Gastroenterology and Hepatology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2888 | Journal DOI: 10.61148/2836-2888/GHR
Mukul Rastogi, Rakesh Kumar Jagdish*
Department of Hepatology, Gastroenterology, and Liver Transplant Medicine, Fortis Hospital Noida, UP, India.
*Corresponding author: Rakesh Kumar Jagdish, Department of Hepatology, Gastroenterology, and Liver Transplant Medicine, Fortis Hospital Noida, UP, India.
Received date: November 09, 2021
Accepted date: November 16, 2021
published date: November 24, 2021
Citation: Mukul Rastogi, Rakesh Kumar Jagdish. (2021) “The Life-Threatening Onset of Celiac Disease: A Rare Case Report of Celiac Diseases with Situs Inverses, Presenting with “Paroxysmal Supraventricular Tachycardia”.”, J of Gastroenterology and Hepatology Research, 2(5); DOI: http;//doi.org/11.2021/2.10121
Copyright: © 2021 Rakesh Kumar Jagdish. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Celiac diseases have varied manifestations ranging from asymptomatic course to celiac crisis. We have seen a rare case of celiac disease (CD), first presented with paroxysmal supraventricular tachycardia (PSVT) due to severe anaemia and underlying situs inverses. This is the first case report of CD associated with situs inverses but without any congenital anomaly.
Case Report:
Mrs SK, 43 years female, admitted with palpitations of two hours duration along with severe weakness, easy fatigability and breathlessness on exertion of one-month duration. She had history of unintentional weight loss of 4 kg in last one month, without any history of loose stools, steotorrhea, vomiting and anorexia. Family history, personal history and past history were not significant.On examination her vitals were unstable with blood pressure of 90/60mmHg, pulse rate of 226 beats /min (which was consistent with PSVT on ECG), respiratory rate was 25/min, which stabilised once her PSVT was controlled with adenosine. Systemic examination showed severe pallor, no icterus, cyanosis or pedal oedema.Other examination was unremarkable, except for dextrocardia.On further evaluation she was found have severe anaemia (Haemoglobin - 4.9 g/dl), and thrombocytopenia (platelets- 45,000 per mcL), MCV-81.9 FL, reticulocyte count was high (7.3%), low vitamin B 12 levels (72.2ng/mL), stool for occult blood was negative, peripheral smear was suggestive of normocytic normochromic with marked anisocytosis, mild thrombocytopenia. Her thyroid stimulating hormone (TSH) was raised (17.03mIU/L). She received two units of packed red blood cells (PRBC) in view of severe anaemia. Further evaluation showed dextrocardia on echocardiography, with ejection fraction of 55% and ultrasound of the abdomen was normal except for situs inverses. Other investigations showed low vitamin D (< 3ng/mL); kidney function test was normal, folic Acid level was 4.12ng/mL, (3.89-26.8), ESR was 16 mm/hr (0-20). Liver functions tests showed total bilirubin 0.84gm/dl, total protein 5.7gm/dl, Albumin-3.7gm/dl, globulin-2.0gm/dl and normal liver enzymes. Her TTG IgA was elevated (74.18 U/mL). Anti endomysial antibody was positive and anti- parietal cell antibody were negative. Her upper GI endoscopy was done which showed scalloped D2 folds (Figure 1) and biopsy taken, report shown in (Figure 2). Haemoglobin electrophoresis showed thalassemia minor, which might have aggravated the severe anaemia induced by coeliac diseases. She was diagnosed with paroxysmal supraventricular tachycardia (reverted), severe anaemia, celiac disease, thalassemia minor, vitamin B12 and folic acid deficiency, hypothyroidism, hypovitaminosis D and situs inverses. She was managed conservatively with gluten free diet and supportive treatment of her nutritional deficiencies. She improved with conservative treatment. Celiac diseases in case of situs inverses never reported earlier in literature.

Figure 1: Endoscopy images showing Scalloped D2 folds
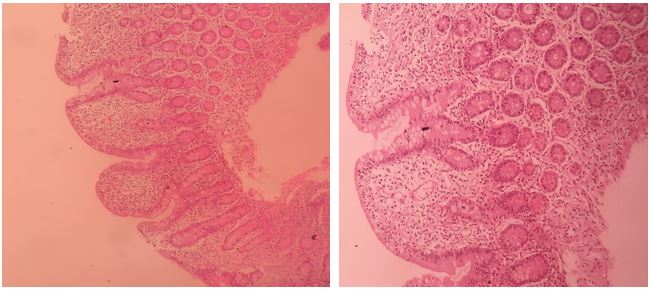
Figure 2: D2 biopsy H and E staining: suggestive of near total villous atrophy with associated crypt hyperplasia. Lamina propria was oedematous and showed dense chronic inflammatory infiltrates. Intraepithelial lymphocytes are increased (45-50/100enterocyte. No giardia/gastric metaplasia seen. Suggestive of coeliac diseases, marsh 3b with mucosal absorptive disorder.
Review of literature:
Our case is rare case of celiac diseases, which is present in a patient with situs inverses, moreover it presented with life- threatening onset PSVT due to severe anaemia, without any manifestations of cardiac anomaly or celiac crisis. This type of presentation is never reported in the literature so far. Situs inverses totalis is a very rare condition which presents in 1 out of 4000–20000 people, and it is characterized by complete transposition of the thoracic and abdominal viscera. [1,2]. The exact cause of this condition is not known. These patients have normal life expectancy unless associated with cardiac or gastrointestinal anomalies [3] .Apart from the cardiac anomalies (3-5% cases), GI anomalies can be present like polysplenia, asplenia, annular pancreas, Biliary Artesia, Duodenal Artesia, Colonic aganglionosis, malrotation of the intestine, diaphragmatic hernia and others [4,5].
This conditionis not a premalignant condition, although rare case reports of GI malignancy reported like gastric cancer and colorectal cancer [6, 7]. Celiac diseases is a multisystem disorder of autoimmune aetiology, common cardiac manifestation [8] are cardiomyopathy, increased thrombosis, cardiovascular risk , atherosclerosis , stroke , arterial function , and ischemic heart disease . Cardiac manifestations mostly showed good response to GFD, which occurs in conjunction with the healing of small intestinal villous atrophy.
In CD, there is increased incidence of Rhythm disturbances, ECG changes, (conduction delay, and p wave abnormalities) [9]. Most common arrhythmia in CD is AF (atrial fibrillation) [10, 11] which is associated with higher risk of stroke and or heart failure. [12] Untreated CD results in chronic inflammation, which is one of risk factors for atrial fibrillation, whereas case of PSVT is rare. CD is also reported with pulmonary hemosiderosis with infranodal heart block, which required a pacemaker [13]. In CD, ASD is most common congenital cardiac defect [14]. In children with congenital heart disease and CD, growth improves on a GFD [15].Severe Cardiac manifestations with celiac are reported as myocarditis,which is attributed to the common autoimmune process toward myocardial antigenic components and small bowel, this can be seen upto>4% of the patients of myocarditis. Immunosuppression and a gluten-free diet are the effective treatment options, patients showed marked improvement in cardiac functions after starting GFD (gluten-free diet), ejection fraction reaching 70 %from 15%. [16].
Our patient showed that celiac can present with life threatening episode, even without underlying cardiac anomaly or celiac crises. Thus, all celiac emergencies are not related to celiac crisis which manifests with profuse diarrhoea, hypotension, electrolyte disturbances and severe metabolic disturbances. This can theoretically manifest with cardiac arrhythmia due to dyselectrolytemia (hypokalemia), although, commonest presenting feature is hypokalemia induced neuromuscular paralysis. [17]. Our patient was having normal electrolytes, and cause of her PSVT was severe anaemia without any GI manifestations. [18] CD is a chronic diseases but acute onset possible in a long-term compensated patient for anaemia, hypoprotenimia, malnutrition or vitamin B12 deficiency related manifestations [19,20] .Care should be taken to avoid treatment related re-feeding syndrome.In a person with celiac disease, repeated exposure to gluten damages the intestinal lining. This can result in nutrient deficiencies that can cause issues such as: Anaemia, Hair loss, osteoporosis , small bowel ulcers, rarely lymphoma, and refractory celiac disease.
Anaemia usually do not present with PSVT, but this was a rare case where severe anaemia have presented with PSVT, without any cardiac anomaly and found to have Celiac diseases on evaluation. Therefore, for evaluation of anaemia and other malabsorption related disorders, one must consider celiac diseases in differential diagnosis and also in life threatening conditions one must keep in mind to rule out celiac diseases.