
Gustavo S Elmiro, Stanlley de Oliveira Loyola, Celina Lumi Kushida, Abissay Francisco Dias, Jessyka Bueno Cruz, José Onofre de Carvalho Sobrinho, Artur Henrique de Souza, Giulliano Gardenghi *.
ENCORE Hospital, Aparecida de Goiânia / GO - Brazil
*Corresponding Author: Giulliano Gardenghi, ENCORE Hospital Rua Gurupi, Qd.25, Lt.06 / 08 - Setor Vila Brasília - Aparecida de Goiânia - GO – Brazil.
Received: March 12, 2021
Accepted: March 25, 2021
Published: March 29, 2021
Citation: Gustavo S Elmiro, Oliveira Loyola S D, Celina L Kushida, Abissay F Dias, Jessyka B Cruz. (2021) Pilot Study on Analgesia by Continuous Blockade of The Erector Plane of the Spine After Cardiac Surgery. J Clinical Cardiology Interventions, 2(2); DOI: http;//doi.org/03.2021/1.1011
Copyright: ©2021 Giulliano Gardenghi, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction: After cardiac surgery (CS), chest pain limits the ventilatory capacity causing functional disability. Continuous blockage of the erector plane of the spine (BEPS) is a technique recently described, providing good analgesia of the chest wall. Objective: To evaluate the response to BEPS on pain perception in patients in the postoperative period of CS. Material and Methods: Pilot study that included patients in the postoperative period of CS, admitted to the intensive care unit (ICU). Pain was assessed using the visual analog scale. Blockades were used bilaterally in 42.9% of cases and unilaterally in 57.1% of cases. Ultrasound-guided BEPS with catheter insertion was performed for postoperative analgesia. The catheter analgesia regimen was performed with 0.5% Ropivacaine 20mL loading dose followed by continuous infusion at 0.24% 10mL / h for 48 hours. On the 3rd postoperative day, the catheter was removed, according to the institution's protocol. The statistical analysis was performed in a descriptive manner. Results: 7 subjects were approached (71.4% male; age: 57.6 ± 16.8 years; weight: 76.9 ± 7.3 kg; height: 1.7 ± 0.1 meters; BMI: 25.8 ± 2.0). Six patients (86%) were extubated in the operating room and the remaining patient was extubated in the ICU in 3.8 hours. The average length of stay in the ICU was 4.1 ± 0.7 days and the total length of stay was 10.4 ± 8.1 days. The painful perception of individuals submitted to BEPS was 5.3 ± 1.9 points in the pre BEPS versus 1.4 ± 1.5 points after the procedure. Conclusion: The use of BEPS in the postoperative period of CS may be related to pain reduction.
Introduction
Post-surgical pain continues to limit recovery and may increase the risk of perioperative morbidity in cardiac surgery. Poorly administered chest wall pain may also contribute to an increased incidence of pulmonary complications. Restricted postoperative ventilation can result in hypoventilation, atelectasis, pneumonia and increased length of hospital stay. Thus, it is important to treat surgical chest pain properly and to minimize the need for significant administration of opioids [1,2].
Chest wall pain can be iatrogenic due to median sternotomy or pain in the region where the chest drains are inserted. Chronic pain can develop after inadequate management of acute pain, contributing to additional physiological and psychological stress and consuming disproportionate physical and financial resources [1].
Another aspect of the present proposal to promote analgesia using fascial plane blocking techniques is related to minimizing the use of systemic opioids. The opioid crisis currently threatening the health of the global population forces healthcare providers to reconsider the appropriate analgesic options. Great efforts have been made to maximize multimodal analgesia and regional anesthetic techniques, to reduce pain and the need for opioid analgesics. These efforts were associated with improvements in ultrasound imaging technology (US) and a renewed interest in anatomical study that resulted in a proliferation of fascial plane blocks to assist in the provision of perioperative analgesia [1].
Pain in the postoperative period of cardiac surgeries is known to hinder the performance / effectiveness of physiotherapy and seeking techniques that aim to decrease the painful perception and consequently increase the responses to the proposed rehabilitation techniques is fundamental [3,4].
Considering the factors exposed here, the objective of this study was to report cases of analgesic control in the postoperative period of cardiac surgery with US guided blockage of the erector plane of the spine (BEPS), prior to the physiotherapy sessions, in the intensive care unit (ICU).
Material and Methods
Pilot study in which patients were evaluated in the ICU of Hospital Encore, in Aparecida de Goiânia / GO, Brazil. Approved by the Ethics Committee indicated by Plataforma Brasil, under number CAAE 38630920.7.0000.0033. All participants signed a free and informed consent term, according to Resolution 466/2012 of the Ministry of Health. The sample was obtained in the second half of 2019, adopting the following inclusion criteria: individuals with cognitive preservation to understand orders simple undergoing myocardial revascularization or valve replacement. Patients who did not understand the techniques that would be performed, those who refused to participate and those who presented hemodynamic instability during the evaluations would be excluded. Patients with decompensated heart failure and the presence of comorbidities, such as: unstable angina; moderate to severe respiratory disease; active infectious disease or feverish condition; disabling peripheral vascular disease; unstable ventricular arrhythmia and use of cardiac stimulation were also excluded. There was no discrimination of sex, race, skin color, socioeconomic level, education, origin, marital status or religion.
Patients underwent cardiac surgery (myocardial revascularization or valve replacement) and median sternotomy. The patients were operated under general anesthesia, receiving mechanical ventilation with a volume guaranteed by the ventilator between 6 and 8 ml / kg of body weight, ventilated with positive end-expiratory pressure (PEEP) between 6 and 8 cmH2O. All patients were weaned from mechanical ventilation after surgery in a period not exceeding eight hours, placed under regular oxygen therapy, with a nasal catheter, when necessary, aiming at a peripheral oxygen saturation (SpO2) ≥ 92%.
Pain was assessed by the anesthesiology team before the BPEE was performed, using a visual analog scale (VAS). US-guided BEPS with catheter insertion was performed in the ICU for postoperative analgesia. The catheter analgesia schedule was performed with 0.5% 20mL Ropivacaine in loading dose followed by continuous infusion at 0.24% 10mL / h for 48 hours. On the 3rd postoperative day, the catheter was removed, according to the institution's protocol. The BEPS works with the diffusion of the local anesthetic in the paravertebral and intercostal spaces. The spread of the local anesthetic in the paravertebral space in the cephalic-caudal direction can lead to analgesia from C7-T2 to L4-5, depending on the level of injection. It is assumed that the analgesic effect observed can block the thoracic spinal nerves [5].
After 30 minutes of BEPS, pain was assessed by the physiotherapy team. Figure 01 illustrates the BPEE technique, and the VAS used.
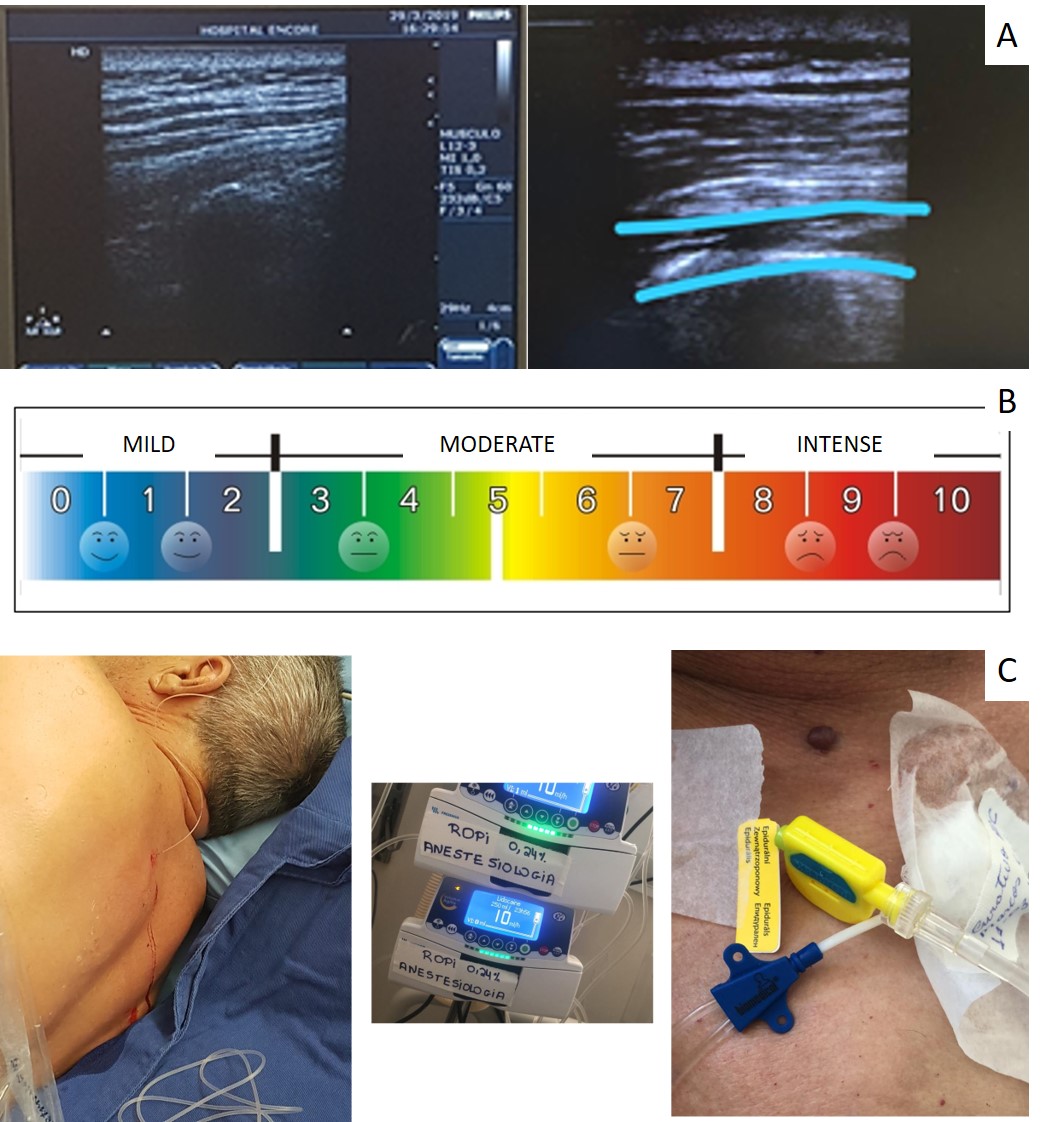
Figure 1: Example of application of the spinal erect plane blocking technique and visual analogue pain scale used in the study. A: Images illustrating the technique of blocking the erect plane of the spine guided by ultrasound. The highlight in blue lines shows the spinal muscles and the spread of the local anesthetic. B: Visual analog scale used to measure pain perception. C: Catheter placed on the erector plane of the spine for continuous analgesia.
Insert figure 01
All individuals were in the ICU when the protocol was performed. On the 1st postoperative day, all patients in the sample had a pleural drain and mediastinal drain, both in the subxiphoid region. On the 2nd postoperative day, the drains were removed.
Pain was assessed by the physiotherapy team before consultations. The guidance that the team receives is based on the fact that they start an exercise session with patients only when the VAS pain is less than 4 points. Physiotherapy sessions consisted of active exercises. On the 1st postoperative day, cycle ergometry of upper limbs was performed, in five-minute sessions, twice a day, according to the previous protocol described by our group [6]. Active assisted and free active exercises for upper limbs were also performed, using the full range of movement of the shoulders, in a bilateral and symmetrical manner, associated with a stick. In the lower limbs, knee extension exercises were performed, with the patient sitting on the bed in a beach chair position, using weights that varied between 1 and 2 kilos by means of shin guards, in one series of 10 repetitions, alternately, once a day. Ankle flexion-extension exercises were also performed.
On the second postoperative day, the protocol was repeated, with exercises for bedside sedestation, stationary gait and ambulation in the ICU environment, at intervals of five minutes each. The patient was also placed in a bedside chair, remaining in it for the longest tolerable time.
The use of non-invasive ventilation could be associated with exercises, according to a joint assessment between doctors and physiotherapists, aiming at maintaining pulmonary expandability and relieving the ventilatory work imposed by exercise.
Physiotherapy sessions would not start if the patient in the pre-intervention phase had any of the following vital signs: SpO2 <90%; Respiratory rate> 30 breaths per minute; Emergence of cardiac arrhythmias; Heart rate> 120 beats per minute; mean arterial pressure <60 mmHg or> 140 mmHg; Increased dose or adoption of a new vasoactive drug.
Statistical analysis
The results obtained in the study were expressed as mean and standard deviation. The software used for statistical analysis was Microsoft Excel®, version 2016. The statistical analysis, to compare the VAS values before and after the BPEE, used Student's t test with 5% significance.
Results
Seven individuals were included in the results. Regarding the characteristics of the sample, the data are presented in table 01.
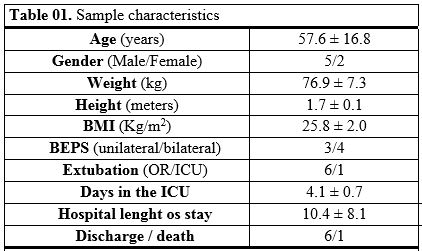
Subtitle: BMI: body mass index; BEPS: blockage of the erector plane of the spine; OR: operating room; ICU: intensive care unit
Six patients were extubated in the operating room and the remaining patient was extubated in the ICU in 3.8 hours.
Figure 02 illustrates the behavior of pain by VAS before and after BEPS in the postoperative period of cardiac surgery (p: 0.03). The pain remained low among the 1st and 2nd postoperative days, with all values below 4 points, making it possible to carry out the physiotherapy sessions, which were well tolerated by the patients. At no time was the patient asked to stop the exercises. No adverse events related to the mobilization occurred.
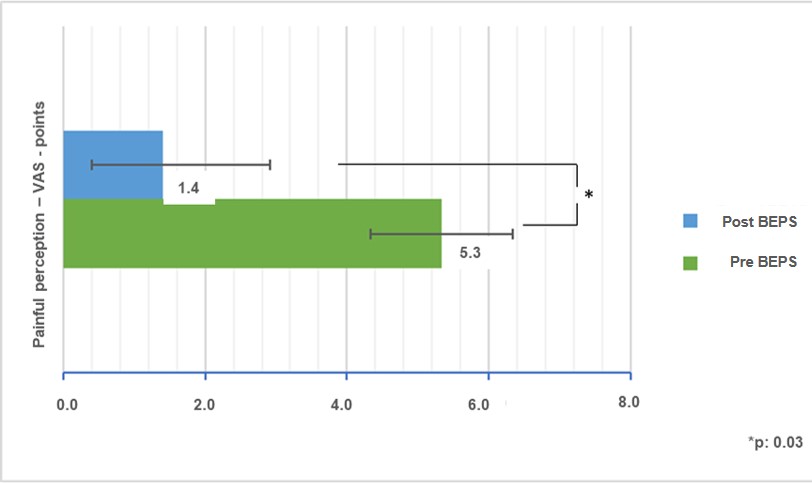
Figure 2: Pain on the visual analog scale before and after blocking the spinal erector plane (BEPS) in the postoperative period of cardiac surgery.
Insert figure 02
One of the patients died of major bleeding after five days in the ICU, unrelated to the BEPS technique or to the physiotherapy sessions performed.
Discussion
In the present article, US-guided BEPS was able to promote analgesia in the seven studied patients, with a significant drop in pain levels, which lasted, considering the continuous infusion of the drug, for more than 48 hours, making physiotherapy sessions feasible, which could be performed with greater efficiency / tolerance, without restrictions regarding the referred pain. The assessment of patients' pain in the postoperative period of cardiac surgeries was routinely based on our service, aiming at measuring pain perception, which guides the choice of analgesic method, which can vary from non-invasive techniques, such as the adoption of analgesia by transcutaneous electrical stimulation [4], until the adoption of BEPS, which in this case was the method chosen to test its efficiency and the feasibility of implementing the technique in our care routine.
In the postoperative period of cardiovascular surgeries, the management of chest pain is challenging for the assistance team. The use of high doses of opioids is not always effective for a good analgesic control and, in addition, it can generate chemical dependence which confers greater morbidity and expenses [2]. Adequate control of postoperative pain is fundamental for the patient's full recovery, avoiding possible pain chronicity, increasing patient satisfaction and contributing to a shorter hospital stay, with reduced risk of infection and pulmonary complications [7]. The persistence of chest pain, when there is ineffective analgesia, can limit lung expansion, thereby decreasing ventilatory capacity and functional capacity [1].
The BEPS with catheter was initially used for analgesia of fractures of multiple ribs and control of refractory herpetic pain and presented good results in the analgesic control [5]. This technique has the advantage of not entering the neuroaxis and thus not presenting contraindications in relation to the use of anticoagulation, making it a promising option for analgesic control in the postoperative period of cardiovascular surgeries [8].
Anatomical and radiological investigations have provided evidence that the site of action of the drugs is in the dorsal and ventral branches of the spinal nerves [7,8]. The use of BEPS in chest pain analgesia is a recent technique, first described in 2016 [8].
According to Park and collaborators [9], the most significant advantages of BEPS are its simplicity and security. The technique can be performed on patients with bleeding tendencies compared to central neuraxial blocks. Complications related to BEPS are rare, as it is an ultrasound-guided technique, the possible risk of pneumothorax is reduced [8]. Other possible rare complications are the motor weakness that occurs when the local anesthetic spreads to the lumbar plexus when the block is performed in the lower thoracic or lumbar areas and also systemic toxicity of the local anesthetic, which can occur with the use of high volumes of anesthetic location that spreads to the paravertebral and intercostal spaces, and to richly vascularized muscles, reaching the systemic circulation and can manifest signs and symptoms of the central nervous system such as tinnitus, confusion, convulsions and / or cardiovascular, such as hypotension, arrhythmias or cardiorespiratory arrest [8].
A major concern today is based on the chronic use of opioids. In the United States of America, opioid dependence was declared a public health emergency with 47,600 deaths related to its use in 2017, which already represents more deaths each year than car accidents or breast cancer [2]. It is known that the prescription of opioids at discharge from the postoperative period of cardiac surgery increases the risk of chemical dependence, with approximately 1 in 10 patients undergoing cardiac surgery can develop its chronic use [2]. BEPS thus becomes an important adjuvant therapy not only for analgesic control, but also in reducing the need for the use of opioids, especially after hospital discharge.
Our study has limitations that must be considered. As this is a pilot study, the results achieved may not represent the same effectiveness if larger populations were approached. Physiological variables such as heart rate, blood pressure, peripheral oxygen saturation, ventilatory frequency or tidal volume were not evaluated. Such notes could add greater value to the study presented here. Another limitation concerns time issues. No results were observed in the medium and long term, with late follow-up of the pain pattern presented by the patients. Larger studies on the application of US-guided Beps, in the form of randomized clinical trials, are necessary in order to verify the potential real treatment effect on pain in the postoperative period of cardiac surgery.
Conclusion
The present pilot study suggests that the use of BEPS in the postoperative period of cardiac surgery may be related to pain reduction, and it can be an alternative to alleviate the limitations caused by the increase in painful perception in these individuals.