Gastroenterology and Hepatology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2888 | Journal DOI: 10.61148/2836-2888/GHR
Vedat Goral 1*, Sıla Yılmaz Erozbek 2, Kerem Mert Goral 3, Burcu Saka 2.
1Istanbul Medipol University Medical School Department of Gastroenterology. Istanbul.
2Istanbul Medipol University Medical School Department of Pathology. Istanbul.
3Yeditepe Medipol University School of Medicine. Istanbul.
*Corresponding author: Vedat Goral, Istanbul Medipol University Medical School Department of Gastroenterology. Istanbul.
Received date: December 07, 2021
Accepted date: December 30, 2021
published date: January 07, 2022
Citation: Vedat Goral , Sıla Yılmaz Erozbek, Kerem Mert Goral and Burcu Saka. (2022) “Esophageal Granular Cell Tumor”, J of Gastroenterology and Hepatology Research, 3(1); DOI: http;//doi.org/01.2022/2.10125
Copyright: © 2022 Vedat Goral. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Esophageal granular cell tumors (GCTs) are rare, often benign tumors of neurogenic origin. Granular cell tumors (GCTs), first described by Abrikossoff in 1926, are rare tumors that occur in various parts of the body [1,2]. They are generally observed in the gastrointestinal tract, less commonly in the thyroid, respiratory tract, female urogenital tract, nervous system, breast, and gastrointestinal (GI) tract [1,2]. Tumors in the gastrointestinal tract represent only 6-10% of all granular cell tumors, especially the esophagus. In 30-60% of these cases, the most common location is the esophagus [1,3]. These neoplasms are usually solitary and are multifocal lesions in 10% of cases. Although their clinical course is relatively benign, approximately 2% of GCTs are malignant.
Case Report:
A 32-year-old female patient who applied to the Gastroenterology outpatient clinic due to epigastric pain and dyspepsia complaints had been continuing intermittently for 1 year. In the endoscopic examination, it was observed that there was an erosive raised lesion of 4-5 mm in diameter at the 33rd cm from the mouth, and a biopsy was taken from this area and sent to pathology (Picture 1). At the pathologic examination, uniform polygonal or round cells were seen under the microscope (Picture 2). These cells had abundant, fine-grained granular, eosinophilic cytoplasms and small centrally located nuclei. In addition, pseudoepitheliomatous hyperplasia areas were observed in the stratified squamous epithelium of the esophagus (Picture 1,2). Tumor cells were found to be PAS and PAS-D positive in histochemical examination. In the immunohistochemical examination, positive staining was observed with S100 protein and CD68, while GFAP stained negatively (Picture 2). After diagnosis of EGC tumor, endoscopic submukozal disection (ESD) was applied. Now she is under control and she has not any complaint.

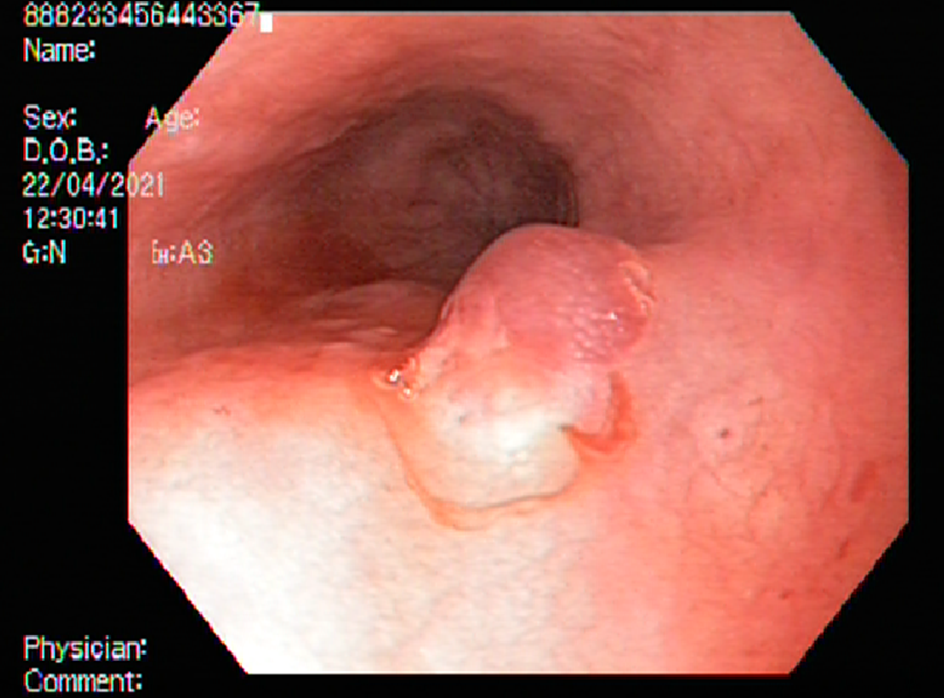
Picture 1: Endoscopic apperance of the lesion
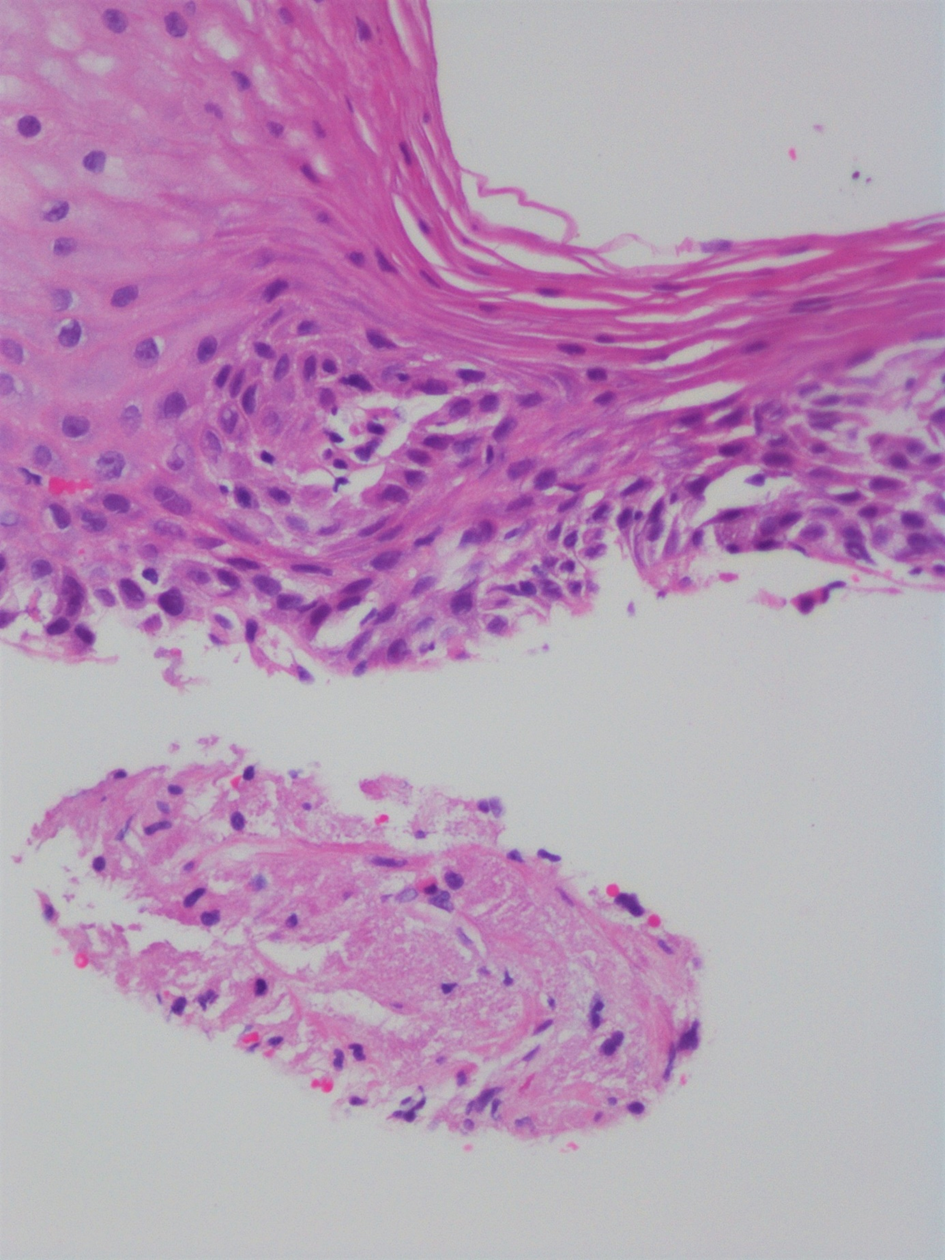
Picture 2: Granular cell tumor-20x-H&E- Fragment consisting of cells with squamous epithelium on the surface, dark, small nuclei, large, granular and eosinophilic cytoplasm in the subepithelial area suggests the diagnosis of granular cell tumor.
Dıscussıon:
Esophageal GHTs commonly occur in the fourth to sixth decade of life, with some reports reporting a slightly higher incidence in women [1-3]. Tumors are typically insidious, with most patients asymptomatic at diagnosis. In fact, granular cell tumors are often found incidentally in the investigation of other GI disorders. When tumors are symptomatic, patients most commonly complain of retrosternal pain and discomfort [4-6]. Less reported symptoms include epigastric pain, nausea or vomiting. These symptoms correlate with lesion size with lesions <20 mm in diameter.
Malignant esophageal GCTs are extremely rare, with <40 cases described in the literature, accounting for only 2% of cases. Although there is no racial predisposition for benign tumors, one study found that malignant GCTs are most common in African American women. found to occur in African American women. any other population. The same study also reported malignant GCTs for benign tumors, most commonly occurring in the soft tissues of the thigh and in the head and neck region. Unlike the more common GCTs of the tongue and skin, those of the esophagus often lack significant malignant potential.
They are determined during upper gastrointestinal endoscopy in patients who apply to the gastroenterology outpatient clinic with dyspeptic complaints. They are usually benign, but because they have malignant potential, histopathological examination is mandatory for definitive diagnosis and treatment. It has been reported that esophageal granular cell tumors are generally asymptomatic in patients with a tumor diameter of less than 10 mm, and the lesions are detected incidentally during upper endoscopy. Dysphagia is the most common complaint in tumors larger than 10 mm in diameter.
Esophageal granular tumors can sometimes be multiple. Although most of them are benign, histopathological examination is mandatory in terms of diagnosis and treatment, since 1-2% of the cases are reported to be malignant [5]. They are mostly asymptomatic.
Macroscopically, it is solid, yellow in color. They have malignant potential. 1-2% of the cases have been reported as malignant. For esophageal GCTs, it has been reported that patients with a tumor diameter of less than 10 mm are generally asymptomatic, and the lesions are incidentally detected during upper endoscopy. Although most of the cases originate from the mucosa or submucosa, few tumors have been reported to originate from the muscularis propria.
Endoscopically, they are usually seen as a submucosal lesion. They are in the form of yellow fluff. The endoscopic appearance may resemble a leiomyoma. Endoscopic USG and EUS play an important role in diagnosis and treatment. In this way, size, location and depth of invasion can be determined. It has been reported that the definitive diagnosis of granular cell tumors cannot be given by endoscopy and EUS, and histopathology and immunohistochemical examination are mandatory. In some publications, it has been shown that the diagnosis of granular cell tumor is made with EUS-guided fine needle aspiration [7]. In our case, EUS was performed and biopsy was taken from the lesion in the same procedure session.
In differential diagnosis; leiomyoma, GI stromal tumor, esophageal cyst, rhabdomyoma, schwannoma, melanoma, hamartoma, squamous papilloma, squamous cell carcinoma, and metastasis should be considered. A comprehensive study is essential to make an accurate diagnosis and traditionally includes imaging with both EGD and EUS.
EGD shows the classic appearance of an esophageal GCT as a yellow-gray, intramural lesion lined with normal-appearing mucosa, with a yellow-gray consistency, covered with normal-appearing mucosa [5-8]. EUS is used in both the diagnosis and management of esophageal GCTs plays an important role. EUS is invaluable in determining tumor size, location, depth of invasion, and origin of the lesion, and in excluding malignancy and/or lymph node involvement [3,5,6]. The typical finding in EUS is hypoechoic, homogeneous, and smooth-edged. tumor within the mucosa or submucosa [5]. Approximately 95% of esophageal GCTs occur within the mucosa, with the remaining 5% in the submucosa. Both endoscopy and EUS together can easily distinguish GCTs from malignant lesions, esophageal cysts, inflammatory polyps, and lipomas [7-10]. However, GCTs are more echogenic and show posterior shadowing. However, it can be difficult to reliably distinguish lesions in the mucosa and muscularis propria with EUS and endoscopy alone, and a definitive diagnosis is essential on tissue histopathological examination and IHC.
Small, asymptomatic esophageal GCTs (<10 mm in diameter) should be treated conservatively. Therefore, small, asymptomatic esophageal GCTs require annual surveillance with endoscopy and EUS to monitor for growth, recurrence, or malignant transformation. Some authors recommend histological evaluation every 1-2 years, especially in patients with atypical or related feature
Endoscopic or surgical removal is recommended for lesions greater than 10 mm, symptomatic or exhibiting rapid growth, suspected malignancy, or infiltration [9-13]. EMR (endoscopic mucosal resection) is well tolerated in patients with lesions ≤20 mm in diameter and no attachment to the muscularis propria. STER (Submucosal tunneling endoscopic resection) is the newer technique of choice for lesions 20-30 mm in diameter or lesions located in the submucosa but not within the muscularis propria [14]. In addition to its advantages in resection of larger neoplasms, STER provides direct endoscopic visualization and maintenance of the GI tract, promoting wound healing and reducing secondary infection, and the risk of esophageal perforation. Recommend the use of STER as it allows an accurate resection, it is safe and less invasive than traditional techniques such as surgical resection, but is cost-effective. The important point to note, however, is that STER is suitable for patients who can tolerate anesthesia with endotracheal intubation only, since it is performed under general anesthesia. The risks of complications such as , mediastinitis, abscess or stricture formation should be addressed.
In conclusion, esophageal GCTs are rare, usually benign tumors of nervous system origin. They can cause dyspeptic complaints and are detected during endoscopy. Observation of characteristic histopathological features is important for diagnosis. Since they have the potential for malignancy, it is recommended to determine tumor location and spread with EUS, and to perform endoscopic resection by providing sound surgical margins.