
Fairoz Abdul 1, Jawad Khan 1, Sunil James 1, Hui Ping Lee1, Mengshi Yuan 1, Ruwana Munasinghe 1,4, May Khei Hu 1, Abdel Yousif 1, Ahmed Hassan 1, Derek Connolly 1,2,3,
Vinoda Sharma 1,2*,
1Department of Cardiology, Birmingham City Hospital
2Institute of Cardiovascular Sciences, University of Birmingham
3Aston University, Birmingham
4 District General Hospital Monaragala, Sri Lanka
*Corresponding Author: Vinoda Sharma, Department of Cardiology, Birmingham City Hospital, B18 7QH.
Received date: March 27, 2023
Accepted date: May 24, 2023
published date: July 17, 2023
Citation: Abdul F, Khan J, James S, Hui P Lee, Yuan M. (2023) “High Risk Plaque (HRP) on Computed Tomography Coronary Angiography (CTCA) - does Gender Matter?.” J Clinical Cardiology Interventions, 3(1); DOI: http;//doi.org/10.2023/07.1034.
Copyright: © 2023 Vinoda Sharma. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background:
Computed tomography coronary angiogram (CTCA) provides diagnostic and prognostic information in coronary artery disease (CAD). Patients with high-risk plaque (HRP) on CTCA are more prone to cardiovascular events. While men are more likely to experience cardiovascular events than women, in the post-menopause, women tend to catch up. Therefore, our aim was to evaluate gender differences in HRP and outcomes, specifically examining whether women have higher or lower levels of HRP and whether this difference changes as women age.
Methods:
Retrospective analysis was conducted of stable patients who underwent CTCA from June 2018 to January 2020.
Results:
Of the 861 patients included, 41.5% (n=357) were female and mean age was 62.6 (±11.2) years. HRP was found in 59% of patients, and women had a lower prevalence of HRP compared to men (53.5% vs. 62.9%, p=0.006). However, among women over 55 years, HRP prevalence was similar to that of men (57.7% vs. 62.9%, p<0.001).
Revascularization was less frequent in women compared to men, even if they demonstrated HRP on CTCA (12.6% vs. 21.1%, p=0.01). The composite outcome of death and Acute Coronary Syndrome (ACS) was not statistically different between the two groups (Female: 2.3% vs. male: 3.6%, p=ns)
Conclusions:
HRP prevalence is lower in younger women compared to men, but this trend is reversed with increasing age. Early identification of HRP on CTCA could facilitate aggressive primary prevention to prevent adverse cardiovascular events.
Introduction:
Coronary artery disease (CAD) is the leading cause of death worldwide, accounting for more than nine million deaths annually (1). Diagnosis of stable CAD has shifted from exercise stress testing to direct imaging of the coronary tree anatomy using computed tomography coronary angiogram (CTCA). CTCA provides valuable diagnostic and prognostic information, accurately detecting and visualizing coronary atherosclerosis and providing information on plaque morphology, composition and characteristics (2, 3). CTCA is increasingly used in the diagnosis of stable CAD, and it compares favourably with intravascular ultrasound (IVUS), which has long been regarded as the gold-standard imaging tool of culprit and non-culprit plaques in the diagnosis of CAD and acute coronary syndrome (ACS) (2).
In recent years, the utility of CTCA has resulted in greater uptake of preventive measures among patients with CAD (4). The use of CTCA is recommended as the first-line imaging approach by the United Kingdom (UK) National Institute of Clinical Excellence (NICE) and European Society of Cardiology (ESC) chronic coronary syndrome guidelines. From an economic viewpoint, CTCA has been reported to save the National Health Service (NHS) of UK £16 million annually via effective triaging of patients and prompt exclusion of significant CAD (4).
High-risk coronary plaque morphology
While patients with significant obstructive CAD diagnosed by CTCA have a higher risk of major adverse cardiovascular events (MACEs), characterizing high-risk plaque (HRP) features and total plaque burden within the coronary arteries is becoming more important (5). It is increasingly observed that plaque rupture events can remain clinically silent and occur in patients with non-obstructive stenosis; hence the focus is gradually shifting away from assessing the severity of lumen stenosis towards identification and characterisation of high-risk plaque (HRP) features and total plaque burden within the coronary arteries (2).
Women typically have less plaque burden than men, and gender differences exist in the presentation and outcomes of stable CAD. (6-8). However, limited literature exists regarding the characterization of plaque and HRP in men versus women and its effect on outcomes. To address this gap, we aimed to evaluate gender differences in HRP and outcomes in stable patients who underwent CTCA.
Methods:
Study design
We retrospectively collected demographic, clinical, procedural and follow-up data for patients who underwent clinically indicated CTCA from the outpatient clinic and compared HRP between men and women. The study protocol was registered as a retrospective audit (#1768) and approved by our local governance body.
Patient selection
2205 patients who were referred for CTCA in June 2018 to January 2020 in Sandwell and West Birmingham Hospitals NHS Trust were retrospectively identified (Figure 1). We excluded non-rapid access chest pain clinic (RACPC) referrals, duplicate records, patients whose CTCA images were unable to be extracted from the archive, patients with previous CABG, normal coronaries or minimal CAD (as defined by the Coronary Artery Disease - Reporting and Data System (CAD-RADS) 1=1-24% coronary stenosis), (9) and degraded images.
CTCA protocol
Baseline observations were performed, including heart rate and blood pressure, as part of the CTCA checklist. A venous cannula (minimum 18G) was preferably inserted in the ante-cubital fossa of patients and standard ECG leads were placed. After confirmatory checks, the patients were given sublingual glyceryl trinitrate (GTN) spray (400 μg) or GTN tablet (500 μg) and intravenous metoprolol (maximum 50 mg). Breath holding was practiced.
Patients underwent prospective, gated CTCA with a 128-slice dual source CT (DSCT) scanner (Somatom Definition Flash, Siemens Medical Solutions, Forchheim, Germany). Based on the patient’s body mass index (BMI), the tube voltage (<25 kg/m2 : 100 kV, ≥25 kg/m2 : 120 kV) and current were adjusted. When a standard adapt (sequential scan) was performed, single source 128 x 0.6 mm acquisition was utilised with a rotation time of 0.28 seconds. This was performed at 70% of the standard cardiac cycle. The systolic scan (also an adapt scan) had additional padding and was performed at 250-350 ms of the cardiac cycle.
The contrast bolus (at a rate of 4.5mL/s with a high-pressure injector) for the main scan was as follow:
An automated multi-lingual voice recording was incorporated to instruct breath holding during the scan. Imaging was performed from 2 cm below the tracheal bifurcation to the level of the diaphragm in a cranio-caudal manner. The data was rebuilt, including post-processing for maximum intensity projection (MIP), multi-planar reformation (MPR), as well as volume rendering, and transferred automatically to the workstation (syngo.via, Siemens Healthineers, Erlangen, Germany).
Assessment of CTCA images
CTCA images were analysed by operators with level 2 CTCA accreditation and had at least one year of experience in reporting CTCA images. The presence or absence of three HRP features was assessed: positive remodelling (PR), napkin-ring sign (NRS) and spotty calcification (Appendix Figures 1-3). PR was defined by remodelling index (RI) of ≥ 1.1, which was calculated by the vessel size at the site of the maximal remodelling divided by vessel size of the reference site. NRS was defined as a central area of low attenuation surrounded by peripheral area with high attenuation. Spotty calcification was defined as focal areas of calcification within the coronary artery wall < 3mm in maximum diameter. Low attenuation plaque was not included due to inconsistent observer reproducibility.
Figure 1: Patient selection
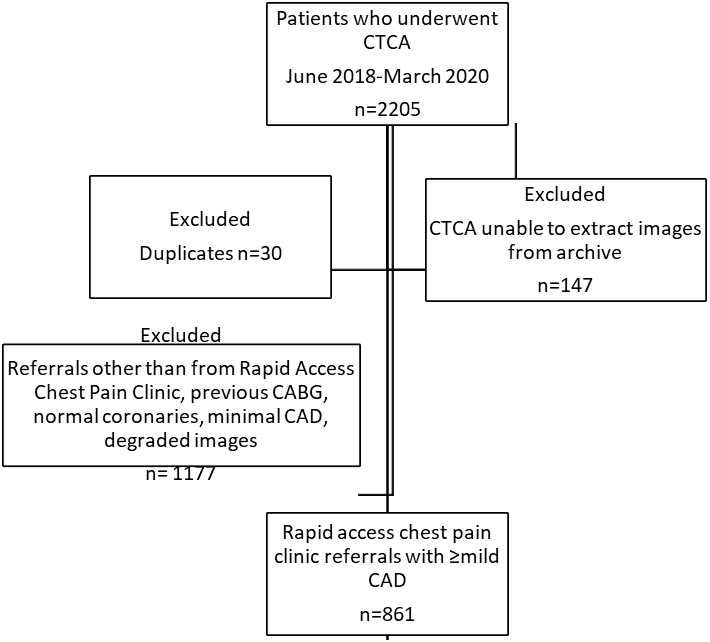
Figure 2: Invasive coronary angiography in female versus male patients
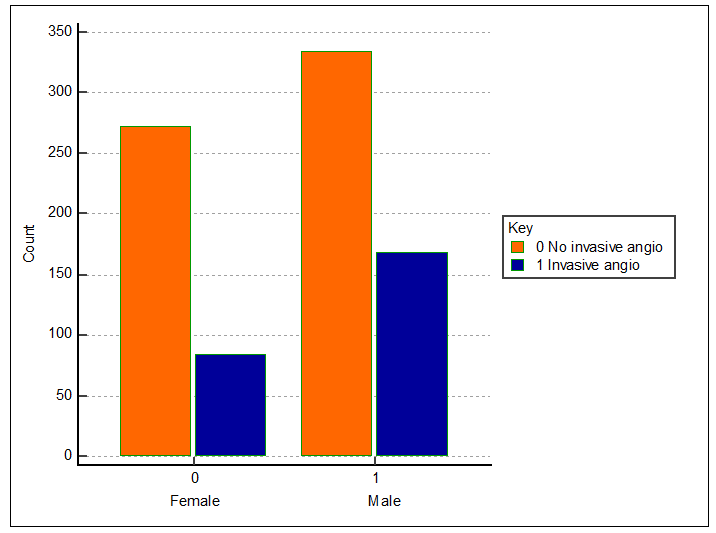
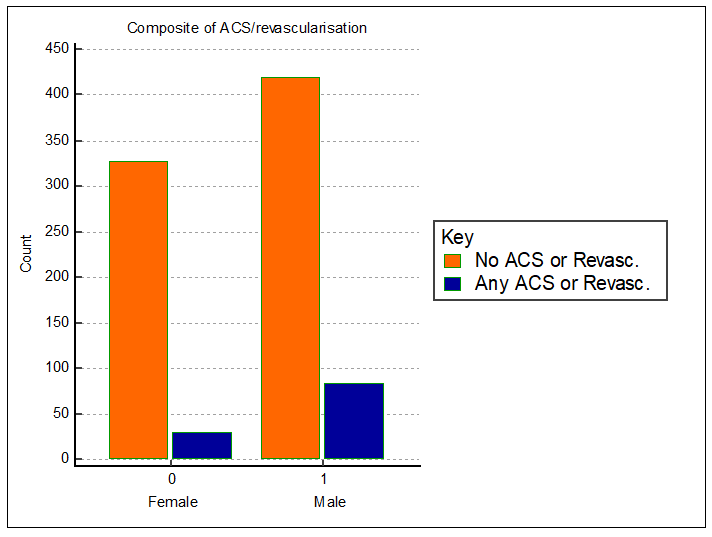
Figure 3: ACS or revascularisation in female versus male patients
Statistical analysis
Statistical analysis was performed using MedCalc® (MedCalc Software Ltd, Ostend, Belgium).
We compared the following groups of patients for demographics, HRP morphology and composite outcome of all-cause mortality and ACS:
i) female and male patients
ii) female patients >55 years and ≤55 years
Continuous variables were presented as mean ± standard deviation and categorical variables were presented as percentages. Continuous variables were compared using student’s unpaired t-test or ANOVA, while categorical variables were compared using chi-squared or Fisher’s exact tests. A p-value of 0.05 was considered significant. Modelling by binary regression analysis was performed to assess predictors of HRP after identifying significant independent variables.
Interobserver variability for the analysis of HRP (per coronary artery and per type of HRP) was assessed by Cohen’s kappa (κ value).
Results:
A total of 861 patients were included in our study of whom 41.5% were female (n=357), the majority being > 55 years of age (76.2%, n=272). Mean age was 62.6 (±11.2) years and 33.7% had diabetes mellitus (DM, n=290).
Compared to their male counterparts, female patients were older, with higher body mass index (BMI) but less likely to be smokers (table 1). Other demographics were no different between the two groups.
Table 1: Baseline characteristics and laboratory data of all patients
|
Variable |
Total n=861 (%) |
Female n=357(41.5%) |
Male n=504(58.5%) |
p-value |
|
Age, in years |
62.6 (±11.2) |
63.6 (±11) |
61.9 (±11.3) |
p=0.03* |
|
South Asian ethnicity |
327 (38.6) |
138 (39.2) |
189 (38.1) |
p=0.75 |
|
HTN |
499 (58.0) |
198 (55.5) |
301 (59.7) |
p=0.21 |
|
DM |
290 (33.7) |
127 (35.6) |
163 (32.3) |
p=0.32 |
|
HbA1c value, mmol/mol+ |
45.9 (±12.6) |
46.3 (±13.1) |
45.6 (±12.3) |
p=0.90 |
|
Hypercholesterolemia |
490 (56.9) |
204 (57.1) |
286 (56.7) |
p=0.91 |
|
Total cholesterol value, mmol/L+ |
4.50 (1.2) |
4.76 (±1.2) |
4.42 (±1.2) |
p<0.001* |
|
BMI, kg/m2+ |
29.9 (±6.4) |
30.7 (±7.0) |
29.3 (±5.8) |
p=0.016* |
|
Smoker+ |
306 (46.6) |
98 (37.0) |
208 (53.2) |
p<0.0001* |
|
Family History of CAD+ |
285 (52.6) |
120 (54.1) |
165 (51.6) |
p=0.57 |
|
Previous MI |
38 (4.4) |
9 (2.5) |
29 (5.8) |
p=0.02* |
|
Previous PCI |
34 (4.0) |
10 (2.8) |
24 (4.8) |
p=0.15 |
|
Lipid therapy prior to CTCA |
549 (63.8) |
216 (60.5) |
333 (66.1) |
p=0.09 |
|
Lipid therapy after CTCA
|
542 (98.7)
7 (1.3) |
212 (98.1)
4 (1.9) |
330 (99.1)
3 (0.9) |
p=0.49
|
|
Aspirin prior to CTCA+ |
283 (33.7) |
101 (29.1) |
182 (37.0) |
p=0.017* |
|
Aspirin after CTCA
|
446 (52.5) 50 (5.9)
|
170 (48.0) 19 (5.4)
|
276 (55.6) 31 (6.2)
|
p=0.05
|
Continuous data are presented as mean ± standard deviation and categorical data are presented as number and percentages.
+Not all patient data were available.
More than half the cohort (n=508, 59%) had features of HRP on their CTCA images. Spotty calcification was the commonest HRP detected on CTCA followed by positive remodelling (table 2).
Overall, female patients were less likely to have HRP as well as less total plaque burden compared to male patients (table 2).
With increasing age, although female patients had similar HRP to the male patients (females >55 years: 57.7% vs. males: 62.9%, p<0.001), their burden of HRP was higher than in than younger females (HRP: females >55 years: 57.7% vs female ≤55: 40.0%, p=0.004, table 3) (>1 type of HRP: 19.5% vs. 10.1%, p=0.013, table 3).
Table 3: Comparison of plaque characteristics and outcomes in women >55 years versus ≤55 years
|
Variable |
Total n=357 (100%) |
Female>55 years n=272 (76.2%) |
Female ≤55 years n=85 (23.8%) |
p value |
|
Age in years |
63.6 (±11) |
68.1 (±7.9) |
49.2 (±5.6) |
p<0.001* |
|
HRP present |
191 (53.5) |
157 (57.7) |
34 (40.0) |
p=0.004* |
|
Plaque present ≥ 50% vessel length |
79 (22.1) |
68 (25) |
11 (12.9) |
p=0.02 |
|
> 1 type of HRP |
62 (17.4) |
53 (19.5) |
9 (10.6) |
p=0.013* |
|
HRP morphology i) Only one type of HRP
ii) >1 types of HRP |
164 (45.9) 83 (23.2) 10 (2.8) 62 (17.4) |
137 (50.4) 69 (25.4) 8 (2.9) 53 (19.5) |
27 (31.8) 14 (16.5) 2 (2.4) 9 (10.6) |
p=0.003 p=0.16 p=1.00 p=0.013* |
|
Multivessel HRP |
70 (19.6) |
62 (22.8) |
8 (9.4) |
p=0.007* |
|
Angiography |
85 (23.8) |
66 (24.3) |
19 (22.6) |
p=0.82 |
|
Revascularisation performed (PCI or CABG) |
35 (9.8) |
30 (11.0) |
5 (5.9) |
p=0.16 |
|
Composite outcome (death and ACS) |
8 (2.2) |
8 (2.9%) |
0 (0) |
p=0.11 |
Categorical data are presented as number and percentages.
Abbreviations - ACS: acute coronary syndrome; CABG: coronary artery bypass graft; CTCA: computed tomography coronary angiogram; HRP: high-risk plaque; PCI: percutaneous coronary intervention.
Revascularisation was less frequent in female compared to male patients (Revascularisation female 9.8% vs 19.8%, p=0.0001) even if they demonstrated HRP on CTCA (Revascularisation female 12.6% vs. revascularisation male 21.1%, p=0.01) or had plaque burden >50% (High plaque burden revascularisation female: 26.6% vs. high plaque burden revascularisation male: 42.3%, p=0.02). The overall incidence of ACS was low (0.7%), nevertheless, the presence of more than one type of HRP was associated with occurrence of an ACS in both men as well as women (men: 3.2% vs. women 3.1%), occurring solely in women>55 years of age. All patients who developed an ACS had both calcium nodule and positive remodelling as the HRP morphology.
The composite outcome of death and ACS was not different between the groups (table 2).
Table 2: Comparison of plaque characteristics and outcomes in female versus male patients
|
Variable |
Total n=861 |
Female n=357(41.5%) |
Male n=504(58.5%) |
p value |
|
HRP present |
508 (59) |
191 (53.5) |
317 (62.9) |
p=0.006* |
|
Plaque present ≥ 50% vessel length |
242 (28.1) |
79 (22.1) |
163 (32.3) |
p=0.001* |
|
HRP morphology i) Only one type of HRP
ii) >1 types of HRP |
429 (49.8) 241 (28.0) 47 (5.5) 191 (22.2) |
164 (45.9) 83 (23.2) 10 (2.8) 62 (17.4) |
265 (52.6) 158 (31.3) 37 (7.3) 129 (25.6) |
p=0.06 p=0.009* p=0.004* p=0.004* |
|
HRP in LAD / LMS artery:
|
163 (18.9) 193 (22.4) 22 (2.6) |
55 (15.4) 67 (18.8) 5 (1.4) |
108 (21.4) 123 (24.4) 17 (3.4) |
p=0.03* p=0.06 p=0.08 |
|
Multi-vessel HRP |
205 (23.8) |
70 (19.6) |
135 (26.8) |
p=0.015* |
|
Angiography performed |
253 (29.4) |
84 (23.5) |
169 (33.5) |
p=0.002* |
|
Revascularisation performed (PCI or CABG) |
135 (15.7%) |
35 (9.8) |
100 (19.8) |
p=0.0001* |
|
Readmitted with ACS |
6 (0.7%) |
2 (0.6%) |
4 (0.8%) |
p=0.68 |
|
All-cause mortality |
20 (2.3%) |
6 (1.7%) |
14 (2.8%) |
p=0.29 |
Categorical data are presented as number and percentages.
Abbreviations - ACS: acute coronary syndrome; CABG: coronary artery bypass graft; CTCA: computed tomography coronary angiogram; HRP: high-risk plaque; LAD: left anterior descending artery; LMS: left main stem artery; PCI: percutaneous coronary intervention.
Binary regression analysis demonstrated that increased plaque burden and age were independent predictors of HRP; female gender was negatively associated with HRP (figure 4, table 4).
Figure 4: Predictors of High-risk Plaque
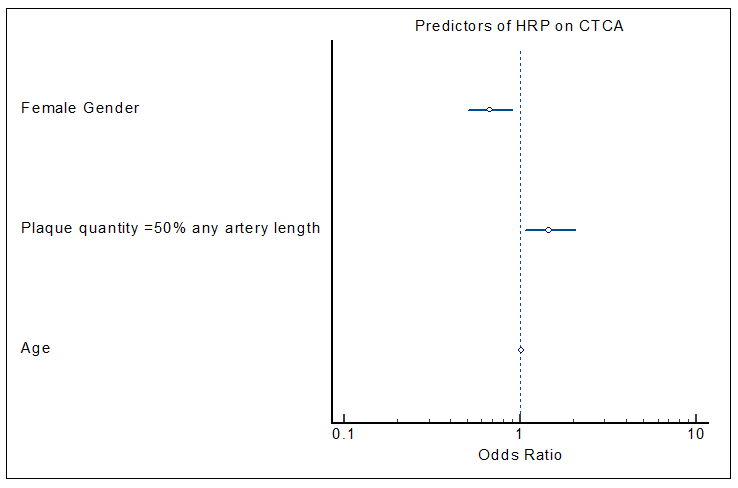
Table 4: Predictors of HRP
|
Covariate |
OR |
95% CI |
p-value |
|
Plaque present in ≥50% of any artery |
1.47 |
1.07 - 2.03 |
p = 0.019 |
|
Female gender |
0.67 |
0.51 - 0.89 |
p = 0.006 |
|
Age |
1.02 |
1.01 - 1.04 |
p <0.001 |
Abbreviations – CI: confidence interval; OR: odds ratio; HRP: high-risk plaque.
Inter-observer variability was performed for 10% of the dataset (n=86) and was as follow: calcium nodule: kappa = 0.5 (moderate), positive remodelling: kappa = 0.4 (fair), NRS: kappa = 0.15 (slight).
Discussion:
This retrospective observational study demonstrated that in a stable chest pain population, female patients were less likely to have HRP on CTCA compared to male patients. However, with increasing age, female patients had similar HRP burden to male patients. Patients with more than one type of HRP were more likely to have an ACS.
Women manifest CAD at least a decade later than men (10, 11), in part due to the protective, regulatory effects of oestrogen on lipids, metabolism and inflammation in the pre-menopausal phase. As observed in the CLARIFY registry (ProspeCtive observational LongitudinAl RegIstry oF patients with stable coronary arterY disease), women with stable CAD were older with more cardiovascular risk factors (6). Transition to menopause, which usually occurs between 45 and 55 years of age (12), increases the cardiovascular risk profile of women (13). Only 5% of women will have a late menopause after 55 years of age (12) - hence we chose the cut-off of 55 years to compare older and younger women.
Why is it important to characterise high risk plaque morphology in female patients? Would not just identifying cardiovascular risk factors be adequate? Yu et al defined female specific risk factors associated with age in a comprehensive review (14). They concluded that plaque erosion was more frequent in younger women who smoked and plaque rupture in older women with hypercholesterolemia. Burke et al (11) summarised that older post-menopausal women have an increased number of vulnerable plaques and hence develop plaque rupture in contrast to younger women who mainly present with plaque erosion. Addressing risk factors after the occurrence of a cardiovascular event is akin to shutting the stable door after the horse has bolted. It would be preferable to be able to non-invasively identify lesions at risk and initiate aggressive primary prevention measures. CTCA addresses this objective extremely well with identification of HRP.
HRP is known to predict long term adverse events even in the absence of coronary stenosis (15). In the Rule Out Myocardial Infarction/Ischemia Using Computer-Assisted Tomography II (ROMICAT II) trial, Puchner et al demonstrated that HRP was more frequent in patients presenting with ACS and was an independent predictor of ACS (OR: 38.6; 95% CI: 14.2 to 104.7; p < 0.001), even when adjusted for coronary stenosis ≥50% (16). Our study has reiterated these findings.
What about HRP in women? Ferencik et al assessed the effect of HRP on major adverse cardiovascular events (MACE) in 4415 stable patients in the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial (17). They concluded that HRP was a stronger predictor of MACE in women (aHR, 2.41; 95% CI, 1.25-4.64) compared to men (aHR, 1.40; 95% CI, 0.81-2.39)(17). Women are known to have smaller diameter coronary arteries and it is possible that any plaque rupture due to HRP will lead to resultant occlusive coronary event (17, 18).
The commonest HRP feature in both male and female patients in our analysis was spotty calcification. Acute plaque rupture is known to occur in areas of mild or speckled calcification (19, 20) and spotty calcification correlates with high risk vulnerable plaque on intracoronary imaging with IntraVascular UltraSound (IVUS) (19). The second most frequent HRP observed in our analysis was positive remodelling (PR) which is known to contribute to ACS as plaque accumulation near sites of PR are prone to plaque rupture (21). Hu et al have demonstrated the prognostic value of identifying PR on CTCA (22). We observed that the two female patients who developed an ACS were older (>55 years) with two types of HRP: spotty calcification as well as PR. Similarly, the four male patients who developed ACS also demonstrated both spotty calcification and PR on CTCA. It is hence important to identify patterns of HRP which have the potential to cause unstable clinical presentations as it introduces the opportunity to aggressively intervene in these patients both with medications (e.g. statins) as well as lifestyle change.
The vast majority of both women and men were commenced on high potency statins and a smaller number on aspirin after the CTCA. In high risk patients with non-obstructive CAD on CTCA, Hwang et al demonstrated that aspirin was associated with lower all-cause mortality (adjusted HR 0.649; 95% CI 0.492-0.857; p = 0.0023)(23). We recommend that it would be reasonable to commence patients with HRP on CTCA on high potency statin and other lipid lowering agents along with aspirin especially in the presence of more than one type of HRP.
Gender differences are well identified in the management of stable angina in women compared to men, including the reduced incidence of invasive angiography and revascularisation (24, 25). This corroborates with our finding that invasive coronary angiography and revascularisation occurred less frequently in women despite the presence of HRP and/or increased plaque burden compared to male patients. This could be due to multiple factors including patient’s reluctance to undergo an invasive procedure, interaction of the physician with the patient or atypical symptoms seen more frequently in female patients (25, 26).
Limitations:
Our study has a number of potential limitations. This is a single centre study and the observations may reflect findings in a select cohort which may not be applicable to the larger, general population. Secondly, images were interpreted without the presence of a core lab or utilisation of AI/automated software- this can introduce a degree of bias although the inter-observer variability was acceptable. Thirdly, the reasons for invasive angiography or revascularisation were not available- for example, no details of symptoms or anti-anginal medications were available.
Conclusions:
HRP is less frequently present on CTCA in women compared to men but with increasing age, women have similar HRP as their male counterparts. Early identification of HRP on CTCA coupled with aggressive primary prevention could potentially prevent adverse cardiovascular events. Although this study is one of the first to identify the differences in HRP on CTCA between female and male patients, larger prospective multi-centre trials are needed to confirm these findings.
Acknowledgement:
We have utilised the software CHAT GPT to assist in restructuring and reformatting.
We are grateful to Philip Spencer#, radiographer for assistance with the CTCA protocol.