste, 2010). Studies by Jooste made in South Africa suggest that a large number of symptomatic patient with STIs report high risk of sexual behaviour and they are often unrecognised.
Method
In this study a quantitative approach with a descriptive research designs was used to collect the data. No manipulation of variables was possible; instead any determined differences was ex post facto in nature in that way they stem from differences in result in the measurement efforts according to gender and self-directed learning readiness scores (Burns et al,.2015). Quantitative data was collected using closed-ended questionnaires. Questionnaires are good way to obtain information from a large number of people, they may not have time to attend to an interview or take part in experiments. Questionnaires enable respondents to take their time, think about it and come back to the questionnaire later. Respondents can state their view or feeling privately without worrying about the possible reactions of the researcher. In the content of this study the number of respondents in the station was set to a total number of 30 youth that were treated for STIs at the health centre. Population of youth seeking health services at Ongwediva health centre is about 600 per month according the facility records. The number selected were 30 respondents according to Yamane’s formula of calculating sample size, because the potential number of participants in this study is much more and it was not practically to include everybody. A non-probability, purposive sampling technique was conducted as a method of selecting the sample. Non-probability sampling implies that not every element of the population has an opportunity to be included in the sample. This technique was applicable to this study because a selective population from the youth treated at Ongwediva HC was taken. N = 30
Results
The study sample consisted 30 correspondents all of whom 30 filled the questionnaires. Tables, pie charts and bar graphs were used to present the result in a meaningful way and for easy interpretations. During data collection process the most (50%) participants were of age 25 and above filled the questionnaires. Tables, pie charts and bar graphs were used to present the results in a meaningful way and for easy interpretations. During data collection process the most participants were of age 25 and above which made up 50% of the total number of participants (Table 1). The study was not limited to any age group.
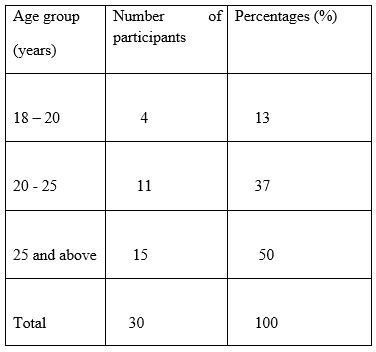
Table 1: Age of respondents/participants
Table 1. Age of respondents/participants in which 18 (60%) were male and 12 (40%) were female (Figure 1). In terms of family context 18 (60%) respondents live alone, 7 (23%) live with their parents and 5 (17%) live with a friend; no one is living with another relative. Respondent’s marital status were as follow: 6 (20%) were single and 24 (80%) were currently in relationships. In terms of employment status 8 (33.3%) were students, 12 (40%) were employed, 1 (3.3%) were self-employed while 7 (23%) were unemployed. The number of male respondents were higher than the female ones, most of the male respondents came to the health centre with referral cards from their partners who were treated before for STIs at some other health centre or at Ongwediva health centre.
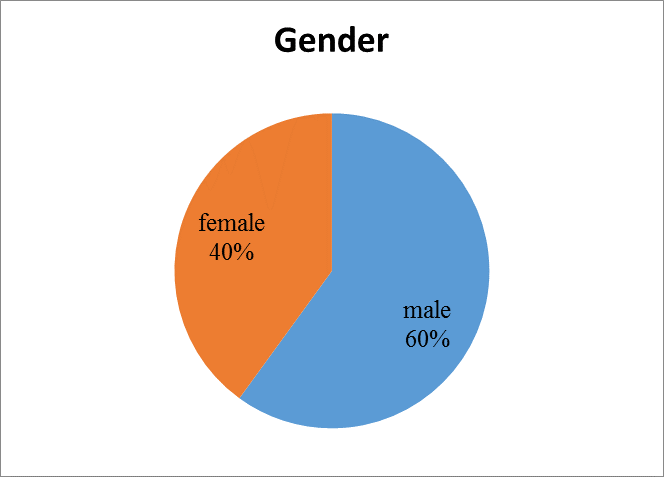
Figure 1: Respondents’ gender (N=30)
Most respondents were employed with a number of 12 participants making up 40% , followed by Students which made up 33.3%, 23.3% are unemployed and 3.3% were self-employed. In terms of family context 60% of the respondents were living alone, 23% were living with their parents while 17% of the respondents were living with a friend and no one was living with another relative (Figure 2).
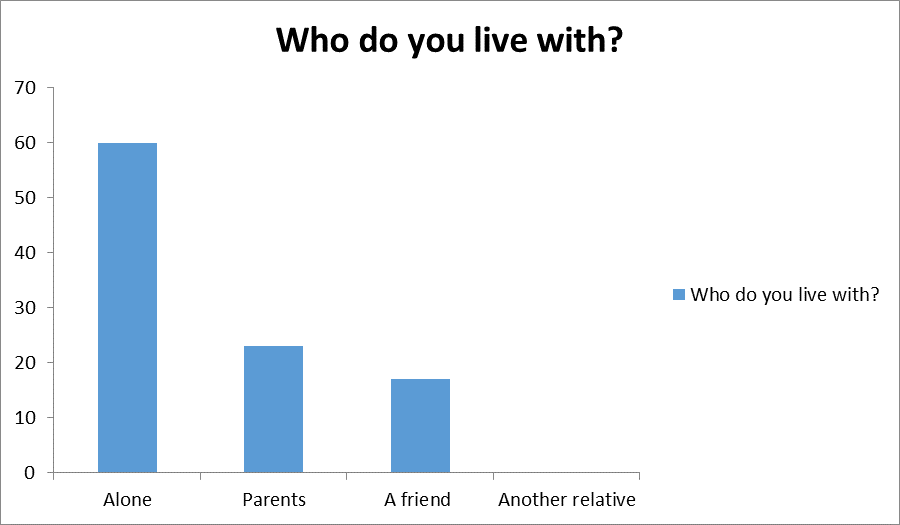
Figure 2: Respondents family context
All 30 respondents are sexually active, where 21 (70%) respondents had only one sexual partner and 5 (17%) had multiple partners, while 4 (13%) respondents don’t have sexual partners at the moment of data collection. Overall of 27 (90%) youth used a condom, 3 (10%) never used a condom and 10 (33%) used condom at some point only. About 60 % of the respondents were sharing the toilets with other tenants, 6 (20%) sharing the toilets with their family members and only 20% were using their own toilets. The study showed that 20% of the respondents were sharing toilets with their family members while 60% were sharing a toilet with other tenants, which made up 80% of the population that were sharing toilets and only 20% of the population were using their own toilets. Out of 18 male respondents only 7 that were circumcised. About 11 of them were not circumcised made up 61%. Twenty seven (27%) of those that are not circumcised stated that it is against their religion to be circumcised, 18% stated that their partners does not approve circumcision while a large number of 6 (55%) stated that they don’t see the need to be circumcised. A good number of 21 respondents had only one sexual partner which makes up 70%, 5 (17%) had multiple sexual partners, while 4(13%) were not having any sexual partners (Figure 3).
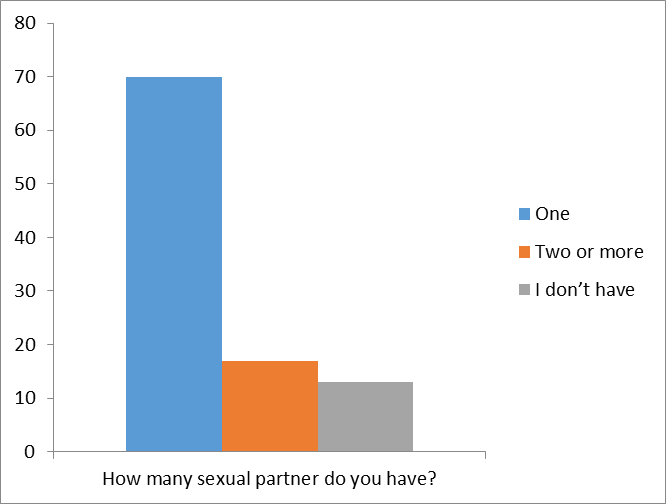
Figure 3: Respondents number of their sexual partners
Although all 30 respondents are sexual active only 17 (57%) who used a condom always, 10(33%) of the respondents used a condom at some points/sometimes, while 3(10%) of the respondent had never used a condom. A good number of 29 (97%) had tested for HIV and 25 (83%) knew their partner status. 40% of the respondents had sex under the influence of alcohol, while 3 (10%) had sex in order to get something either money or gifts. Out of 18 male respondents only 7 (39%) were circumcised, the high number of 11 (61%) are not circumcised in which 3 (27%) of respondents stated that it is against their religion to be circumcised, 6 (55%) of the respondents don’t see the need to be circumcised and 2 (18%) stated that their partners does not approve them to be circumcised.
Discussion and conclusion.
In the study, most respondents had heard about STIs before, but it seems like they don’t know the factors that contribute the increase of STIs. In addition most male respondents had a low knowledge regarding male circumcision as a strategy to prevent HIV and other STIs. A survey done in sub-Saharan Africa, shows that the male circumcisions reduce the female to male transmission of STIs (Williams, Lloyd-smith, Gouws, Hankins, Gets &Hargrove, 2010). In Namibia male circumcision programme was initiated in 2014 and is still implemented in all region of the country. All participants had been sexual active were 80% were in relationships and only 57% used condoms at all times. 80% of the respondents are sharing toilets either with their family members or other tenants. This may partly explain why the prevalence of STIs among the youth treated at Ongwediva HC is high as sharing of toilets is a significant contributing factor to the spread of STIs.
This study has shown that most of females get STIs from the toilet seat compared to males, most males get STIs from unprotected sex. Sexual intercourse for money or gifts was reportedly widespread among the youth; one would have thought it to the practice as youth seek financial gains from their partners, because of poor socioeconomic conditions. Having multiple sexual partners and practicing unsafe sex leads to the increased risk of contracting HIV and Other STIs.