Gastroenterology and Hepatology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2888 | Journal DOI: 10.61148/2836-2888/GHR
Mukul Rastogi1, Rakesh Kumar Jagdish1*, Noopur Gupta2, Abhishek Shekhar3
1Department of Hepatology, Gastroenterology, and Liver Transplant Medicine, Fortis Hospital Noida.
*2Department of Hepatology, Gastroenterology and Liver Transplant Medicine, SRL, Fortis Hospital Noida.
3Department of Radiology, Fortis Hospital Noida.
*Corresponding author: Rakesh Kumar Jagdish, Department of Pathology, SRL, Fortis Hospital Noida.
Received date: November 09, 2021
Accepted date: November 16, 2021
published date: November 24, 2021
Citation: Mukul Rastogi, Rakesh K Jagdish, Noopur Gupta, Abhishek Shekhar. (2021) “Post SARS-Cov-2 Infection Related Colonic Ulcerations Masquerading as Gastrointestinal Mass.”, J of Gastroenterology and Hepatology Research, 2(4); DOI: http;//doi.org/11.2021/2.10120.
Copyright: © 2021 Rakesh Kumar Jagdish. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
respiratory symptoms to only gastrointestinal manifestations to completely asymptomatic course. Coronavirus can be found in the stool even after other symptomatic recovery and nasal/pharyngeal swab become negative. Gastrointestinal (GI) involvement in COVID-19 also has varied manifestations which can range from diarrheal illness to necrotising colitis. We hereby reported a case of colonic ulcerations presented as caecal mass which developed during COVID-19 infection recovery.
Case Report:
A case of 42 years old female, without any prior comorbidities, having fever of moderate severity, with shortness of breath, was diagnosed with SARS-CoV-2(COVID-19) infection related pneumonia (COVID-19 RT PCR Positive), for which she received steroids, ivermectin, azithromycin and other supportive treatment. There was no history of NSAIDs, or tocilizumab, remedisvir treatment. She recovered gradually and discharged.
After 7 days of her COVID-19 therapy, she developed pain in right iliac fossa, which was radiating to umbilicus, non-colicky, severe in intensity, visual analogue score (VAS) of 6/10, requiring analgesics, mimicking acute appendicular pain .It was associated with nausea and infrequent vomiting without loose stools, or abdominal distention. There was no history of bleeding per rectum. There were no residual symptoms of cough, shortness of breath, sore throat, or any other symptoms. She denied any chronic medicine use, prior gastrointestinal (GI) symptoms, food allergies, lactose intolerance, alcohol abuse, smoking, and drug use. She was treated with metronidazole and other antibiotics for her abdominal symptoms before presenting to us, with no improvement in symptoms.
Laboratory evaluation showed anaemia with haemoglobin of 10.5 gm/dl, (range 12.1-15.1 g/dl) white blood cell count of 9100 /cumm (range 4500-1100/cumm) with 72% of neutrophils and, platelet count was 245,000/microL (range 150,000-450,000 /microL). ESR-55 mm/1sr hour (range 0-20 mm/hr), INR was 1.0(range 0.8-1.1) and creatinine was 0.85 mg/dL (range 0.59-1.04). Stool for ova and cyst were negative. Stool occult blood test was positive.
Contrast enhanced computed tomography (CECT) scan abdomen showed (Figure 1, A, B) asymmetrical wall thickening of cecum and terminal ileum, needs to rule out malignancy in view of asymmetrical nature of the thickening. Small sub-centimetric hypo dense lesion was also noted in liver, which are difficult to characterized and have no appreciable enhancement on contrast study with possible liver metastasis, in view of asymmetrical ceacal thickening. Appendix, and pancreas were normal. Because of suspicion of malignancy her tumor marker (CA 19.9, CEA, CA 125, AFP) were done which were normal. She came for further evaluation of her GI symptoms, and she underwent colonoscopy, which showed normal ileum and ileo-cecal valve. There were multiple, punched out; friable ulcerations in caecum and ascending colon with in-between normal mucosa without any obvious thickening, biopsies were taken (figure 2, A, B). Differential diagnosis of amoebic colitis, tubercular ulcers, NSAIDs related ulcer, Nonspecific IBD, and Covid related ulceration was considered.
Colonic biopsy (figure3, A, B) showed inflammatory exudates, ulcerations, cryptitis, congested vessels, without microscopic coagulopathy necrosis, PAS stain was negative. Lamina propria showed edema, dense inflammatory infiltrates, no crypt abscess, no evidence of mucin depletion, hemosiderin deposits, no parasite, no vasculitis, no malignancy, no granuloma; Biopsy was suggestive of Nonspecific active colitis with ulcerations likely related to Post COVID-19 Colonic ulcerations. She was referred to us as a possible case of disseminated malignancy with GI involvement, but biopsy and review imaging were not suggestive of malignancy. She was treated conservatively, and her symptoms resolved on follow up and stool occult blood test became negative.
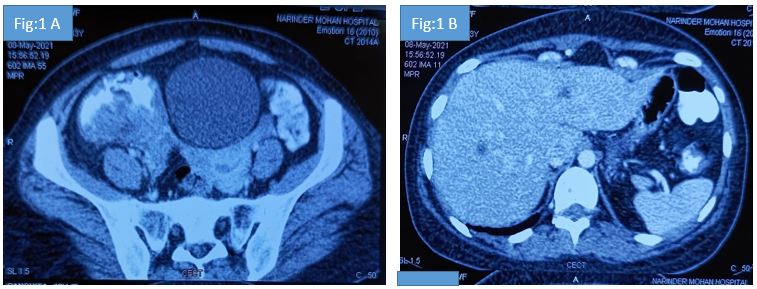
Figure 1: Figure 1A: Abdominal computed tomography showing asymmetrical thickening of the caecum and IC junction. Figure 1B suggestive of < 1 cm hypodense lesions too small to characterize in the liver.
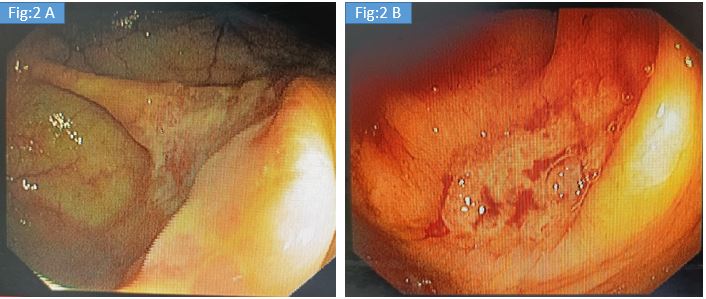
Figure 2: Colonoscopy Images of the cecum (Fig.2A) and ascending colon (Fig.2B) on flexible colonoscopy examination showing ulcerations.
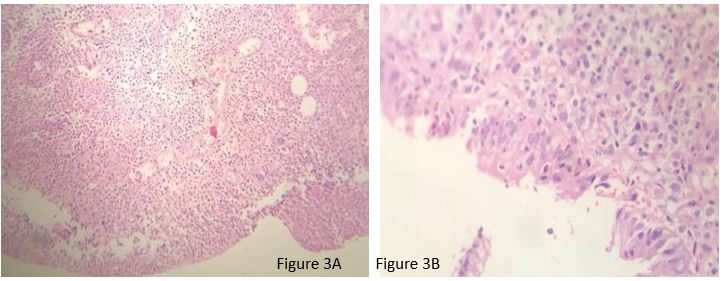
Figure 3: Colonic Biopsy images, H and E stain 10 x (Fig 3A) and 40 x (Fig 3 B): Biopsy of the colonic ulcer showing inflammatory exudate, ulceration, cryptitis, and congested vessels. No microscopic coagulopathy, crypt abscess, mucin depletion, hemosiderin deposits, parasite, vasculitis, malignancy, granuloma was seen.
Discussion:
SARS-CoV-2 (COVID-19)infection has varied manifestations, ranging from most common respiratory symptoms to less common gastrointestinal manifestations .It may have completely asymptomatic course as well.Initial case series reported that 3-10% of patients have initial GI symptoms, who eventually develop pulmonary manifestations [1].GI involvement in Covid also has varied manifestations which can range from anorexia, dyspepsia, nausea, vomiting, diarrheal illness , abdominal pain and necrotising colitis. Gastrointestinal manifestations may be due to binding of the SARS-CoV-2 (COVID-19)virus to ACE 2 receptors (angiotensin converting enzyme-2 receptors) [2] which are prevalent throughout the gut [3].COVID-19 can results GIT inflammation directly via infection of the GI cells or indirectly mediated by cytokines which can results in systemic symptoms and multiple organ involvement [4].
Studies of colonoscopy from Italy, done in the Covid 19 patients showed segmental colitis associated with diverticulosis in 25% cases followed by, ischaemic colitis in 20%and ulcerative haemorrhagic colitis in 5% of cases [5].The colonic ulcers as manifestation or sequel of Covid infection has not reported in literature so far, probably this is the first case report of colonic ulcers as a sequel to Covid infection. There are some case reports of bloody diarrhoea as a clinical manifestation of COVID-19 with or without underlying inflammatory bowel disease [6, 7]. There is also cases with colitis presenting as only presentation of COVID-19 infection [8].Case reports of large bowel involvement in COVID-19 disease characterised by thickening of the ascending, transverse, left colon and case of colonic ileus with air fluid levels [9].Due to the fear associated with the COVID-19 illness, and endoscopy being considered as a high risk procedure [10]. As endoscopy and colonoscopy are aerosols generating procedures it may endanger medical staff, and therefore not routinely performed in COVID-19 patients unless patients with life-threatening gastrointestinal bleeding or oesophageal foreign-body obstruction [11]. So far, no standardised methods established for stool COVID-19 analysis despite its prolonged shedding even after respiratory recovery. Coronavirus can be found in the stool even after other symptomatic recovery and nasal/pharyngeal swab become negative due to prolonged stool shedding .[12] Stool COVID-19 testing should done be in patients of gastrointestinal symptoms with negative nasopharyngeal swab test in a suspected COVID-19 disease [13], therefore methods should be sought for faecal isolation and stool testing for COVID-19.
In the present case, the patient was referred to us as a case of ileo-cecal mass with possible metastasis to liver, in view of radiological findings, but clinical history was not in favour. There are case reports in the form of case series, where colonic ulcers were found to be masquerading as malignancy, particularly tuberculosis in India .It is very difficult to differentiate tuberculosis on endoscopic and radiological features from malignancy or inflammatory bowel disease, therefore biopsy remains the key in such cases [14, 15]. Also, case of ischemic colitis mimicking as tumour are reported [16]. One has to be at utmost awareness to rule out or rule in possible malignancy due to varied presentation, in the current pandemic COVID-19 related GI manifestation must be kept in mind, either treatment related adverse effects or virus-related injury.
Therefore, patient was subjected to colonoscopy and biopsy with all standard precautions of COVID-19 protocols for the colonoscopy procedure to rule out the malignancy or other possible differential diagnosis. In present case we have considered multiple differential diagnosis for the cause of ulcerations which were masquerading as mass on radiological imaging. Firstly, NSAIDS related ulcerations, due to the proximal colonic nature, although history of NSAIDs or over the counter (OTC) drugs was not there. Secondly, tuberculosis related colonic ulcerations was considered, which is more common entity particular in developing countries like India, and suspected involvement of ileum and cecum on imaging, although on colonoscopy, ileum was normal up to 10 cm from ileo-cecal valve. Thirdly, possibility of amoebic ulceration was kept, which usually presents as punched out ulcerations, and also common in India, but this was also ruled out in the biopsy analysis. All the other possible differential diagnosis was ruled out on biopsy evaluation of the lesions. Since such presentation is never reported in contest to COVID-19 infection, it is worthwhile reporting this index case. Moreover, we have limitation of this case report is that the diagnoses are without any kinds of histologic confirmation of COVID-19, but we have ruled out all the alternative possible etiologies.
Ethical statement: No ethical issue
No conflict of interest