
Kayla Martinez MD1*, Juleen Elizee MD 1, Thomaidha Qipo MD1, Naveen Multani DO2, Gurvir Kaur Mangat MS42, Noorulann Sherwani MS42, Stephanie Crass DO3, Shukri David MD3
1Ross University School of Medicine.
2Ascension Providence Hospital, Department of Cardiology and Interventional Cardiology.
*Corresponding author: Kayla Martinez, Ross University School of Medicine, USA.
Received: May 30, 2024
Accepted: June 07, 2024
Published: June 10, 2024
Citation: Martinez K, Elizee J, Qipo T, Multani N, Gurvir K Mangat. (2024) “Circulatory Conundrum: Investigating the Intersection of an ST-Elevation Myocardial Infarction with Myocardial Bridge.” J Clinical Cardiology Interventions, 4(2); DOI: 10.61148/2836-077X/JCCI/047
Copyright: © 2024 Kayla Martinez. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A myocardial bridge (MB) is defined by the deviation of a coronary artery segment from its typical epicardial course, instead traversing through the myocardium. Individuals afflicted with myocardial bridges may manifest symptoms including exertional chest pain, dizziness, diaphoresis, and shortness of breath, which cannot be attributed to a secondary etiology1. The prevalence of myocardial bridge is approximately 19%, although post-mortem studies have revealed a prevalence of 42% since most cases are asymptomatic2. We report the case of a 58-year-old Caucasian male who presented with chest pain.
myocardial bridge; chest pain; dizziness; diaphoresis; shortness of breath
Introduction:
A myocardial bridge (MB) is defined by the deviation of a coronary artery segment from its typical epicardial course, instead traversing through the myocardium. Individuals afflicted with myocardial bridges may manifest symptoms including exertional chest pain, dizziness, diaphoresis, and shortness of breath, which cannot be attributed to a secondary etiology1. The prevalence of myocardial bridge is approximately 19%, although post-mortem studies have revealed a prevalence of 42% since most cases are asymptomatic2. We report the case of a 58-year-old Caucasian male who presented with chest pain.
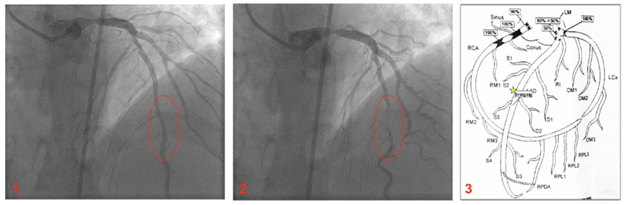
Images 1, 2, 3: Patient’s myocardial bridge captured in real time via cardiac catheterization. Red circle indicates bridging segment in a portion of the LAD, star indicates bridging segment on catheterization schematic.
Case Presentation:
A 58-year-old male with past medical history of end-stage renal disease secondary to polycystic kidney disease–on hemodialysis, anemia of chronic disease, hypertension, ischemic cardiomyopathy, protein C deficiency, brain aneurysm, and former tobacco dependence, was transferred to our hospital CVICU for evaluation of a coronary artery bypass grafting (CABG) vs. high-risk percutaneous coronary intervention (PCI). Over the last month he experienced dyspnea and intermittent burning-pressure like chest pain. His vitals on presentation were stable. EKG showed ST elevation in leads III and AvF with reciprocal changes in the anterior leads, consistent with an acute inferior STEMI and the cath lab was immediately activated. Oral aspirin, sublingual Nitroglycerin, and IV morphine were administered and IV heparin gtt was started. Labs showed elevated Troponin I at 0.77ng/mL. A bedside chest x-ray showed mild pulmonary volume overload. Urgent catheterization via right groin access showed severe 3-vessel CAD with left main involvement. The LCx and RCA were 100% occluded and PCI failed. Of note, the LAD showed diffuse moderate disease with bridging mid-segment. Balloon angioplasty of the left main was done with a 2.5mm balloon to improve flow to the LAD and collaterals. An intra-aortic balloon pump (IABP) was placed and he was transferred to our CVICU facility in stable condition.
Discussion:
A myocardial bridge is characterized as a congenital cardiac anomaly wherein one of the coronary arteries traverses a segment of the myocardial tissue. In the typical cardiac anatomy, coronary arteries are situated directly atop the myocardium. This arrangement facilitates the unimpeded perfusion of blood to septal arteries, thereby nourishing the myocardium. In the prenatal developmental phase, a muscular band may emerge encircling one of the coronary arteries, resulting in the formation of a myocardial bridge over the affected artery. During each myocardial contraction, the bridge applies pressure, inducing constriction in the specified artery. Consequently, this constriction may precipitate diminished blood flow to the heart.
Effectively addressing symptomatic myocardial bridge poses a considerable challenge in clinical management. Clinicians are advised to meticulously evaluate the patient's symptoms, cardiac anatomy, extent of ischemia, and the presence of concurrent comorbidities. Presently, comprehensive cardiovascular society guidelines pertaining to the diagnosis or management of MB do not exist. Nevertheless, cardiac catheterization offers insight into the assessment and diagnosis of MB. Traditionally, angiography stands as the primary diagnostic modality for myocardial bridge. The identification of systolic narrowing or "milking" of the vessel during angiography serves as a key indicator of MB. In cases where patients experience intolerable or worsening chest pain, a surgical unroofing procedure represents a viable intervention3. To enhance patient care for myocardial bridge, we aim to show the collaborative, multidisciplinary approach between medicine and cardiology in its assessment.
Conflict of Interest: This study does not have any conflict(s) of interest.