Gastroenterology and Hepatology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2888 | Journal DOI: 10.61148/2836-2888/GHR
Divya Teja Patil *, Anil Kumar Sakalecha, Parameshwar Keerthi B.H and Yashas Ullas L.
Department of Radiodiagnosis,RL Jalappa Hospital and Research Centre, Tamaka, Kolar, Karnataka, India.
*Corresponding author: Divya Teja Patil, Department of Radiodiagnosis,RL Jalappa Hospital and Research Centre, Tamaka, Kolar, Karnataka, India.
Received date: June 10, 2021
Accepted date: June 16, 2021
published date: June 29, 2021
Citation: Divya T Patil, Anil K Sakalecha, Keerthi B.H.P and Yashas Ullas L. (2021) “Duodenal gastrointestinal stromal tumor – a case report.”, J of Gastroenterology and Hepatology Research, 2(2); DOI: http;//doi.org/06.2021/2.1013.
Copyright: © 2021 Divya Teja Patil. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Gastrointestinal stromal tumours (GIST) are the most common mesenchymal tumours of the gastrointestinal tract (GIT). They account for ~5% of all sarcomas and are mostly found in stomach and mid/distal small bowel.
Introduction:
Gastrointestinal stromal tumours (GIST) are the most common mesenchymal tumours of the gastrointestinal tract (GIT). They account for ~5% of all sarcomas and are mostly found in stomach and mid/distal small bowel.
Epidemiology:
GISTs are rare as compared to carcinoma. Mostly seen in older age group. Incidence is equal in both males and females. Can arise anywhere along the GIT. Most common site is stomach. In duodenum, the incidence is ~ 5 to 10 %. They are believed to arise from the interstitial cells of Cajal 2-3, with 95% staining positive for CD117 (c-KIT) and 70% for CD34. Three different types are recognised: Spindle cell GIST (70%), epithelioid cell GIST (20%), mixed (10%)
Case report:
A 42-year-old male came with generalized weakness and upper abdominal pain, increasing for 2 months and multiple episodes of vomitings and bleeding per rectum for 1 week. No past history.
On USG, a large well-defined mass was seen in right hypochondrium measuring ~ 10.8 x 9.1 x 8.6 cm. The lesion shows central hypo to anechoic areas suggestive of necrotic degeneration. On colour Doppler, the lesion shows central and peripheral vascularity. On CT, a large, well-defined heterogeneously enhancing exophytic mass measuring ~10.4 x 9.0 x 11.1 cm (anteroposterior x transverse x craniocaudal) noted in the lateral wall of 2nd part of duodenum with luminal narrowing. Few arterial feeders are arising from common hepatic artery. Mass effect in the form of displacement of bowel loops inferiorly & inferior vena cava posteriorly. Few peripheral calcifications noted. Antero-laterally, there is focal adhesion of segment VI of liver. Posteriorly, the lesion is abutting & displacing the right kidney superiorly, however no infiltration seen. Supero-medially, the lesion is focally abutting the head of pancreas, however, no obvious infiltration noted. On lateral decubitus study, the contract is seen entering from the lumen into the lesion with few air pockets.
In view of the above findings and supportive clinical history, features of duodenal GIST was given.

Figure 1: A large soft tissue density lesion with central anechoic components in right hypochondrium.
Figure 2: The lesion shows peripheral and internal vascualrity on CDI.
Figure 3: On plain CT, the lesion appears heterogenous with a calcification focus.
Figure 4: CECT abdomen axial section, the lesion shows heterogenous enhancement.
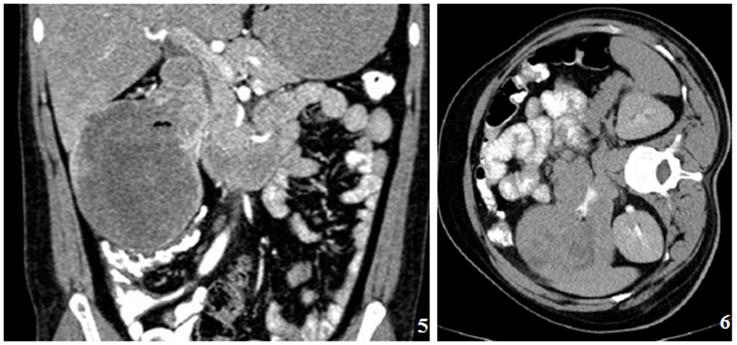
Figure 5: CECT abdomen coronal reforrmated image showing the lesion arising from 2nd part of duodenum.
Figure 6 :On lateral decubitus study, the contrast is seen entering the mass. Few airfoci are also seen in the mass.

Discussion:
Gastrointestinal stromal tumours are the non-epithelial tumours arising from the interstitial cells of Cajal. 80% of malignant duodenal GISTs are located in the second or third portion of the duodenum.
The clinical findings vary depending on the location and size of the tumour at presentation. If the tumour is small, it may be only an incidental finding during radiological imaging or surgery for some other cause, whereas a large exophytic lesion may present as an abdominal mass due to its large size.
Imaging findings:
Barium studies:
Smooth, discrete mass with filling defect when ulcerations are present.
Substantial extraluminal component, only seen on cross-sectional imaging.
CT:
Because most of these tumours are submucosal in location, they usually attain a large size without causing bowel obstruction by the time of diagnosis. [5] Burkill et al. reported a mean diameter of 13 cm in their 116 cases of GIST. The margins of these tumours are well defined in about two-thirds of the cases.
Many of these tumours have an exophytic component as they arise from the muscularis propria. Marla et al.[6] found that all tumours in their study were predominantly exophytic, except for four cases where the primary tumour could not be categorized because of extensive metastatic spread.
They appear as exophytic, heterogeneous lesion with central non-enhancing necrotic areas within.
The enhancement pattern can vary from homogenously enhancing to heterogeneously enhancing, with or without ulceration. Lee et al. found GIST to be well-defined tumours with homogenous enhancement, while Levy et al., [7] found large heterogeneously enhancing masses due to areas of necrosis or cystic degeneration. They described ulceration as a common feature of GIST.
Metastases from GIST commonly occur to the liver and peritoneal cavity via hematogenous spread and peritoneal seeding. Occasionally, metastases occur to soft tissues, lungs, and pleura. Marla et al. also found that tumours that enhanced homogenously (nine out of 53 cases in their series) showed no metastases when they were followed for a mean period of 2.6 years as compared with those that enhanced heterogeneously. According to Nilsson et al., [8] at least 50% of these tumours have metastasis at presentation.
Treatment:
Surgical resection:
Imatinib is a new chemotherapeutic agent used in the treatment of GIST. It is a molecularly targeted tyrosine kinase receptor blocker. Response to imatinib is usually good, with improved long-term survival. The imaging features in patients showing response to imatinib include decrease in the density of the lesion, reduction in enhancement, and reduction in the number of nodules and number of vessels. The size of the lesion may increase or decrease. King et al. also demonstrated cystic degeneration and involution of hepatic metastases on treatment with imatinib