Clinical Cardiology Interventions
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-077X | Journal DOI: 10.61148/2836-077X/JCCI
Bruce Murphy, M.D1, PhD., Peyton Card, M.D1, Leybi Ramirez-Kelly, M.D1*, and Amanda Xaysuda, M.P.H 1, R. Eric Heidel, Ph.D 2
1Arkansas Heart Hospital
2University of Tennessee Graduate School of Medicine
*Corresponding Author: Leybi Ramirez-Kelly, Arkansas Heart Hospital United States.
Received date: July 11, 2022
Accepted date: September 19, 2022
published date: December 22, 2022
Citation: Murphy B, Card P, Ramirez-Kelly L, and Xaysuda A, R. Eric Heidel, (2022) “Effects of the Strong Hearts Program After a Major Cardiovascular Event in Patients with Cardiovascular Disease.” J Clinical Cardiology Interventions, 2(5); DOI: http;//doi.org/12.2022/1.1025
Copyright: © 2022: Leybi Ramirez-Kelly. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
This prospective, non-randomized study evaluated the effectiveness of a 9-week structured outpatient cardiac rehabilitation program at the Arkansas Heart Hospital’s Strong Hearts Rehabilitation Center. Paired t-tests were used to compare baseline values to those at program completion. Participants showed statistically significant measured improvements at program completion in weight (p-value <0.001), body mass index (<0.001), total fat mass (<0.001), waist circumference (<0.001), HDL (0.02), triglycerides (0.01), Vitamin D (<0.001), systolic blood pressure (<0.001), diastolic blood pressure (0.002), and functional capacity (<0.001). Participants also showed statistically significant improvements in self-reported physical activity (<0.001), nutrition (<0.001), depression (0.044), and quality of life (<0.001). The 9-week structured program resulted in significant cardiovascular benefit to patients with cardiovascular disease by reducing cardiac risk factors, increasing exercise capacity, and improving quality of life.
Introduction
Cardiovascular diseases (CVD) are the leading cause of mortality and remain the leading cause of disease burden in the world (Roth, 2020). In the United States, over 126 million adults suffer from at least one form of CVD or its complications (Virani, 2021). Of these, an estimated 1.3 million patients with heart disease (Turk, 2019) and more than 650,000 patients with Congestive Heart Failure (CHF), are candidates for cardiac rehabilitation (CR) each year (Roger, 2013).
CR is a multidisciplinary intervention with class 1a recommendation from the American Heart Association and American College of Cardiology following acute myocardial infarction (MI), coronary surgery or intervention, stable angina, and class 2a recommendation for CHF. It is well demonstrated that CR participation positively affects risk factors for heart disease (Kotseva, 2012) and improves health-related quality of life (QOL) (Williams, 2006). CR is linked to an increase in exercise capacity (Franklin, 2013) and ability to perform activities of daily living (ADLs) (Johnston, 2011). Patients who participate in CR are more likely to adhere to medications (Thomas, 2010) and less likely to be readmitted to the hospital (Dunlay, 2014). A meta-analysis of over 8,000 patients from 48 randomized controlled trials showed a reduction in overall mortality of 20% and cardiac mortality of 26% over a 3-year period following CR (Taylor, 2004). The NICE guidelines for the management of secondary prevention following MI states that the implementation of CR should be a key priority (NICE, 2007).
There is wide variability in CR programming though most programs center around medically supervised exercise and provide patient education designed to improve CV health and functional capacity. CMS guidelines limit traditional CR to 36 sessions within 36 weeks. According to Mirman et al. (2020), due to time and insurance coverage constraints, traditional programs dedicate most of the effort to aerobic exercise rather than education or behavior modification. Intensive cardiac rehab (ICR) is more rigorous, offering up to six sessions per day for a total of 72 sessions over 18-weeks (AACVPR, 2013). ICR was developed to enhance traditional CR by adding sessions focused on nutrition, lifestyle behaviors, and stress management (Husaini, 2021). ICR programs must be approved by CMS and must show through peer-reviewed research that they positively affect the progression of heart disease, reduce the need for CABG, and reduce the need for PCI. ICR programs must also demonstrate a statistically significant reduction in five or more of the following outcome measures when compared to baseline: (1) LDL; (2) triglycerides; (3) BMI; (4) systolic blood pressure (SBP); (5) diastolic blood pressure (DBP); and (6) the need for cholesterol, blood pressure, and diabetes medications. Currently there are only three ICR programs recognized and certified by CMS.
Despite proven benefits, the utilization of CR is suboptimal (Servey, et al). Today, over 20 million patients eligible for CR have never participated in a program (Viriani, 2021). Results from a national sample of Medicare patients between 2012-2016 showed that only 16.2% of qualifying patients participated in traditional CR and only 0.1% in ICR (Husaini, 2021). Barriers to utilization include factors related to cost, transportation, and program availability. Additional options for ICR programming should be considered as a way to increase overall capacity for and utilization of CR.
The purpose of this study was to evaluate the effectiveness of the Strong Hearts (SH) program on CVD-related outcomes and progression of disease in the CVD patient in relation to CMS requirements for ICR programming. The SH program is a 9-week structured outpatient CR program consisting of two sessions per day, one exercise and one education, four times per week for a total of 72 sessions. The program takes a patient-focused approach to medical nutrition, hands-on education, and functional exercise therapy.
Methods
One hundred ninety-eight participants (n=198) were enrolled in the study in 2020 and 2021. The study took place at a Strong Hearts Rehabilitation Center (Center) in central Arkansas. The protocol was approved by Western IRB and written informed consent was obtained from all participants prior to participation.
Participants were referred to the program by a licensed physician. Referring physicians acknowledged that CR with supervised exercise training would be a viable post-event intervention. Referrals came from Arkansas Heart Hospital, Arkansas Heart Hospital Clinics, and from outside community referrals.
Participants were eligible for the program if they were referred following a major CV event, which was defined as any of the following: (1). acute MI within the preceding 12 months; (2). current stable or unstable angina pectoris; (3). heart valve repair or replacement; (4). PCIs; (5). heart transplant; (6). CHF with reduced or preserved ejection fraction; or (7). other cardiac-related postprocedural states.
Patients were excluded if they met any of the following: (1). renal or hepatic dysfunction; (2). current chemo/radiation treatment; (3). malnourishment or BMI < 18; (4). history of HIV/AIDS-related complex or active HIV infection; (5). post-bariatric surgery; (6). history of substance abuse; (7). gastrointestinal disorders which impair absorption; (8). patients taking warfarin/coumadin; (9). CHF if on fluid restrictions; (10). A1C > 10; (11). cognitive deficits that would preclude exercise therapy; or (12). physical limitations that would contraindicate exercise therapy.
Program Design
Participants were asked to attend the center four days per week for 9-weeks. Each day consisted of two sessions: one session of live education and one session of exercise for a total of 72 total sessions. An initial treatment plan (ITP) was developed for each participant according to AACVPR guidelines and was signed by a physician at the first session. Outcomes measures were recorded at program start, program discharge, and 12-months (ongoing).
Outcomes Measures
Anthropometric measurements, including height, weight, and waist circumference were measured using standard scales. BMI was calculated using measured height and weight (BMI = kg/m2). Exercise capacity is reported in METS and was measured via 6MWT, Treadmill, or Nu-Step submaximal test protocols. Fasting blood draw was used to measure total cholesterol, HDL, LDL, triglycerides, A1c, and Vitamin D. Fat mass and Lean mass were measured using iDXA scan. Self-reported measures were captured through questionnaires including Dartmouth COOP to measure quality of life (Trustees of Dartmouth College, COOP Project, 2009), Cardiac Depression Scale to measure depression (D.L.Hare, 1996), Duke Activity Status Index to measure activity (Hlatky and colleagues, 1989), and Rate Your Plate to measure nutrition (Brown University, 2005). Satisfaction surveys were provided to patients at program completion.
Exercise Intervention
Patients were asked to complete four exercise sessions each week. During each exercise session, heart rate and cardiac rhythm was monitored via 3-lead cardiac telemetry (Life Systems International, 2021), as well as blood pressure and blood glucose levels measured periodically. All exercise sessions were personalized to the patient and were performed in accordance with the guidelines and recommendations set forth by the American College of Sports Medicine (ACSM, 2018). Target heart rate was calculated at 40% - 70% of maximal heart rate. Exercise sessions began with a 5 – 10-minute warm-up and ended with a 5 – 10-minute cool-down.
Patients were asked to participate in aerobic conditioning each of the four days. Initially the aerobic exercise training zone was set between 10 and 40 minutes in duration and at an exertion level of 11-14 on the Rate of Perceived Exertion Scale (RPE). Exercise prescription progression to moderate or high-intensity exercise was dictated by each patient’s current level of conditioning, tolerance for exercise, and symptom-limited parameters. Aerobic training was allowed to increase up to 85% of maximal aerobic capacity.
Strength training was conducted in the form of chair exercises, exercise bands, free weights, and bodyweight exercises. Patients were asked to participate in strength training 2 - 3 days per week. Initial resistance training was conducted at 30-60% of 1 RM with 10-15 repetitions and 11-14 RPE. Training was allowed to progress to 60-80% of 1 RM, 1-4 sets, 8-12 repetitions, and 8-10 exercises.
Patients were encouraged to participate in modified yoga 1 - 2 days per week. Yoga sessions focused on flexibility, balance, range of motion, posture, deep breathing, and relaxation.
A low-intensity home exercise program was provided for patients on days when they were not at the SH center for sessions. Home exercise was highly encouraged to promote healthy lifestyle change and further progression of goals and quality of life.
Nutrition Intervention
The nutrition component of the program consisted of a structured Mediterranean diet with base percentages of 25% protein, 30% fat and 45% carbohydrate. This diet was prepared in our Strong Heart Kitchen by a certified chef. Patients were provided with the meals at the end of the last session of the week. Caloric needs were adjusted for each patient using the Mifflin-St. Jeor equation. Nutrition recommendations were communicated to the patient during 1-on-1 Registered Dietitian consults. Educational workshops supported these recommendations.
Education
Participants were asked to attend an education session four times per week during the program. Education was delivered through live workshops taught by Registered Dietitians, Registered Nurses, Exercise Physiologists and Mental Health Experts. A 9-week workshop schedule was followed to ensure every patient received the same information.
Statistical Analysis
The clinical parameters of interest were assessed for change across time using repeated-measures t-test. Means and standard deviations were reported and interpreted for each observation in the within-subject’s analyses. Statistical significance was assumed at a two-sided alpha value of 0.05 and the statistics were performed using SPSS Version 28 (Armonk, NY: IBM Corp.).
Results
Of the 198 participants who enrolled, 50 patients withdrew from the study, 13 did not complete all sessions within 9-weeks, and 7 were lost to follow-up. This resulted in n=128. Of this 45 were female and 83 were male. The mean age was 65. Qualifying diagnoses were PCI (60), CABG (33), Angina (24), Valve repair or replacement (5), CHF (3), and Other Postprocedural States (3).
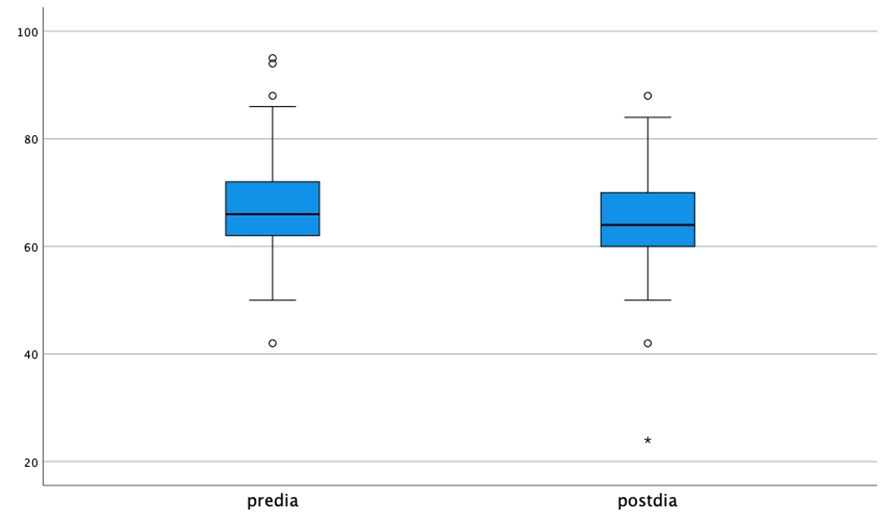
After implementation of the intervention, statistically significant decreases in weight (p < 0.001), BMI (< 0.001), waist circumference (< 0.001), triglycerides (0.01), SBP (< 0.001), DBP (0.002), total fat mass (< 0.001), Dartmouth quality of life scores (< 0.001), and cardiac depression scores (0.044) were detected. In other instances, there were statistically significant increases across time for the clinical parameters of HDL (0.02), Vitamin D (0.001), METS (< 0.001), Duke activity scores (< 0.001), and Rate Your Plate nutrition scores (< 0.001). There were no significant changes across time for total cholesterol (0.17), LDL (0.21), A1c (0.27), or DXA total lean mass (0.86). See Table 1 for all the means, standard deviations, and p-values associated with these analyses. See Figures 1-5 for boxplots of certain comparisons.
By program completion, five patients had discontinued cholesterol medication completely, two had reduced cholesterol medication, four had stopped blood pressure medication, and one patient reduced diabetes medication. At program completion, 94% of participants scored their satisfaction with the program as a 5 = highly satisfied.
Table 1.
|
Variable |
Pre-intervention |
Post-intervention |
p-value |
|
Weight |
208.4 (42.7) |
204.0 (42.1) |
< 0.001 |
|
BMI |
31.8 (5.7) |
31.0 (5.5) |
< 0.001 |
|
Waist circumference |
45.3 (5.9) |
43.7 (5.8) |
< 0.001 |
|
Total cholesterol |
153.9 (53.9) |
146.3 (53.4) |
0.016 |
|
Triglycerides |
139.3 (94.3) |
115.1 (77.6) |
< 0.001 |
|
HDL |
45.0 (13.2) |
46.7 (13.2) |
0.029 |
|
LDL |
86.6 (44.3) |
80.1 (39.9) |
0.013 |
|
A1c |
6.3 (1.0) |
6.2 (1.0) |
0.039 |
|
Vitamin D |
36.0 (20.9) |
39.2 (20.4) |
< 0.001 |
|
Systolic BP |
122.7 (18.2) |
114.7 (12.7) |
0.001 |
|
Diastolic BP |
66.6 (8.9) |
63.7 (7.2) |
0.014 |
|
METS |
3.8 (1.5) |
5.7 (2.6) |
< 0.001 |
|
DXA Fat Mass |
85.1 (27.7) |
81.3 (27.9) |
< 0.001 |
|
DXA Lean Mass |
114.0 (21.8) |
113.7 (22.6) |
0.70 |
|
Duke Score |
29.7 (16.4) |
39.9 (14.7) |
< 0.001 |
|
Duke METS |
6.5 (2.0) |
8.2 (4.8) |
0.003 |
|
Rate your plate |
50.3 (7.6) |
56.1 (8.6) |
< 0.001 |
|
Dartmouth |
23.4 (5.2) |
18.3 (6.7) |
< 0.001 |
|
Cardiac Depression |
93.2 (15.4) |
91.0 (12.2) |
0.40 |
Figure 1.
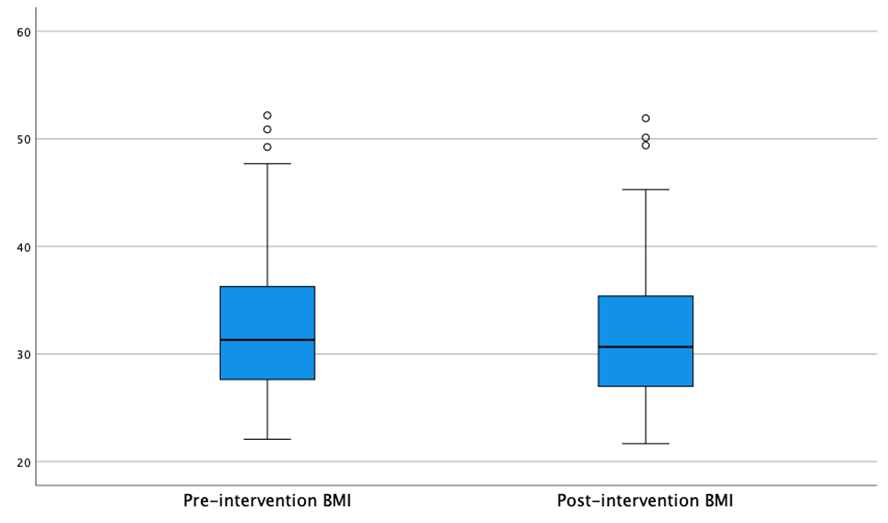
Figure 2.
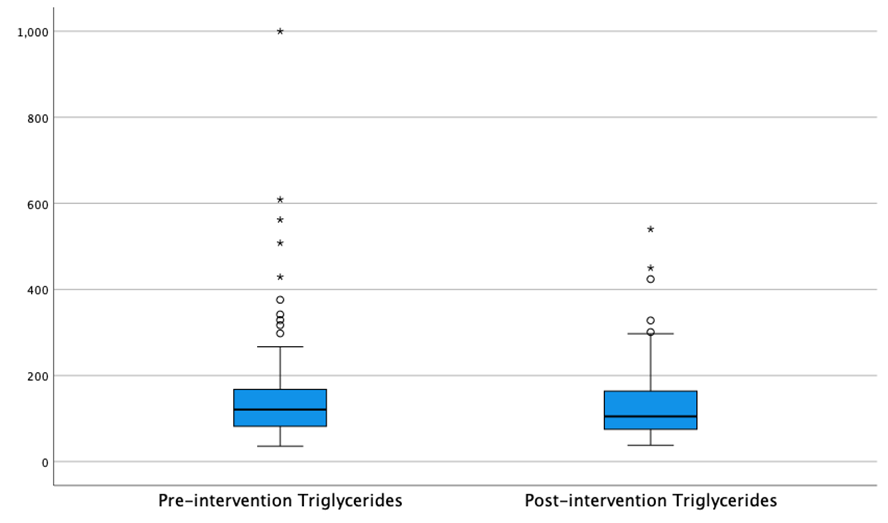
Figure 3.
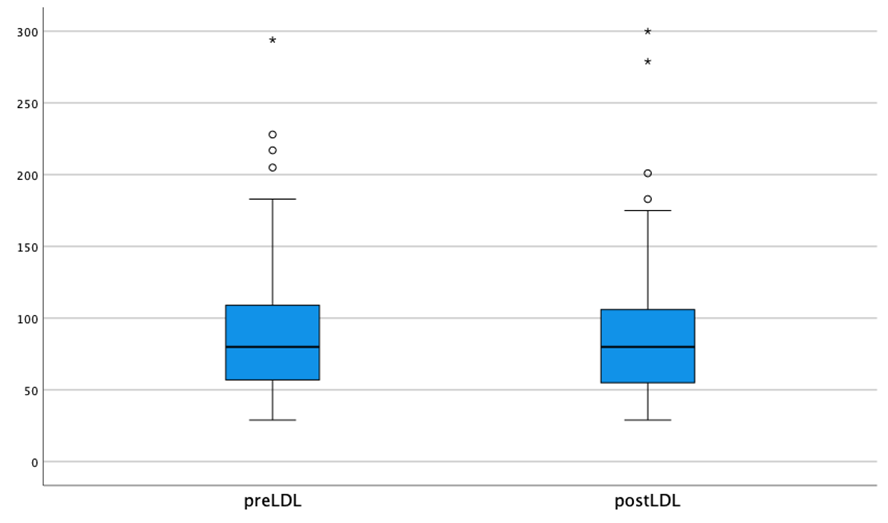
Figure 4.
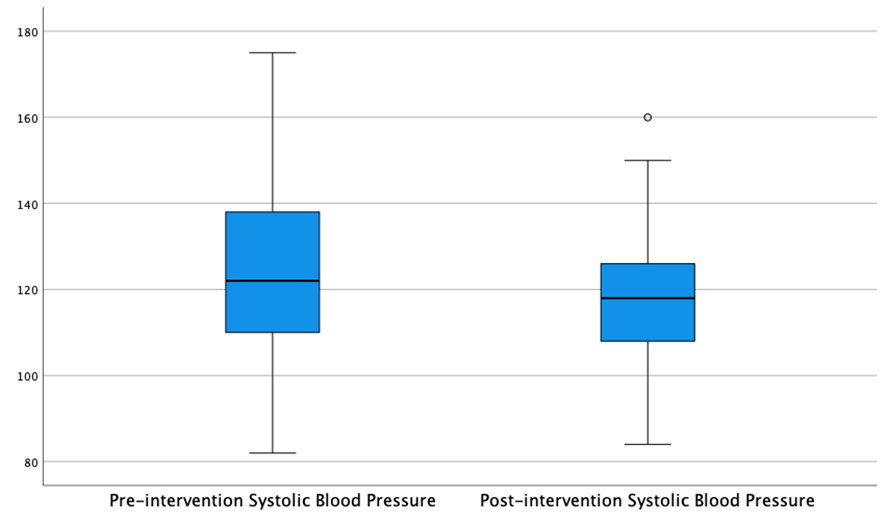
Figure 5.
Discussion
Our evaluation found that patients who complete the SH program following a major cardiovascular event show improvement in CVD risk factors including body composition, lipid profile, blood pressure, and depression score. These results are similar to previous studies on the effects of CR and ICR. Nalini et al (2013) reported improvements in body composition and body fat distribution after two months of CR which is comparable to our 9-week program. Previous studies measuring blood pressure effects following CR are conflicting. While Beckie et al. (2013) reported a decrease in SBP following traditional CR, other studies reported an increase in SBP (Aldana et al., 2003; Carlson et al., 2000). Results from literature indicate that ICR is more effective than traditional CR in reducing SBP (Thatcher, 2021). Silberman et al (2010) studied 2,974 participants in one of the CMS approved ICR program and reported significant reductions in SBP, DBP, and depression after 12-weeks. Our findings support this as we saw similar improvements after 9-weeks.
While our results show improvement in total cholesterol, LDL, HDL, and triglycerides values, only changes in HDL and triglycerides were significant. Of the 128 who completed the study, 47.6% had been prescribed a statin prior to starting the program with an average starting total cholesterol value of 153. This average is much lower compared to previous study populations. In Silberman et al (2010) study the average cholesterol value at program start was 187.7.
The benefits of CR have been shown to be dose dependent and program adherence has recently been added as performance measure by AACVPR. Ritchey et al (2020) tracked CR participation in 2016 and found that 26.9% of MCR beneficiaries who initiated CR completed 36 or more sessions. We saw a completion rate of 65% for this study. Barriers to completion match what many CR programs face nationally. These include transportation, work schedules, availability of healthy food, support systems within the home, willingness to change, and co-morbidities.
The SH Program is designed to be an intensive cardiac rehab program, with patients attending two 1-hour sessions per day, four days per week for 9-weeks, the intensity of the program helps patient keep momentum and improves attendance. The program includes exercise sessions at each visit that centers around functional capacity and movement as well as to include incorporation of strength training more often than traditional programs which focus more on cardiovascular training (i.e., Treadmill, bike) rather than strength training and conditioning. Strength training is important in the CVD patient population because it leads to improved balance and stability and in turn reduces risk for falls. Strength training also leads to a shift in body composition, decreasing fat mass and increasing lean mass which in turn improves bone density as shown in our DXA results. The patients in the SH program are exposed to live educational sessions with trained professionals who can give feedback on the progress in real time. The program differs from traditional CR in the structure of classes and addition of heavy focus on functional medicine, nutrition, and exercise education. The program also differs from already approved ICR programs in the fact that less emphasis is placed on a strict one-size-fits-all diet and more emphasis on the patients metabolic, medical, and environmental needs.
Patients in the SH program also reported significant improvement in physical activity, nutrition, and overall quality of life as reported by the patients in industry approved quality of life questionnaires.
In conclusion, our study demonstrates that the SH program is just as effective/non-inferior as the currently CMS approved programs and therefore should be considered as another option for CR and therefore CMS approval. Currently there are only three approved ICR programs which limits the options that current and future CR programs, as well as patients have, in choosing programming to increase utilization and adherence to Cardiac rehab. Dalal (2015) in his clinical review of cardiac rehabilitation concluded that one way to overcome the barriers to cardiac rehabilitation is by expanding access. This can be accomplished through the CMS approval of additional ICR programs such as the Strong Heart Rehabilitation Program.
Study Limitations
Patients were given the option to participate in the program or not participate instead of being randomized into participation groups. The researchers felt it unethical to ask people to not participate in a program that has been previously and extensively proven to improve patient’s health and quality of life. Furthermore, no conclusions can be made about the individual treatment measures on their own as the focus of the study was on the overall effects of the SH program in its entirety. Another limitation was the fact that nutrition was provided to every participant in the form of prepared meals. Having done this we feel that future participants may not be able to afford the kind of diet that was provided. We need to do more studies to make sure that the results were not only due to meals being provide.
Conclusions
The Strong Hearts program has a positive impact on the reduction of CVD risk factors and should be considered further for approval as an ICR program. Follow up studies are ongoing to determine if the impacts continue at 1-year post completion and beyond. This will be important to determining the extended effects of the program on long term CVD outcomes and progression of disease.