MdAkmat Ali 1, Richmond Ronald Gomes 2*, Farida Yeasmin 3
1Associate Professor, Department of Hepatology, Ad-din Women’s Medical College
2Associate Professor, Department of Medicine, Ad-din Women’s Medical College
3Assistant Professor, Department of Pathology.Ad-din Women’s Medical College
*Corresponding author: Richmond Ronald Gomes, Associate Professor, Medicine Ad-Din Women’s Medical College Hospital, Dhaka, Bangladesh; E-mail: rrichi.dmc.k56@gmail.
MdAkmat Ali 1, Richmond Ronald Gomes 2*, Farida Yeasmin 3
1Associate Professor, Department of Hepatology, Ad-din Women’s Medical College
2Associate Professor, Department of Medicine, Ad-din Women’s Medical College
3Assistant Professor, Department of Pathology.Ad-din Women’s Medical College
*Corresponding author: Richmond Ronald Gomes, Associate Professor, Medicine Ad-Din Women’s Medical College Hospital, Dhaka, Bangladesh; E-mail: rrichi.dmc.k56@gmail.
Received date: December 25, 2020; Accepted date: December 27, 2020; Published date: December 31, 2020
Citation: Richmond R Gomes., (2020) Demographic Profile and Pattern of Bilio-Pancreatic Malignancy by Ercp Among Bangladeshi Patients. Gastroenterology and Hepatology Research, 1(1); DOI: http;//doi.org/03.2020/1.1001
Copyright: © 2020 Richmond Ronald Gomes, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction: Outcome of most of the biliary and pancreatic malignancy is not good. Demography and involvement of different sites of these malignancies by ERCP are not widely studied in Bangladesh. We have studied ERCP based different biliary and pancreatic malignancy and their demographic characteristics.
Methods: Patients with radiological evidence of biliary tree dilatation along with CA 19.9 more than 400 unit /ml and strictures were confirmed with endoscopic retrograde cholangiopancreatography. History of biliary surgery or trauma, stone, ascariasis, pregnancy, extra pancreatobiliary abdominal tumour and HCC were excluded. The study was done from patients whose endoscopic retrograde cholagiopancreatography(ERCP) were performed from 2010 to 2015 at the Crescent Gastroliver Hospital in Dhaka, Bangladesh.
Results: Among 469patients, cholangiocarcinoma, ampullary carcinoma, carcinoma of gall bladder and carcinoma of head of pancreas were 246(52.7%), 133 (28.5%), 72 (15.4%) and 18 (3.9%) respectively. Mean age with range for cholangiocarcinoma were 54.5+13.9 (20-96) years, male was 137 (55.7%), female was 109 (44.3%). Mean age with range for ampullary carcinoma were 54.6+ 15.3 (20-90) years, male was 87(65.4%) and female was 46(34.6%). In Carcinoma of gall bladder mean age with range was 54.9+13.6 (30-80) years, male was 30(41.7%) and female was 42(58.3%), In carcinoma of head of pancreas mean age with range was 59.8+18.1 (29- 89) years, male was 11(61.1%) & female was 7(38.9%). Total upper, middle and lower common bile duct (CBD) stricture seen in 199(42.6%), 65(38.8%) and 206(44.1%) patients respectively with significant overlapping in between.
Conclusion: Cholangiocarcinoma was the commonest one. Stricture in the lower part of biliary tract was commonest. There was male predominance in all biliary carcinomas except carcinoma of gall bladder.
Introduction:
Among pancreatobiliary malignancy, cancer of the gallbladder, ampulla of Vater, extra hepatic bile duct cancer and carcinoma of head of the pancreas are relatively common.Most of them are associated with high mortality rate and the options of systemic therapy are very limited. Biliary obstruction due to malignancy may result bad outcome in spite of all available treatment. There is paucity of informations about prevalence of biliary tract malignancy and their radiological findings during ERCP in Bangladesh.
In the United States, biliary tract cancer is the sixth most common alimentary tract cancer, diagnosed less frequently than colorectal, pancreatic, liver, stomach, or esophageal cancers and accounting for only slightly more cases than small intestinal or anal cancer [1].
Cholangiocarcinoma is the most common biliary malignancy and the second most common hepatic malignancy after hepatocellular carcinoma (HCC) [2]. Cholangiocarcinoma accounts for 3% of all gastrointestinal tumors. Over the past 3 decades, the overall incidence of CCA appears to have increased. [3]
According to Randi G el al. and another study gallbladder cancer is one of the few cancers are observed more frequently among women than men; rates are higher among American Indians and Hispanic groups than others. [4, 5] About 90% of biliary tract cancer is not diagnosed until the disease became locally advanced or metastatic. [6]
Pancreatic tumors are the fifth most common cause of cancer-related mortality in the Western world. [7, 8] The most of them are located in the head; bile duct and duodenum are often affected for their anatomical proximity. Strictures of the biliary tract may occur at an early stage of the disease, patients present with jaundice and itching as a symptom; for these they seek for medical help. However, gastric outlet obstruction due to duodenal infiltration of the tumor is typically a late feature in an already advanced tumor stage. [9]
At the time of diagnosis up to 90% of patients with pancreatic tumors come with obstructive jaundice. Liver dysfunction and even hepatic failure may occur due to bile stasis and cholangitis. Cholangitis is more frequently found in patients with ampullary lesions than in patients with pancreatic cancer. Relief of the obstructive jaundice causes a dramatic increase in the quality of life of patients and should therefore always be accomplished. [10]
Neoplasms of the ampulla of Vater account for only 0.5% of all gastrointestinal malignancies. [11] Obstructive jaundice is the most common presenting symptom of ampullary cancer (85%) [12, 14]caused by compression of the distal bile duct by the tumor.
Materials and Methods:
A retrospective review of consecutive 469 patients who had undergone ERCP for biliopancreatic malignant strictures of different causes. The study was performed between January 2010 and December 2015 at the Crescent Gastroliver Hospital, Dhaka, Bangladesh, a specialized centre for Hepatobiliary endoscopic intervention. The informations about ERCP patients are retrieved from this hospital’s database including ERCP room computer. The institutional ethics committee approved this study. A search of the malignant biliopancreaticobstruction database was performed to identify all consecutive ERCP reports during the study period.The database included patient’s demographic data and USG,CT scan, MRCP and serum CA-19-9 reports.
Pathological characteristics
Biliopancreatic cancers were identified and sub-grouped as pancreatic, ampullary, biliary and gall bladder cancer to identify the proportions of each cancer during ERCP.
Statistical analysis:
Statistical methods used in this study are mostly limited to simple descriptive analysis were performed in SPSS version 20 .
Results:
Among 469patients,cholangiocarcinoma,ampullary carcinoma, carcinoma of gall bladder and carcinoma of head of pancreas were 246(52.7%), 133 (28.5%), 72 (15.4%) and 18 (3.9%) respectively. (Fig-1)
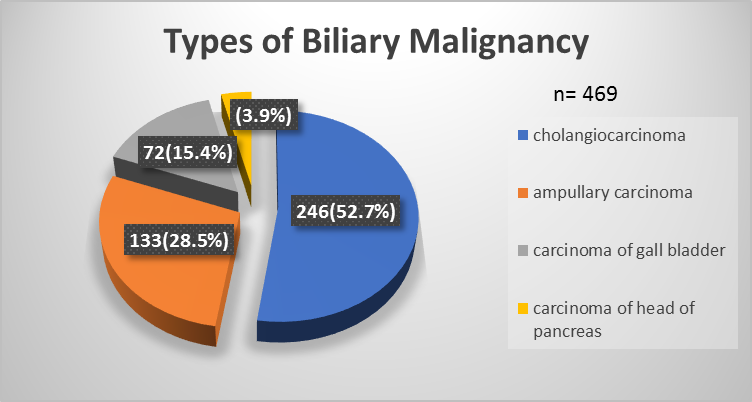
Figure 1: Types of Biliary Malignancy
Mean age with range for cholangiocarcinomawere 54.5+13.9 (20-96) years, male was 137 (55.7%), female was 109 (44.3%). Mean age with range for ampullary carcinoma were 54.6+ 15.3 (20-90) years, male was 87(65.4%) and female was 46(34.6%). In Carcinoma of gall bladdermean age with range was 54.9+13.6 (30-80) years, male was 30(41.7%) and female was 42(58.3%), In carcinoma of head of pancreas mean age with range was 59.8+18.1 (29- 89) years, male was 11(61.1%)&female was 7(38.9%).(Fig-2 and Fig-3)
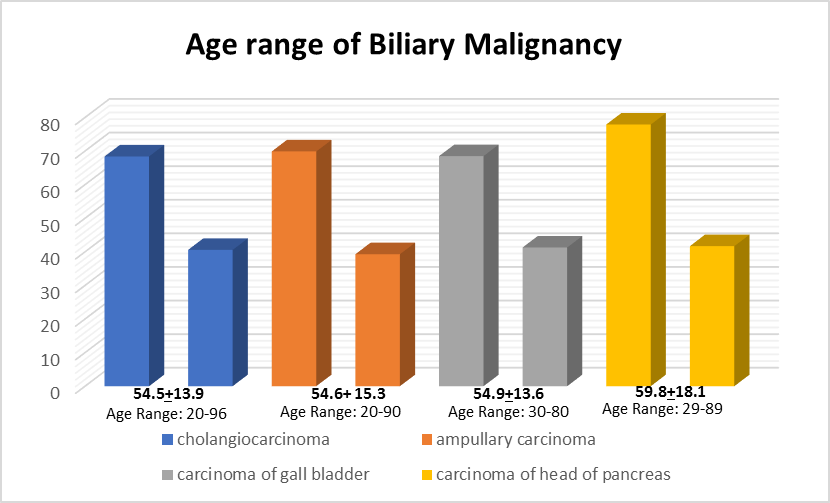
Figure 2: Age Range of Biliary Malignancy
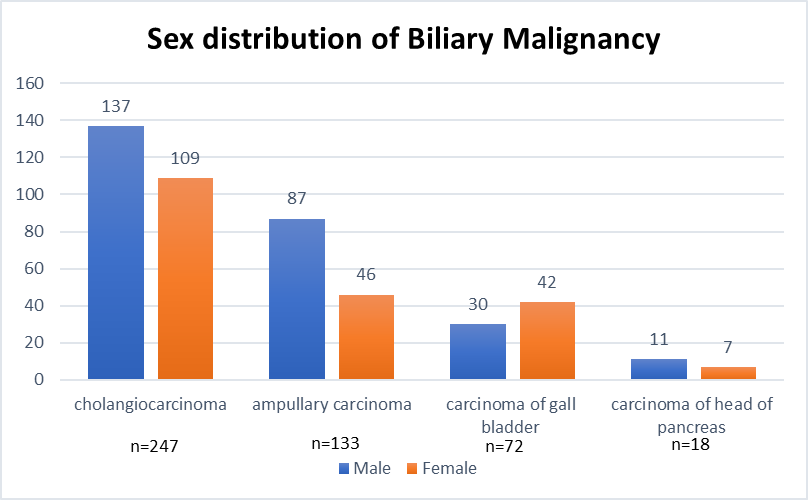
Figure 3: Sex distribution of Biliary Malignancy
Total upper, middle and lower common bile duct (CBD) stricture seen in 199(42.6%), 65(38.8%) and 206(44.1%) patients respectively with significant overlapping in between. (Fig-4)
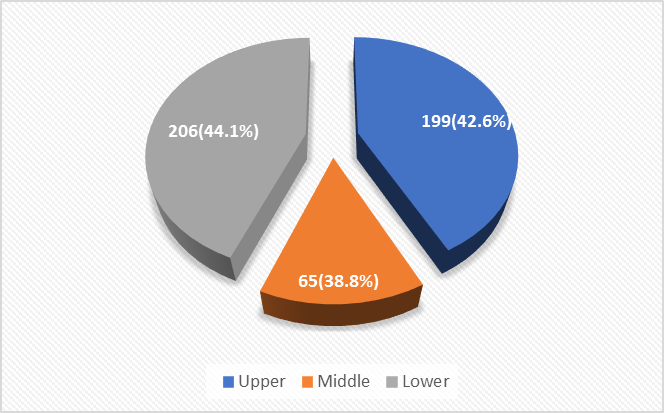
Figure 4: Percentage of different parts of CBD stricture(overlapping)
Discussion:
Geographic variation in the rates for extrahepatic bile duct cancer has been noted in the literature. [15, 17] In this study the most common pathology for which ERCP were performed was cholangiocarcinoma. But according to ChandrasegaramMD et all. the most common pathology for which a Pancreatoduodectomy was performed was pancreatic cancer 56%, followed by ampullary cancer 25%, biliary cancer 15% and duodenal cancer 4%.[18]
Felipe A et al. found during the 1992–2009 period 19,031 biliary tract cancers of gallbladder 41.3%, extrahepatic bile duct 32.9% and ampulla of Vater 19.8%.[19]
A recent large Chinese series by Chen et al. of 501 periampullary cancers found that ampullary carcinomas represented the majority of cancers with a value of 50%, followed by pancreatic cancer 34%, biliary cancer 10% and duodenal cancer 5%. [20] Gallbladder cancer rates were lowest among whites highest among American Indian/Alaska Natives. [19] However, many publications have continued to group these entities, which is dominated by gallbladder cancer in many but not all populations [4, 21, 22].
Ampulla of Vater cancer represents 20% of all biliary cancers in the US. A previous report found that rates for this cancer increased between 1973 and 2005 for all racial groups combined23. Primary ampullary tumors are rare, with an incidence of approximately four to six cases per million population [14, 24, 25]They account for only 6 percent of lesions that arise in the periampullary region [26]
Ampulla of Vater cancer represents 20% of all biliary cancers in the US. A previous report found that rates for this cancer increased between 1973 and 2005 for all racial groups combined [24].
Gallbladder cancer rates were lowest among whites and highest among American Indian/Alaska. Extrahepatic bile duct cancer rates also were lowest among whites and blacks and highest among American Indian/Alaska Natives- more than twice those among whites, The rates for ampulla of Vater were lowest among whites and blacks and highest among Hispanics followed by Asian. [19] For gallbladder cancer, there was a clear female predominance. In contrast, there was a male predominance for the two other specific anatomic sites. [19]
The major determinant of biliary tract cancer, especially gallbladder cancer, is a history gallstones [21, 27],as well as obesity and diabetes [28, 29].
Geographic variation in the rates for extrahepatic bile duct cancer has been noted in the literature [15, 17, 29] In a recent large three-decade study of 2,564 resected periampullary cancers, by He et al., the distribution of resected pancreatic, ampullary, biliary and duodenal carcinomas were 66%, 16%, 12%, and 6%, respectively [29]
Age:
With the exception of patients with primary sclerosingcholangitis (PSC), cholangiocarcinoma(CCA) is uncommon before age 40 years.According to a small scale study report median age of biliary malignancy at diagnosis was 62 years (range, 31-81 years),69% were intraheaticcholangiocarcinoma, 61% wasmale. [30] The average age at diagnosis of sporadic ampullary carcinomas is 60-70 years old [31, 34]
The median age of all the patients undergoing a Pancreaticoduodectomy for a cancer was 67 years. [18] Patients with pancreatic cancer had a median age of 64 years, those with ampullary cancer had a median age of 69 years, biliary cancer median age 66 years18;males 58% and females 42% aged between 26 and 86 years. [18]
Gall bladder carcinoma was diagnosed in patients with the mean age was 69.4 years. [35] Patient’s age with ampullary cancer in a study is slightly more than with pancreatic cancer,median age at diagnosis was 62 years. [18]
Gender:
Gallbladder cancer incidence was higher in females than in males, while extrahepatic bile duct and ampulla of Vater cancer incidence rates were higher in males. [19] Men have a slightly higher incidence of cholangiocarcinoma and mortality from the cancer than womenwhich were58% males and 42%females respectively. [36] A higher rate of ampullary cancer is observed in men. [24] A study report which was described by Chen Z et al. of gall bladder cancer, 70.0% were females and 30.0% were males. [37] Gall bladder cancer was diagnosed more in women than men in an another study where male female ratio was 1:1.14. [35]
Conclusion:
Biliary and pancreatic cancers often leading to distressing consequences including severe itching; ERCP often necessary to relieve symptoms.Sites of biliary strictures sometimes important for therapeutic ERCP and reconstructive surgery. This study report has bothsimilarities and dissimilarities with the previous studies and may be helpful for further multicenter study to assess the demographic changing pattern of biliary and pancreatic malignancy.