Ebehiwele Ebhohon1*, Olumuyiwa A Ogundipe2, Chineye B Amuchi3, Ikponmwosa Enofe4, Fidelis C Okoli5, Mohamed Abdallah6, Gbeminiyi Samuel7, Adeyinka C Adejumo8
1Department of Gastroenterology and Hepatology, University of Maryland Medical Center, MD, USA.
2Applied Clinical Research Program, St. Cloud State University Minnesota, St. Cloud, USA.
3Boston University School of Public Health, Boston, USA.
4Department of Gastroenterology, Loyola University of Medical Center, Maywood, USA.
5New York University Long Island School of Medicine, New York University Langone Hospital, Long Island, USA.
6Division of Gastroenterology and Hepatology, University of Minnesota, Minneapolis, USA.
7Premier Gastroenterology Specialists, Upper Valley Medical Center, Troy, USA.
8Division of Gastroenterology, Hepatology, and Nutrition, University of Pittsburgh, Pittsburgh, USA.
*Corresponding author: Ebehiwele Ebhohon, Department of Gastroenterology and Hepatology, University of Maryland Medical Center, MD, USA.
Received date: January 26, 2024
Accepted date: February 02, 2024
Published date: February 05, 2024
Citation: Ebehiwele Ebhohon, Olumuyiwa A Ogundipe, Chineye B Amuchi, Ikponmwosa Enofe, Adeyinka C Adejumo. et.al. (2024) “The Burden of Different Hospital Readmissions on Outcomes of Alcoholic Hepatitis in the United States (Characters = 87).”, J of Gastroenterology and Hepatology Research, 5(1); DOI: 10.61148/2836-2888/GHR/044.
Copyright: ©22024 Ebehiwele Ebhohon. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background and Aim: Alcoholic hepatitis (AH) is the most acute presentation of alcoholic liver disease, accounting for a high readmission rate to the same or a different hospital (DHR). DHR is associated with fragmentation of care and results in poor outcomes. In this study, we report the national burden of DHR among hospitalization of AH in the United States.
Methods: Among adults (aged ³18 years) surviving an initial hospitalization for AH from January to September 2010–2014 from the Nationwide Readmissions Database, we identified patients readmitted at 30 and 90 days. We then estimated the rate and trends, predictive factors (demographic, comorbid, liver- and hospital-related), and the impact of DHR on outcomes of AH (mortality, length of stay, and hospital charges) for 30- and 90-day readmissions (SAS 9.4).
Results: Of the 21 572 hospitalizations for AH, 22.8% (4917) and 36.6% (7890) were readmitted within 30 and 90 days, respectively. The DHR rates at 30- and 90-day readmissions (29.4% and 30.7%) were similar and unchanged from 2010 to 2014 (P-trends>0.05). After multivariate adjustment, young age (18–44 years vs. 45– 64 years or ≥65 years), hospital features (hospitals with a small bed size, large metropolitan and non-teaching facilities), and absence of ascites were associated with higher odds of DHR. Compared to initial hospitalization for AH, DHR was associated with a longer duration of admission (0.4 and 0.6 days) and extra hospital charges ($6575 and $5897) but no difference in mortality.
Conclusions: Further studies are needed to understand the factors driving these DHRs and guide public health measures toward reducing the burden of DHR in AH.
alcoholic hepatitis; charges; length of stay; mortality; nationwide readmissions database; odds; risks
Introduction:
Chronic alcohol consumption leads to alcoholic liver disease (ALD), a spectrum of medical conditions ranging from uncomplicated steatosis to alcoholic hepatitis (AH) and alcoholic cirrhosis [1,2]. Among these disease entities within ALD, AH is the most severe manifestation. While the incidence of AH is unclear, research suggests that 10 to 35% of heavy drinkers have liver changes consistent with AH [3-5]. AH is a potentially life-threatening condition triggered by the release of alcohol-induced inflammatory markers and cytokines, leading to increased intestinal permeability and translocation of gut bacteria into the portal circulation resulting in neutrophil-mediated hepatocyte injury. Likewise, alcohol metabolism depletes glutathione levels leading to increased oxidative stress, liver or multi-organ damage, and increased risk of mortality [6-8]. ALD accounts for nearly fifty percent of the two million deaths from chronic liver disease (CLD) that occur annually [9], and the estimated 30-day mortality rate in AH ranges from <10% in mild forms to > 50% in severe conditions [2,10,11]. Corticosteroids can be used to manage severe AH (Maddrey’s Discriminant Function ≥32 or Model for End-Stage Liver Disease >20) [12]; however, the survival benefit at three months is not sustained at longer follow-ups.
Approximately two million readmissions from various medical conditions occur per annum in the US, with an estimated $26 Billion to Medicare. Out of the $26 billion, an estimated $17 billion is attributed to potentially avoidable readmissions, thus making readmissions a cost-controlling priority [13]. To address this issue, the Centers for Medicare & Medicaid Services (CMS) sets up financial penalties for hospitals with relatively higher rates of Medicare readmissions. As such, readmissions have garnered significant attention in the medical community, presenting an opportunity to lower healthcare costs, improve quality, and increase patient satisfaction at once [14]. Due to AH therapy limitations, patients often shoulder a high readmission burden to control recurrent liver failure symptoms and complications (ascites, variceal bleeding, spontaneous bacterial peritonitis, encephalopathy, and sepsis). These limitations ultimately lead to worse AH outcomes and high hospital charges despite recent studies revealing a steady decline in the average length of hospital stay (LOS) [2-4, 6,7].
Readmissions for Alcoholic hepatitis (AH) could be to the same or a different hospital (DHR). Different hospital readmission (DHR) is when hospital readmissions occur in centers distinct from the original place of care, leading to fragmentation of care that is widely recognized as a marker of healthcare quality and is hypothesized to decrease the quality of care received, increase hospital costs, and healthcare utilization [15]. Unfortunately, research on the predictors and patterns of DHR in AH is lacking. Such data is needed to formulate recommendations to decrease the burden of DHR in AH. Therefore, in this study, we aim to 1) report the frequency and trends of DHR, 2) highlight the crucial predictors for DHR, and 3) examine the effect of DHR on clinical outcomes, including LOS, mortality, and hospital-related charges in hospitalized patients with AH in the US.
Methods
Study Design and Data Source:
We performed a retrospective cohort analysis of discharge records from 2010 to 2014 Nationwide Readmission Database (NRD). The NRD is a sample of inpatient discharge records from community hospitals, including academic medical, general, and specialty centers in the United States [16]. It is US's largest publicly available inpatient database containing hospital discharge records. However, the NRD does not include race information or documents from institutionalized centers, prisons, mental health facilities, rehabilitation centers, or military hospitals. NRD has approximately 17 million unweighted records per year, with each record having over 25 clinical diagnoses and 15 procedures, all encoded with the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM). It has unique patient identification that allows patients to be monitored longitudinally for rehospitalizations. We did not seek institutional review board approval for this study because the NRD is de-identified and publicly available.
Study Cohort and Covariates:
Using ICD-10-CM codes (K70.1), we selected patients aged >18 years hospitalized with a primary discharge diagnosis of Alcoholic Hepatitis from 2010 to 2014 (Figure 1 and Table S1) to ensure that each hospitalized patient post-discharge could be followed up for up to 3 months. The 571.1 code has a moderate positive predictive value of 67% for AH [17] and has been used in other administrative data fields [6,18].
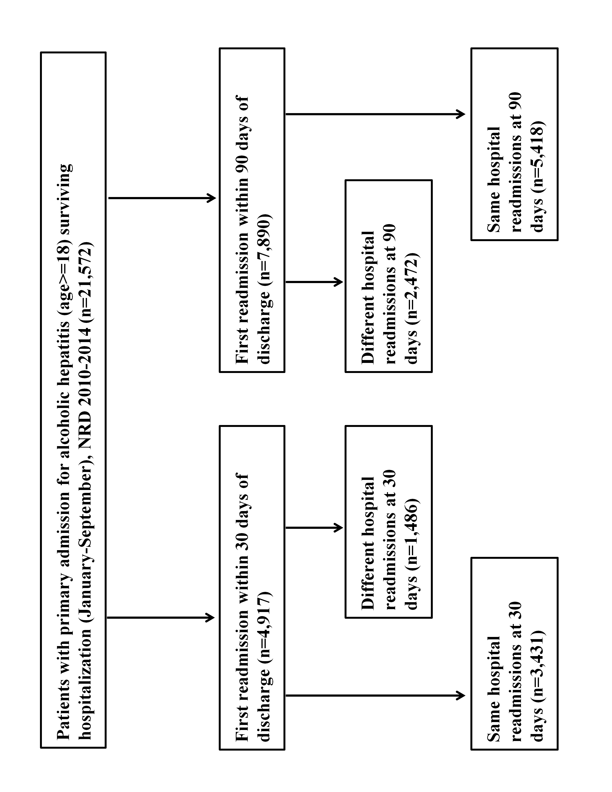
]Figure 1: Patient selection flow chart
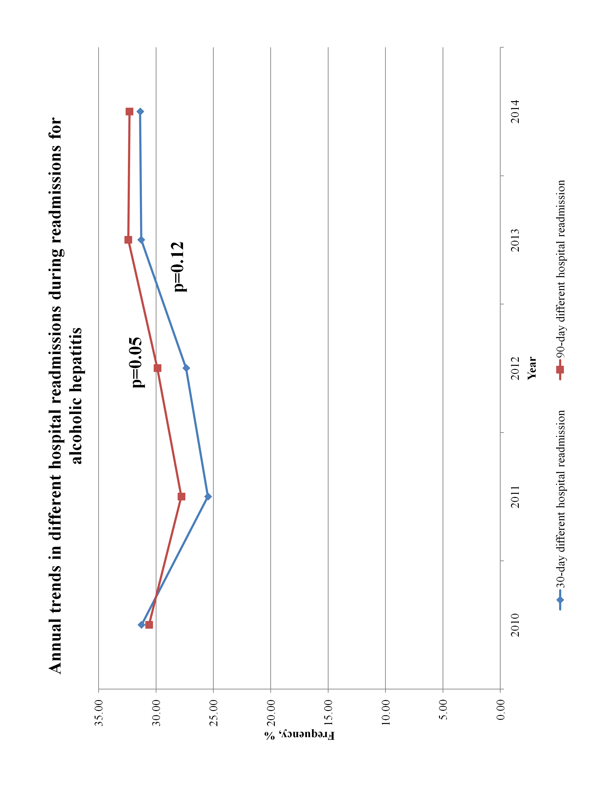
Figure 2: Annual trends in different hospital readmissions during readmissions for alcoholic hepatitis
|
Clinical Condition |
ICD-9-CM Codes, Elixhauser Comorbidity variables and Clinical Classification System codes |
|
Alcoholic hepatitis |
571.1 |
|
Liver cirrhosis |
571.2, 571.5, 571.6 |
|
Decompensation: |
|
|
Protein Energy Malnutrition |
260.x, 261.x, 262.x, 263.x, 269.8, 799.4, 783.3, 783.21, 783.22, 783.7 |
|
Liver transplant |
V42.7, 50.5 (procedure) |
|
Liver cell carcinoma |
155.0 |
|
Charlson-Deyo comorbidities |
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130-1139. |
Table S1: ICD-9-CM codes for identifying clinical conditions in the Nationwide Readmissions Database dataset.
Outcomes:
The primary outcome was the prevalence of DHR at 30- and 90 days after an index hospital admission for AH. Patients who survived the initial hospitalization were reviewed during the 3-month follow-up period for the first readmissions within 30 days. Among the first readmissions, those readmitted to a different hospital from the initial hospital were identified using the unique hospital identification numbers and termed DHR at 30 days. This analysis was repeated for the first readmissions within a 90-day follow-up period to determine DHR at 90 days. All planned interhospital transfers of care and readmissions to the same hospital at 30-or 90-day were excluded from our study. Secondary outcomes in the study were mortality rate, length of stay (LOS), and total hospital charges (THC) during 30- and 90-day readmissions due to DHR. We adjusted for inflation for individual calendar years so that the hospital charges at 30-or 90-day were comparable to previous years.
Covariates:
Biodemographic characteristics, health insurance coverage, and hospital-related factors associated with initial hospitalization were identified from the NRD and reported. Covariates include age >18 years (stratified into three categories: 18-44, 45-64, and > 65), sex (male and female), median household income, primary health insurance coverage, the timing of hospital admission (weekend vs. weekday), disposition at discharge (discharge home, non-routine discharge, and leaving against medical advice [LAMA]). Liver disease-related factors included ascites, variceal bleeding, hepatorenal syndrome, hepatic encephalopathy, portal hypertension, spontaneous bacteria peritonitis (SBP), protein-energy malnutrition (PEM), liver cancer, and receipt of a liver transplant. Furthermore, factors specific to the index hospital were identified from the NRD and included (bed size, teaching status, urban-rural designation, and hospital control). Several comorbid diseases that may influence the clinical status of the patients were identified using ICD-10-CM codes. The Charlson-Deyo Index was computed by aggregating the presence of comorbid conditions from different organs into one score, which was then categorized into 3: 0, 1–3, and >3. End-stage liver disease and cancer presence were not used to calculate the Charlson-Deyo index in this study [19].
Statistical Analysis:
The aggregate and annual rates of DHR from 2010 to 2014 were calculated and summarized as percentages. Categorical variables were also summarized with percentages, while numerical variables were summarized and compared with the mean and Student T-test. The rate of DHR was derived from the proportion of patients with rehospitalizations between the specified period after an index hospitalization for AH. A multivariate survey-weighted logistic analysis was used to determine the factors associated with DHR. This multivariate model included demographics, comorbid, liver-related, and hospital-related characteristics. Finally, survey-weighted multivariate models were utilized to determine the association between DHR and clinical outcomes (Mortality, LOS, THC). A logistic model was used for mortality, a negative binomial for LOS, and a gamma model for THC. All analyses were conducted with the Statistical Analysis System (SAS V.9.4, SAS Institute Inc., Cary, NC, USA), accounting for the multi-level complexity of the survey design. A P-value of <0.05 was chosen as the level of statistical significance.
Results:
Rate and Annual trends of DHR in AH:
There were 21,572 unique hospitalizations for AH from January to September of each calendar year from 2010 to 2014, out of which 4,917 (22.8%) were readmitted within 30-days and 7,890 (36.6%) as readmitted within 90 days of hospital discharge. Among the 4,917 patients readmitted within 30 days of discharge, 1,486 (29.4%) were DHR, while 2,472 (30.7%) of the 7,890 readmissions at 90 days were DHR (Figure 1). The annual rates of DHR at 30-and 90-day readmissions were similar and remained unchanged from 2010 to 2014 (p-trends>0.05) (Figure 3 and Table S3).
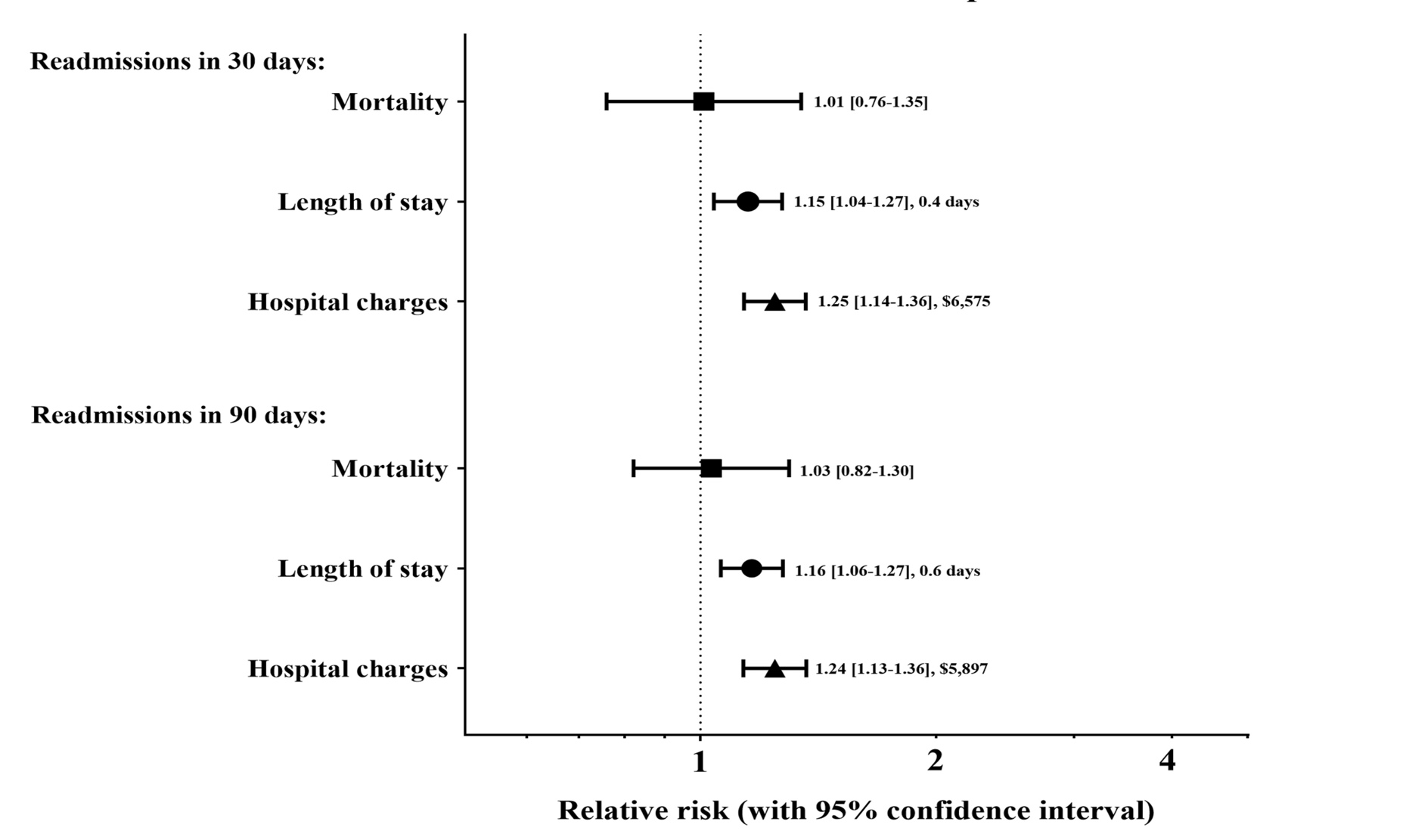
Figure 3: Association between different hospital readmissions and outcomes of readmissions for alcoholic hepatitis
|
Year |
30-day |
SD |
90-day |
SD |
|
2010 |
31.27 |
4.43 |
30.61 |
3.18 |
|
2011 |
25.48 |
3.48 |
27.79 |
2.80 |
|
2012 |
27.37 |
3.60 |
29.88 |
2.85 |
|
2013 |
31.29 |
3.13 |
32.42 |
2.56 |
|
2014 |
31.38 |
2.92 |
32.32 |
2.48 |
|
2010-2014 |
29.43 |
1.54 |
30.70 |
1.23 |
Table S3: Trends in frequency of different hospital readmissions for alcoholic hepatitis
Factors associated with DHR in AH:
Baseline sociodemographic characteristics in patients with the same versus different readmissions were comparable during 30- and 90-day readmissions. Compared with patients readmitted to the same hospital, the risk of DHRs was more likely among young patients without health insurance. Patients with DHRs were also more likely to have been initially admitted to hospitals with small beds or non-teaching in large metropolitan areas run on a private-profit model. Furthermore, patients who left against medical advice and have a high comorbidity burden, such as ascites, variceal bleeding, portal hypertension, and spontaneous bacterial peritonitis, were more likely to have higher readmissions rates on 30 and 90 days (Table 1). On multivariate analysis (Table 2), factors associated with high DHRs were young patients, small bed size hospitals, large metropolitan hospitals, and teaching centers at both 30- and 90-day readmissions. Surprisingly, the lowest quartile income earners and non-routine discharge were only predictive of DHR at 90 days. Only ascites were associated with a reduced risk of DHR at 30 and 90 days among all liver cirrhosis complications. No significant difference was found with variceal bleeding, hepatic encephalopathy, portal hypertension, and spontaneous bacterial peritonitis. Also, hepatorenal syndrome, liver cancer, and liver transplant were not predictive of DHR at 30 and 90 days.
|
30 day readmission (n=4,917) |
90 day readmission (n=7,890) |
||||||
|
Same |
Different |
p-value |
Same |
Different |
p-value |
||
|
Age, years, mean (sd) |
47.3 (10.7) |
45.8 (10.5) |
<0.0001 |
47.0 (10.9) |
45.6 (10.6) |
<0.0001 |
|
|
Age, categorized |
|
|
0.0016 |
|
|
<0.0001 |
|
|
18-44-years |
38.8 |
44.5 |
|
39.9 |
44.9 |
|
|
|
45-64-years |
55.9 |
51.8 |
|
54.7 |
51.5 |
|
|
|
>=65-years |
5.3 |
3.7 |
|
5.4 |
3.6 |
|
|
|
Sex, female, % |
43.0 |
42.4 |
0.7173 |
42.1 |
42.0 |
0.9737 |
|
|
Insurance, % |
|
|
0.0033 |
|
|
0.0038 |
|
|
|
Medicare |
14.9 |
14.2 |
|
15.7 |
15.2 |
|
|
|
Medicaid |
32.9 |
31.2 |
|
31.8 |
31.2 |
|
|
|
Private |
28.1 |
24.8 |
|
26.9 |
23.6 |
|
|
|
Self-pay & others* |
24.0 |
29.8 |
|
25.6 |
30.0 |
|
|
Income, % |
|
|
0.6612 |
|
|
0.806 |
|
|
|
Lowest Quartile |
28.7 |
29.7 |
|
29.2 |
29.2 |
|
|
|
Second Quartile |
24.6 |
25.8 |
|
25.5 |
25.9 |
|
|
|
Third Quartile |
24.2 |
23.6 |
|
23.6 |
24.3 |
|
|
|
Highest Quartile |
22.5 |
21.0 |
|
21.7 |
20.6 |
|
|
Hospital bedsize, % |
|
|
<0.0001 |
|
|
<0.0001 |
|
|
|
Small |
12.5 |
17.8 |
|
12.4 |
17.5 |
|
|
|
Medium |
22.9 |
26.7 |
|
23.4 |
25.6 |
|
|
|
Large |
64.5 |
55.5 |
|
64.2 |
56.9 |
|
|
Hospital urban-rural designation, % |
|
|
<0.0001 |
|
|
<0.0001 |
|
|
|
Large metropolitan |
55.9 |
65.0 |
|
54.8 |
64.4 |
|
|
|
Small metropolitan |
37.4 |
27.4 |
|
37.3 |
28.8 |
|
|
|
Micropolitan |
5.0 |
5.1 |
|
6.0 |
4.9 |
|
|
|
Non-micro/metro-politan |
1.7 |
2.5 |
|
1.9 |
1.9 |
|
|
Hospital teaching status, % |
|
|
0.0003 |
|
|
<0.0001 |
|
|
|
Metropolitan non-teaching |
32.7 |
38.8 |
|
34.0 |
38.9 |
|
|
|
Metropolitan teaching |
60.6 |
53.6 |
|
58.1 |
54.3 |
|
|
|
Non-Metropolitan |
6.7 |
7.6 |
|
7.9 |
6.8 |
|
|
Hospital control, % |
|
|
0.0409 |
|
|
0.0402 |
|
|
|
Government |
18.2 |
16.0 |
|
17.4 |
16.2 |
|
|
|
Private, non-profit |
69.6 |
69.2 |
|
70.1 |
68.9 |
|
|
|
Private, profit |
12.2 |
14.8 |
|
12.5 |
14.9 |
|
|
Weekend admission, % |
21.3 |
21.4 |
0.9495 |
22.0 |
21.5 |
0.6644 |
|
|
Discharge disposition, % |
|
|
0.0005 |
|
|
0.001 |
|
|
|
Home |
84.7 |
81.1 |
|
85.2 |
81.7 |
|
|
|
LAMA |
6.2 |
9.6 |
|
6.1 |
8.4 |
|
|
|
Non-routine |
9.0 |
9.2 |
|
8.7 |
9.9 |
|
|
Complications of chronic liver disease, % |
|
|
|
|
|
|
|
|
|
Ascites |
25.6 |
19.3 |
<0.0001 |
22.1 |
17.2 |
<0.0001 |
|
|
Variceal bleed |
5.5 |
4.0 |
0.0466 |
5.2 |
3.9 |
0.0358 |
|
|
Hepatorenal syndrome |
2.7 |
1.8 |
0.0898 |
2.2 |
1.6 |
0.1771 |
|
|
Hepatic encephalopathy |
11.5 |
8.2 |
0.0019 |
9.4 |
7.9 |
0.0545 |
|
|
Portal hypertension |
14.8 |
11.4 |
0.0056 |
13.2 |
10.7 |
0.0029 |
|
|
Jaundice |
6.2 |
5.8 |
0.5919 |
5.4 |
5.1 |
0.6886 |
|
|
Spontaenous bacterial peritonitis |
2.1 |
1.1 |
0.0167 |
1.7 |
1.0 |
0.0235 |
|
|
PEM |
19.9 |
18.5 |
0.3128 |
18.2 |
17.2 |
0.3601 |
|
Liver cancer, % |
0.3 |
0.2 |
0.3138 |
0.4 |
0.2 |
0.2253 |
|
|
Liver transplant, % |
0.3 |
0.1 |
0.1627 |
0.2 |
0.2 |
0.9518 |
|
|
Charleson-Deyo comorbidity index, % |
|
|
0.4277 |
|
|
0.0956 |
|
|
|
Deyo: 0 |
68.5 |
69.9 |
|
68.4 |
70.5 |
|
|
|
Deyo: 1-3 |
29.0 |
28.3 |
|
29.2 |
27.8 |
|
|
|
Deyo: >3 |
2.4 |
1.8 |
|
2.4 |
1.6 |
|
Table 1: Characteristics of patients admitted for alcoholic hepatitis at 30- and 90-day readmissions by different hospital readmissions, Nationwide Readmissions Database dataset, 2010-2014
|
30 day readmission |
90 day readmission |
||||||||
|
Odds ratio |
Lower confidence limit |
Upper confidence limit |
p-value |
Odds ratio |
Lower confidence limit |
Upper confidence limit |
p-value |
||
|
Age |
|
|
|
0.0037 |
|
|
|
<0.0001 |
|
|
|
45-64- vs. 18-44-years |
0.82 |
0.70 |
0.96 |
|
0.84 |
0.74 |
0.96 |
|
|
|
>=65- vs. 18-44-years |
0.52 |
0.33 |
0.82 |
|
0.50 |
0.36 |
0.69 |
|
|
Female vs. male |
0.99 |
0.85 |
1.14 |
0.8476 |
1.01 |
0.90 |
1.14 |
0.8481 |
|
|
Insurance |
|
|
|
0.0556 |
|
|
|
0.0318 |
|
|
|
Medicaid vs. Medicare |
0.88 |
0.67 |
1.15 |
|
0.88 |
0.72 |
1.09 |
|
|
|
Private vs. Medicare |
0.89 |
0.66 |
1.19 |
|
0.82 |
0.66 |
1.02 |
|
|
|
Self-pay & others* vs. Medicare |
1.12 |
0.84 |
1.49 |
|
1.03 |
0.83 |
1.28 |
|
|
Income |
|
|
|
0.12 |
|
|
|
0.0373 |
|
|
|
Second Quartile vs. Lowest Quartile |
0.96 |
0.77 |
1.19 |
|
0.96 |
0.82 |
1.13 |
|
|
|
Third Quartile vs. Lowest Quartile |
0.88 |
0.71 |
1.07 |
|
0.93 |
0.79 |
1.09 |
|
|
|
Highest Quartile vs. Lowest Quartile |
0.78 |
0.63 |
0.97 |
|
0.79 |
0.67 |
0.93 |
|
|
Hospital bedsize |
|
|
|
<0.0001 |
|
|
|
<0.0001 |
|
|
|
Medium vs. Small |
0.76 |
0.60 |
0.97 |
|
0.75 |
0.62 |
0.91 |
|
|
|
Large vs. Small |
0.59 |
0.48 |
0.73 |
|
0.63 |
0.53 |
0.74 |
|
|
Hospital urban-rural designation |
|
|
|
<0.0001 |
|
|
|
<0.0001 |
|
|
|
Small metropolitan vs. Large metropolitan |
0.61 |
0.51 |
0.72 |
|
0.63 |
0.55 |
0.73 |
|
|
|
Micropolitan vs. Large metropolitan |
1.05 |
0.74 |
1.48 |
|
0.75 |
0.57 |
0.99 |
|
|
|
Non-micro/metro-politan vs. Large metropolitan |
1.19 |
0.86 |
1.67 |
|
0.75 |
0.52 |
1.08 |
|
|
Teaching vs. non-teaching |
1.37 |
1.16 |
1.62 |
0.0002 |
1.25 |
1.09 |
1.42 |
0.001 |
|
|
Hospital control |
|
|
|
0.2807 |
|
|
|
0.5335 |
|
|
|
Private, non-profit vs. Government |
1.17 |
0.96 |
1.43 |
|
1.07 |
0.91 |
1.25 |
|
|
|
Private, profit vs. Government |
1.17 |
0.91 |
1.52 |
|
1.13 |
0.91 |
1.40 |
|
|
Discharge disposition |
|
|
|
0.0104 |
|
|
|
0.0016 |
|
|
|
Home/Routine vs. Non-routine |
0.82 |
0.63 |
1.06 |
|
0.71 |
0.58 |
0.88 |
|
|
|
LAMA vs. Non-routine |
1.14 |
0.80 |
1.63 |
|
0.88 |
0.66 |
1.18 |
|
|
Weekend admission |
0.98 |
0.83 |
1.16 |
0.8478 |
0.96 |
0.84 |
1.10 |
0.533 |
|
|
Complications of chronic liver disease |
|
|
|
|
|
|
|
|
|
|
|
Ascites |
0.78 |
0.63 |
0.95 |
0.0152 |
0.79 |
0.67 |
0.94 |
0.0084 |
|
|
Variceal bleed |
0.85 |
0.58 |
1.26 |
0.427 |
0.86 |
0.63 |
1.16 |
0.3252 |
|
|
Hepatorenal syndrome |
1.00 |
0.59 |
1.70 |
0.9913 |
0.99 |
0.59 |
1.67 |
0.9795 |
|
|
Hepatic encephalopathy |
0.86 |
0.64 |
1.14 |
0.2809 |
1.00 |
0.80 |
1.24 |
0.9665 |
|
|
Portal hypertension |
1.02 |
0.79 |
1.32 |
0.8806 |
0.99 |
0.81 |
1.21 |
0.9004 |
|
|
Jaundice |
1.14 |
0.83 |
1.58 |
0.4216 |
1.11 |
0.85 |
1.44 |
0.437 |
|
|
Spontaneous bacterial peritonitis |
0.61 |
0.34 |
1.08 |
0.0877 |
0.65 |
0.39 |
1.08 |
0.0929 |
|
|
PEM |
1.01 |
0.83 |
1.23 |
0.8995 |
1.02 |
0.87 |
1.19 |
0.8175 |
|
Charlson-Deyo comorbidity index |
|
|
|
0.8089 |
|
|
|
0.3547 |
|
|
|
Deyo: 1-3 vs. 0 |
1.00 |
0.85 |
1.19 |
|
0.97 |
0.85 |
1.10 |
|
|
|
Deyo: >3 vs. 0 |
0.85 |
0.51 |
1.41 |
|
0.74 |
0.49 |
1.13 |
|
|
Liver cancer |
0.86 |
0.20 |
3.78 |
0.8415 |
0.76 |
0.28 |
2.04 |
0.5837 |
|
|
Liver transplant |
0.55 |
0.11 |
2.72 |
0.4605 |
1.39 |
0.38 |
5.09 |
0.6158 |
|
|
LOS, per 5 days |
1.00 |
0.94 |
1.06 |
0.8729 |
0.97 |
0.92 |
1.02 |
0.2081 |
|
|
Liver cirrhosis |
|
|
|
0.5262 |
|
|
|
0.045 |
|
|
|
Compensated vs. no-cirrhosis |
1.1 |
0.8 |
1.4 |
|
1.2 |
1.0 |
1.5 |
|
|
|
Decompensated vs. no-cirrhosis |
1.2 |
0.9 |
1.8 |
|
1.3 |
1.0 |
1.7 |
|
Table 2: Factors associated with different hospital readmissions at 30- and 90-day readmissions for alcoholic hepatitis in multivariate models, Nationwide Readmissions Database dataset, 2010-2014
Impact of DHR on AH Outcomes:
DHR was associated with poorer clinical outcomes (Fig. 3, Table 3, and Table S2). DHR was associated with about 15–16% longer hospital stays, resulting in 0.4 extra days of hospitalization at 30 days (3.3 vs. 2.9 days, P < 0.01) and 0.6 additional days of hospitalization at 90 days (4.2 vs 3.6 days; P < 0.01) readmissions, respectively. Similarly, DHR was associated with 33% increased hospital charges at 30-day readmission, resulting in $6575 extra hospital charges ($26 314 vs. $19 739; P < 0.0001) and 24% higher charges at 90-day readmissions, which is $5897 additional charges at 90-day readmissions ($30 069 vs $24 172; P < 0.0001). However, there was no difference in mortality at both 30-day (9.3% vs. 9.9%; P = 0.9445) and 90-day (8.2% vs. 8.3%; P = 0.7853) readmissions.
|
30-day readmissions |
90-day readmissions |
|||||||
|
Odds ratio |
Lower confidence limit |
Upper confidence limit |
p-value |
Odds ratio |
Lower confidence limit |
Upper confidence limit |
p-value |
|
|
Mortality |
1.01 |
0.76 |
1.34 |
0.9445 |
1.03 |
0.82 |
1.30 |
0.7853 |
|
Length of stay |
1.15 |
1.04 |
1.27 |
0.0065 |
1.16 |
1.06 |
1.27 |
0.0012 |
|
Total hospital charges |
1.24 |
1.14 |
1.36 |
<0.0001 |
1.24 |
1.13 |
1.36 |
<0.0001 |
Table 3: Association between different hospital readmissions and outcomes during 30- and 90-day readmissions, Nationwide Readmissions Database dataset, 2010-2014.
|
Different hospital |
Same hospital |
Different vs. same hospital |
|
|
|
Adjusted Mean |
Adjusted Mean |
Adjusted Mean Difference |
p-value |
|
|
Mortality, % |
|
|||
|
30-day readmissions |
19.5 (7.2-52.9) |
19.3 (7.6-49.3) |
0.2 (-0.4-3.6) |
0.9445 |
|
90-day readmissions |
14.4 (6.2-33.8) |
14.0 (6.3-31.2) |
0.5 (-0.1-2.7) |
0.7853 |
|
Length of stay, days |
||||
|
30-day readmissions |
3.3 (2.1-5.2) |
2.9 (1.8-4.4) |
0.4 (0.2-0.8) |
0.0065 |
|
90-day readmissions |
4.2 (2.8-6.3) |
3.6 (2.4-5.4) |
0.6 (0.4-1.0) |
0.0012 |
|
Total hospital charges $ |
|
|||
|
30-day readmissions |
26314.0 (13678.0-50624.0) |
19739.0 (10461.0-37246.0) |
6575.0 (3217.0-13378.0) |
<0.0001 |
|
90-day readmissions |
30069.0 (17949.0-50372.0) |
24172.0 (14555.0-40143.0) |
5897.0 (3394.0-10229.0) |
<0.0001 |
Table S2: Adjusted outcomes during different hospital readmissions for alcoholic hepatitis readmissions.
Discussion:
Alcoholic hepatitis (AH) accounts for a substantial percentage of hospital readmissions [2]. Our large retrospective analysis is the only study to investigate the national burden of DHR on the outcomes of AH in the United States. Our study observed that one in three readmissions after initial hospitalization for AH was DHR. Our analysis also noted a stable trend in DHR from 2010 to 2014. Furthermore, predictors of higher rates of DHR were young age, initial hospitalizations at small bed size non-teaching hospitals, and the absence of ascites. Finally, DHR was associated with a higher healthcare burden, longer duration of stay, and higher hospital charges during readmissions, but there was no difference in mortality.
Among patients with AH, the all-cause 30-day readmissions rate (22.8%) was similar to the AH readmissions rates (22.8% and 23.9%) found in other studies that used identical large databases for the period 2010-2014 -2,6]. We could not directly compare our 90-day readmissions rate for AH (36.6%) because there's currently a need for research on the 90-day readmission rate for AH besides our previous study [6]. When compared to the 90-day readmissions for other medical conditions, our rate was similar to the rate in cirrhotic patients with three or more complications of cirrhosis (36%) [20] but higher than the rate for acute pancreatitis (22.9%) [21], thus highlighting the high disease burden found in AH.
Among the 22.8% who were readmitted in 30 days, 29.4% were DHR, which is higher than the readmission rates in heart failure (21%) [22], acute pancreatitis (28%) [21], and inflammatory bowel disease (26-28%) [23], but lower than the rates in chronic pancreatitis (33%) [21], and liver cirrhosis (33%) [24]. Among the 36.6% readmitted in 90 days, 30.7% were DHR. Our 90-day DHR rate was lower than the rates found in acute pancreatitis (32%) and chronic pancreatitis (38%) [21]. Although DHR is sometimes unavoidable, the high rates of DHR in our analysis and previous studies suggest that the quality of transitions of care remains problematic in the health sector, posing significant risks to patient's health outcomes and a source of higher cost to healthcare organizations.
As the burden of AH grows, recognizing the demographic characteristics of high-risk AH patients is necessary to determine patients who are more likely to have DHR [14]. Our report is consistent with previous research findings that highlighted young age, leaving against medical advice, index hospital admission to small bed size, non-teaching facilities located in metropolitan areas, and comorbidities as possible reasons why patients are more likely to have DHR [21,23,25]. The high DHR rates found among young people with AH may be because they are more likely to engage in binge or heavy drinking, be of low socioeconomic status [26,27], and, when acutely ill, are more likely to be driven by the emergency medical services to the hospital closest to their living location which may be different from the hospital of their index admission. Therefore, surveillance activities and screening for excessive alcohol drinking and asymptomatic liver cirrhosis for timely intervention could help decrease the incidence of acute liver disease and, by extension, DHR in this age group [28-30]. Additionally, the hospital pattern among patients with DHR during initial hospitalization (small bed sized and non-teaching facilities) and during readmission (large bed size and teaching facilities) suggests that the high DHRs may be due to the referral of complicated cases to tertiary hospitals for a higher level of care during the index hospitalization, outpatient follow-up visitations or at a patient or caregiver request. Unfortunately, we could not investigate the dominant cause of these hospital patterns because the NRD database does not contain outpatient visits or referral details. Regardless, our result suggests that early referral from smaller centers to specialized centers with hepatology care may be needed for medical optimization. Surprisingly, only ascites were associated with a reduced risk of DHR at 30- and 90- days among all liver cirrhosis complications. The reduced risk of DHR with ascites may be because patients are more likely to return to the same hospital where they have been well-integrated for regular paracentesis.
Our study also revealed that higher charges and more extended stays occur among patients with DHR at both 30- and 90-day readmissions. A study noted that less than 30 percent of health systems' electronic health records (HER) are interoperable, with just 18.7% of hospitals using health information transferred from an outside health facility [31]. Consequently, our study's higher readmission costs may be related to clinicians duplicating diagnostic testing and imaging or placing new consults whenever a DHR occurs due to interoperability-related issues in the HER systems [32,33] or lack of use of outside data for patient care. Similarly, the longer LOS may be due to patients’ complex cases that require additional days for proper management or delays in information transfer from the referring to the receiving health facility [34]. However, we did not detect a difference in mortality rate with DHR, which is consistent with another study among patients with cirrhosis [24].
This study has several potential limitations. First, our analysis is limited by the accuracy of the NRD database, as cases of alcoholic hepatitis are retrieved with ICD-9-CM, which has a moderate positive predictive value (PPV) of 67% for the disease [17]. Such a PPV implies that almost one-third of our study population of alcoholic hepatitis does not truly have the disease, which invariably impacts our findings' validity. Furthermore, the validity of our study may be confounded by unobserved characteristics like post-discharge follow-up activities, access to alcohol rehabilitation centers, etc., that are not present in administrative claims. Second, the ICD-9-CM diagnosis codes are primarily used for reimbursement purposes and only secondarily for epidemiological research, thus impacting how data for illness severity and comorbidities are represented, which could lead to under-or over-estimation of the seriousness of the AH. Third, the NRD database does not include information on planned and unplanned readmissions to help identify whether some DHRs were planned/scheduled from outpatient care. Fourth, our study may underestimate or overestimate the rates in AH due to limitations in accounting for different hospital readmissions in AH patients who had an initial hospital admission in the last 30 to 90 days in another State where NRD data is not available. Fifth, the database does not contain medication (diuretics, rifaximin, lactulose, acamprosate, naltrexone, etc.) or dietary compliance that impacts AH outcome. Sixth, the NRD does not include information on inpatient diagnostic workups, referrals, or consults which may help identify patients with AH that have a high risk for readmission after discharge. Finally, the NRD database does not contain post-discharge outpatient follow-up activities and social support available that may impact readmissions and DHR rates. Despite these limitations, our study was strengthened by using an extensive database representing many US medical centers and patient populations, which allowed us to study the rate and factors associated with DHR among patients with AH at the national level and to estimate its disease and economic burden.
DHR rates are high in AH and are associated with higher hospital charges and increased LOS. Several general measures for reducing DHR have been recommended, like better planning/coordination during discharge to enable prompt outpatient primary care and specialist follow-up, ensuring seamless intercommunication of electronic health information systems, and providing social welfare to high-risk individuals [35]. Findings from our study strongly encourage implementing these public strategies among the young, the uninsured, and low-income earners. Furthermore, clinicians and policymakers should ensure measures that increase AH social support and promote alcohol abstinence to improve AH management and promote high-value care. Additional studies are necessary to provide further insight into unknown factors and predictors of DHR to decrease rates among patients with AH in the United States.
Financial Support: The authors received no financial support for this article's research authorship or publication.
Conflict of interest: The authors disclose no potential conflicts concerning this article’s research, authorship, and publication.
Funding: This work was partially supported by an NIH T32DK063922 grant (Adeyinka C Adejumo). The funders had no role in any of the opinions in this manuscript.
Author Contributions
Ebehiwele Ebhohon and Adeyinka C Adejumo are responsible for the study concept and design, data interpretation, drafting, and critical revision of the manuscript for important intellectual content. Olumuyiwa A Ogundipe, Chineye B Amuchi, Ikponmwosa Enofe, Fidelis C Okoli, Mohamed Abdallah, and Gbeminiyi Samuel are responsible for the critical revision of the manuscript for important intellectual content. Adeyinka C Adejumo was responsible for study concept and design, statistical analysis, and supervising the project. All authors read and approved the final version of the manuscript.