
Sonia Houssany-Pissot MD1, Cyril Voisard MD2, Henri Broustet MD1, Philippe Commeau MD3, Benoit Lattuca MD, PhD4, Marie Hauguel-Moreau MD5*
1Department of Cardiology, Hôpital d’Instruction Des Armées Percy, Clamart, France.
2 Université Paris Saclay, Université Paris Cité, Ecole Normale Supérieure Paris Saclay, Centre National de la Recherche Scientifique, Service de Santé des Armées, Institut National de la Santé et de la Recherche Médicale, Centre Borelli, Gif-sur-Yvette, France.
3Department of Cardiology, Polyclinique Les Fleurs, Groupe ELSAN, Ollioules, France.
4Department of Cardiology, Nîmes University Hospital, Montpellier University, Nîmes, France.
5Université de Versailles-Saint Quentin, INSERM U-1018, CESP, Department of Cardiology, Ambroise Paré Hospital, Assistance Publique-Hôpitaux de Paris, Boulogne-Billancourt, France.
*Corresponding author: Marie Hauguel-Moreau, Université Versailles-Saint Quentin AP-HP, Hôpital universitaire Ambroise Paré, Service de Cardiologie ACTION Study Group, Paris 9, avenue Charles de Gaulle, 92100 Boulogne-Billancourt, France.
Received: February 01, 2024
Accepted: February 08, 2024
Published: March 05, 2024
Citation: Houssany-Pissot S, Voisard C, Broustet H, Commeau P, Lattuca B, Hauguel-Moreau M. (2024) “Managing Pregnancy as an Interventional Cardiologist: A National Survey.” J Clinical Cardiology Interventions, 4(1); DOI: 10.61148/2836-077X/JCCI/046
Copyright: © 2024 Marie Hauguel-Moreau. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Concerns about radiation exposure during pregnancy are reported as a major barrier to female cardiologists choosing interventional cardiology (IC). These concerns might arise from a lack of knowledge of radiation safety and a lack of consensus on occupational radiation exposure during pregnancy. This results in a wide range of female IC behaviors regarding pregnancy.
Methods: To analyze French female IC behavior regarding pregnancy, we emailed a national survey to all female IC members of the Groupe Athérome coronaire et Cardiologie Interventionnelle.
Results: Of 37 (59%) respondents, 25 (67%) had at least one child. 61% stopped IC at the beginning of pregnancy, 78% of them because of personal fears regarding radiation. 82% of respondents who did not stop IC during pregnancy reported no fear of radiation exposure because of reassuring literature data. 77% of respondents had little or no knowledge of fetal radiation risks. Respondents reported good support from their colleagues in 58% of cases, and little or no support in 42% of cases. Cessation of IC at the beginning of pregnancy was associated with less support from colleagues.
Conclusion: In a context of increasing feminization of IC and reassuring data on fetal radiation exposure effects, fear of radiation during pregnancy remains a major concern among female interventional cardiologists, and leads most of them to suspend their interventional activity. This concern should be addressed by up-to-date guidelines on pregnancy and radiation exposure, and dedicated educational programs, addressing both male and female interventional cardiologists.
pregnancy; interventional cardiologist; occupational radiation exposure; radiation protection
Introduction
Increasing participation of women in interventional cardiology continues to lag behind participation in medical and surgical fields. With orthopedics, interventional cardiology has the most imbalanced sex ratio (1). Only 7.7% of interventional cardiologists (IC) are women (2). The causes for this lag include perception of the career’s effect on family life and radiation exposure during pregnancy (3). IC typically have little education on the occupational exposure risk during pregnancy and, as such, are challenged in making an informed decision. IC are exposed to the highest dose of X rays (4). Despite reassuring data on the limited effect of radiation exposure on fetal development (5), guidelines on occupational radiation exposure during pregnancy are disparate worldwide: the National Council on Radiation Protection and Measurements in the USA recommends limiting occupational radiation exposure of the fetus to no more than 5 millisieverts (mSv) during pregnancy, French legislation sets the threshold to 1 mSv, while other countries (such as Italy) prohibit occupational radiation exposure during pregnancy and even during the breastfeeding period (6,7) (Supplemental Table 1).
|
|
IC with children |
IC without children |
|
|
|||||||
|
Parameters |
Number |
Mean |
SD |
Number |
Mean |
SD |
p-value |
||||
|
Number of respondents |
25 |
|
|
12 |
|
|
|
||||
|
Age, years |
24 |
42.6 |
8.3 |
11 |
41 |
9.2 |
0.63 |
||||
|
Angioplasty procedures/year |
21 |
223.6 |
109.5 |
12 |
229.2 |
111.6 |
0.89 |
||||
|
Structural interventions/year |
23 |
41.3 |
56.2 |
12 |
36.2 |
59.4 |
0.80 |
||||
|
Interventional half-days/week |
25 |
3.3 |
1.5 |
12 |
3.5 |
1.4 |
0.68 |
||||
IC=interventional cardiologist ; SD=standard deviation
This lack of consensus on occupational radiation exposure during pregnancy results in a wide range of attitudes towards pregnancy among IC. While 60% of surveyed Italian IC reported that they would eventually stop working in cardiac catheterization laboratory (cath lab) during pregnancy (8), no study, to date, has assessed the real attitude of currently working IC.
In this study, we assessed the attitude of French female IC towards their interventional activity during pregnancy.
Method
The survey, named “woMen intErventional caRdiologist attitude regarding prEgnancy and X-ray exposure” (the MERE study), was emailed to all French female IC members of the Groupe Athérome coronaire et Cardiologie Interventionnelle (GACI) on May 7th, 2019 with two reminders on June 24th and October 4th. The survey was closed on December 2nd, 2019. It was an online anonymous survey. We encouraged participants to forward the survey to young female IC who were not yet in the GACI’s list of contacts. However, no fellows-in-training were enrolled. The majority of questions were multiple choice, with the possibility to add a free comment (Table S1). Some questions were open-ended. It was not mandatory to answer all the questions to complete the survey.
The first part of the survey was dedicated to demographic data: year of birth, type of practice (public or private), city, experience as an IC (first year of practice, number of angioplasty or structural cardiology procedures, number of weekly half-day work sessions), demography of the cath lab (number of IC in the unit and number of female IC). The second part of the survey was about motherhood: number of children, age at first birth, medical issues in getting pregnant or during pregnancy and potential radiation-related disease among children. The third part was about the attitude of each participant in the cath lab during pregnancy with variable questions depending on previous answers (absence or not from cath lab, duration, reasons). This section was filled in for each pregnancy while working at the cath lab. The fourth part of the study tried to assess the level of knowledge on radiation-related fetal risk of the participant and colleagues. We also asked about the support that participants had from their colleagues and head of department according to their occupational choices during pregnancy.
Finally, we asked about the radiation protection equipment available in centers. The final question was an open question about the potential impact that pregnancy had on their choice of career.
Categorical data are reported as number and percentages and compared using the 2 test or Fisher’s exact test as appropriate. Statistical tests were considered significant for a P value <0.05. Statistical analysis was performed with R Development Core Team (2019) (R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
Results
Study Population
We sent the survey to 63 French female IC members of the GACI. Thirty-seven participants (59%) answered the survey: 25 had at least one child (Table 1). Mean age was 41 ± 9.0 years old and 59% of respondents were <40 years old. The mean occupational duration was 11.5 ±7.9 years and 92% of respondents worked in a public hospital. There was no interventional activity difference between women with children and women without children. The average number of children per woman was 1.27 ±1.19. Mean age at first child was 30.9± 4.9 years old.
Behavior Regarding Interventional Cardiology During Pregnancy
Concerning analysis of the behavior of IC during pregnancy, statistics were based on the total number of pregnancies during interventional cardiology practice (n=47), since each pregnancy is a single event with potentially different IC behavior regarding work in the cath lab. Three pregnancies were excluded from the analysis since they occurred before practicing interventional cardiology. Forty-four pregnancies were included in the analysis (Figure 1).
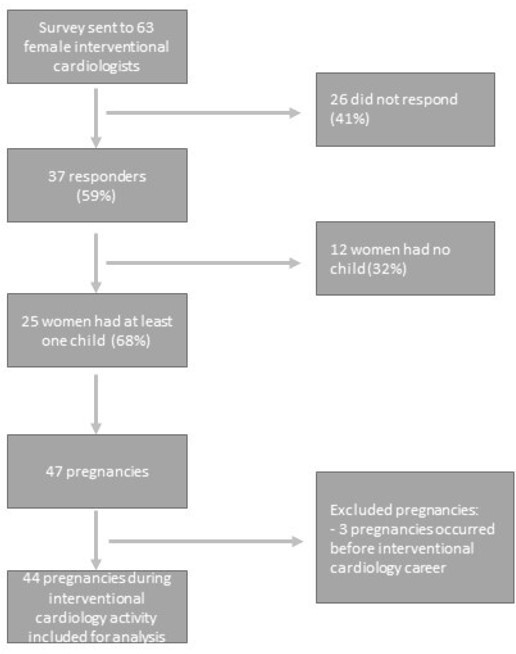
Figure 1: MERE study flow chart
For 27 pregnancies (61%), respondents reported having stopped work in the cath lab at the beginning of the pregnancy (Table 2), 78% of them because of personal fears concerning fetal radiation exposure risks and 30% of them because of their spouse’s fear. The reason given for stopping work in the cath lab was fear of a blood exposure accident in 11% of respondents and a staff instruction in 11% of respondents. Only 4% of respondents reported having stopped interventional activity following instruction from the head of department. Eleven percent of respondents planned the pregnancy during a non-exposure period.
Table 2: Women’s behavior during pregnancy (N=44)
|
Interruption of IC n=27 (61%) |
Motivations to stop |
Percentage (%) |
|
|
|
Instructions from the head of the cardiology department |
4 |
|
|
|
Instruction from the occupational health physician |
11 |
|
|
|
Spouse’s fear of the risks |
30 |
|
|
|
Personal fears about radiation exposure |
78 |
|
|
|
Fear of an accidental blood exposure |
11 |
|
|
|
Pregnancy planned during a non-exposure period |
11 |
|
|
Continuation of IC n=15 (34%) |
Motivations to continue |
|
|
|
|
Fear of colleagues’ reactions |
27 |
|
|
|
Fear for career advancement |
27 |
|
|
|
Reassuring literature on radiation exposure |
82 |
|
|
|
Reassuring experience of female colleagues |
9 |
|
|
No information n=2 (5%) |
|
|
|
IC=interventional cardiology
Respondents reported not having stopped interventional activity for 15 pregnancies (34%): 6 respondents (14%) continued interventional cardiology until the end of the first trimester and 9 respondents (20%) continued until the end of the second trimester. The reasons for not stopping were absence of concerns in the literature in 82%, fear for career prospects in 27%, fear of colleagues’ reactions in 27%, and reassuring previous experience of female colleagues in 9%. Women IC did not change their attitude towards a second pregnancy compared to the first (n=14 women): all women who stopped interventional cardiology during a first pregnancy (n=10) stopped IC for the second also, whereas all women who continued interventional cardiology during a first pregnancy (n=4) also continued during the second.
Table 3 shows additional precautions taken while pursuing interventional activity during pregnancy. Ninety-one percent of respondents who pursued cath lab activity during pregnancy had a close dosimetric follow-up and 73% avoided complex procedures with higher radiation exposure (chronic total occlusion, for example).
Table 3: Additional precautions regarding radiation exposure during pregnancy (n=11 answers among respondents who pursued IC during pregnancy)
|
Additional precautions |
|
|
Close dosimetric follow-up |
10 (91%) |
|
Avoiding complex procedures (CTO) |
8 (73%) |
|
Reinforcement of protective screens |
8 (73%) |
|
Reduction of cath lab activity |
3 (27%) |
|
Close medical follow-up |
2 (18%) |
|
Double lead apron |
2 (18%) |
|
Other |
1 (9%) |
CTO=chronic total occlusion, IC= interventional cardiology
No difference was reported regarding complications or malformations during pregnancy regardless of the attitude to interventional cardiology (interrupting cath lab activity or not) (Table 4).
Table 4: Complications of pregnancy and malformations according to female interventional cardiologists’ behavior regarding pregnancy (n=44)
|
Continuation of IC during pregnancy |
Complications during pregnancy |
Child malformation |
|
No: 27 (61%) |
1 |
2 |
|
Yes: 15 (34%) |
2 |
1 |
|
No information: 2 (6%) |
0 |
0 |
IC=interventional cardiology
Women’s level of awareness about radiation
Overall, 77% of respondents had little or no knowledge of fetal radiation exposure risks. Of the 25 participants who had at least one child, 36% reported having no information about fetal radiation exposure risks, 36% reported having a poor knowledge, and 28% reported having a good knowledge.
There was no difference in the reported level of knowledge of fetal radiation exposure risks between women who stopped IC during pregnancy and women who continued (p=0.99) (Figure 2).
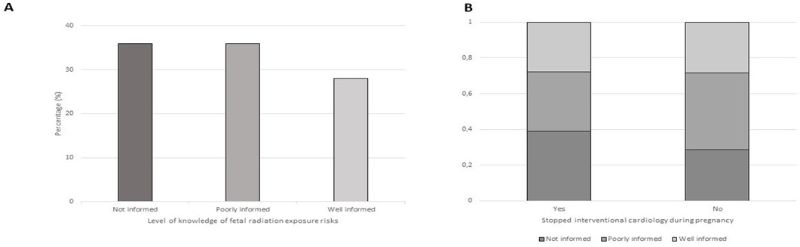 Figure 2: A. Female IC’s level of knowledge of fetal radiation exposure risks among respondents who had at least one child (n= 25 answers). B. Female IC’s level of knowledge of fetal radiation exposure risks among respondents according to cessation of interventional activity
Figure 2: A. Female IC’s level of knowledge of fetal radiation exposure risks among respondents who had at least one child (n= 25 answers). B. Female IC’s level of knowledge of fetal radiation exposure risks among respondents according to cessation of interventional activity
Good support from colleagues was reported by 58% of respondents, and little or no support by 42%s. Cessation of interventional activity at the beginning of pregnancy was associated with a lower degree of support by colleagues (p= 0.008) (Figure 3).
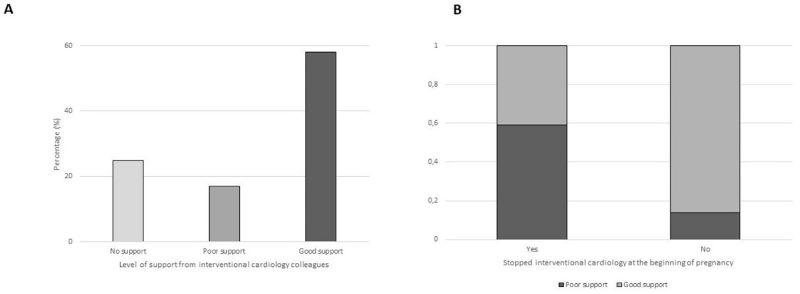
Figure 3: A. Support from colleagues among respondents who had at least one child (n= 24 answers).
B. Support from colleagues among respondents according to cessation of interventional activity
Finally, we asked whether the desire for pregnancy had an impact on choice of career: 8 (22%) respondents did not answer, 14 (37%) reported no impact, 4 (11%) reported a possible impact, and 11(30%) said it definitely had an impact.
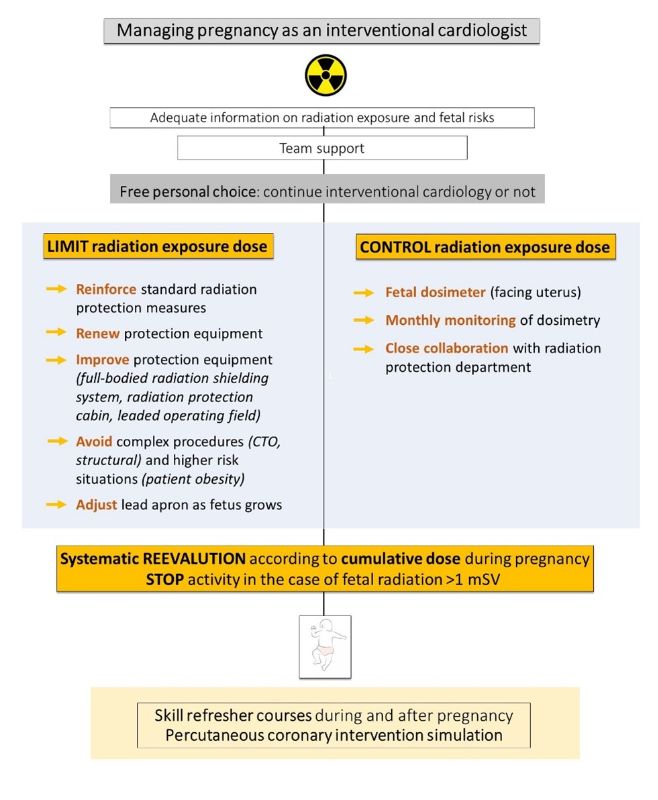
Figure 4: Algorithm to manage radiation safety for pregnant interventional cardiologists.
Radiation Exposure
Considering all participants, the following protective equipment was available: 35 (94.6%) had a lower body shield, 26 (70.2%) had a ceiling suspended lead screen, 33 (89.2%) had a recent lead apron, 12 (32.4%) had a mobile lead door, 21 (56.8%) had a recent cath lab (<5 years). No respondent who pursued interventional cardiology during pregnancy was able to report her fetus’s radiation exposure dose during pregnancy.
Discussion
Our study showed that 1) 67% of respondents had at least one child, with an average number of children per woman of 1.27 and a mean age at first birth at 30.9 years old; 2) 61% of surveyed French female IC interrupted interventional activity during pregnancy, while 34% continued. Twenty percent were able to maintain cath lab activity during the first two trimesters of pregnancy. This is the first survey studying the behavior of female IC regarding pregnancy.
This study provides demographic characteristics of French female IC concerning pregnancy. Among respondents, 32% were childless, which is higher than in the general female population in France (10.2%) (9). Furthermore, 100% of childless female IC reported having a low level of awareness regarding radiation exposure while one-third reported having avoided or delayed pregnancy during the early stage of their career for fear of being penalized. Previous studies have highlighted that trouble reconciling family and career demands leads to self-exclusion from interventional cardiology by women. In the light of our survey, one could argue that interventional cardiology may deter women from planning a pregnancy.
Concerning respondents who chose to have a family, age at first birth was similar to that of the general female population in France (30.9 versus 31 years old). However, the average number of children per woman was significantly lower in respondents (1.27) than in the general female population with a similar socioeconomic status (2.0 in the upper socioeconomic status class in France in 2020) (10). There may be many reasons for such a result. Motherhood-related absence from the cath lab has detrimental impact on both a pregnant IC and her interventional cardiology team. Long-term absence from the cath lab by pregnant IC may negatively affect technical skills. In a previous article, we showed that coronary angiography and percutaneous coronary intervention (PCI) simulation can help trainees to maintain their learning curve (11). However, PCI simulator use is not yet generalized. In an Italian survey, 38.9% and 69.6% of respondents, respectively, believed that it would be useful to perform PCI simulations and to participate in skill refresher skills courses on return to work (8). The British Cardiovascular Society provides resources for cardiology trainees and consultants returning to work after a period of absence (12). Concerning detrimental effects on an interventional cardiology team, the workload if IC is inevitably redistributed to colleagues. In our study, 50% of respondents worked in small teams of ≤4 IC and no replacement of pregnant physicians was proposed. Cessation of interventional activity at the beginning of pregnancy was associated with a low degree of support from colleagues. Furthermore, the reasons for pursuing interventional activity during pregnancy were fear of colleagues’ reactions (increased workload, discrimination) and fear for personal career in 27% of cases. In a previous survey among interventional radiologists, 68% of respondents (73% men and 27% women) reported that working with a pregnant woman would affect their work hours. However, this perception decreased among interventional radiologists who previously worked with a pregnant coworker (13).
In our study, 61% of surveyed French female IC interrupted cath lab activity during pregnancy which is consistent with the Italian survey which interviewed both male and female IC (8). The main reasons were personal fears regarding ionizing radiation and spousal fears about general pregnancy risk. On the other hand, 20% maintained cath lab activity during the first two trimesters of pregnancy. They reported having close dosimetric follow-up, performing no complex PCI and having reinforced protective screens during pregnancy or breastfeeding. Interestingly, 78% of respondents stopped cath lab activity because of fear of radiation exposure, while 82% of respondents who continued cath lab activity had no concerns about radiation since they considered the literature data to be reassuring. These findings illustrate the growing concern about the impact of fetal radiation exposure during pregnancy in a context of feminization of the profession.
While the level of radiation exposure awareness was not associated with the choice of whether or not to continue cath lab activity during pregnancy, most respondents (96%) reported poor support from radiation protection officers during pregnancy. No respondent assessed her fetal radiation exposure dose during gestation, whereas European Directive 2013/59 established 1 mSv as the dose limit in France. However, in France, the mean level of radiation exposure was 0.11 mSv in 2019, which is well below guideline thresholds, and has continuously and significantly decreased by 0.02 mSv/year over the last 10 years. (14) There was no difference in pregnancy complications or malformations in our study. However, this result is highly limited by the small number of respondents. Ionizing radiation has two types of adverse events. Deterministic effects result from damage to a group of cells, and occur at a threshold dose: intrauterine growth retardation, pregnancy loss, mental retardation, congenital malformations. Stochastic events result from single-cell damage and with increasing probability as the radiation dose is increased: childhood cancer, hereditary diseases in the descendants (2). Data on low-dose radiation exposure derive mainly from animal studies (15). However, there is no demonstrable risk of malformation and childhood cancer under 100 mSv (16). Other studies have reported that the fetal risk of malformation increases at a threshold of >150 mSv (17). Fetal radiation exposure for a pregnant worker in a cath lab is much lower than the threshold dose for these effects (18). Velazquez et al reported a study of 5 pregnant IC wearing under-the-lead badges. Four of them had radiation levels consistent with background radiation, and 1 IC had a total of 0.2 mSv throughout her pregnancy, which is much lower than the recommended maximum dose throughout pregnancy (19,20). Two consensus papers suggest it is feasible for a pregnant worker to pursue interventional activity with careful management of radiation exposure and monitoring of the received dose (18,21). Overall, the protection equipment seemed to be satisfying in surveyed centers and consistent with previous reports (22). In figure 4, we propose an original algorithm to manage radiation safety for pregnant interventional cardiologists.
This survey has several limitations. First, the low rate of response (59%) prevents us from extrapolating the results to all female IC. This low rate of response is partly due to the lack of an official census of IC in France, and therefore no official way to reach out to female IC. A low rate of response to this kind of survey has already been reported by Vautrin et al, who noted a similar participation rate of 53% (23). It would be of interest to have a precise census of male and female IC to predict the future demography of IC. Considering the feminization of interventional cardiology, we felt it important to report the responses of French female IC, even with small sample. Second, such a study should also be sent to male IC, to be able to compare pregnancy-related attitudes. However, we chose not to send it to male IC for two reasons: first, we would have faced the same difficulty in reaching out to male IC, and we aimed to assess the real attitude of female IC towards pregnancy. Finally, the level of radiation awareness was only declarative and no knowledge questionnaire was assessed. However, most respondents reported poor support from radiation protection officers during pregnancy, and not enough information.
Conclusion
In a context of increasing feminization of interventional cardiology and reassuring data on fetal radiation exposure effects, our study shows that fear of radiation remains a major concern among female IC during pregnancy and leads the majority of them to suspend their interventional activity. While X-ray protection equipment seems to be satisfying, education and support from radiation protection officers should be improved. To this end, we propose original guidelines for IC who choose to continue interventional cardiology during pregnancy.
Conflict of interest
Dr Hauguel-Moreau, Dr Houssany-Pissot, Dr Voisard, Dr Commeau and Dr Broustet have no conflict of interest. Dr Lattuca has received research grants from Biotronik, Boston Scientific, Daiichi-Sankyo, Fédération Française de Cardiologie and Institute of CardioMetabolism and Nutrition; consultant fees from Daiichi-Sankyo and Eli Lilly; and lecture fees from AstraZeneca, Medtronic and Novartis.
Abbreviations and Acronyms
cath lab: catheterization laboratory
GACI : Groupe Athérome coronaire et Cardiologie Interventionnelle
IC: Interventional cardiologist
MERE study: woMen intErventional caRdiologist attitude regarding prEgnancy and X-ray exposure
mSv: millisieverts
Highlights
• About two thirds of French female surveyed interventional cardiologists stopped interventional activity during pregnancy.
• Fear of radiation remains a major concern among female interventional cardiologists during pregnancy while the mean level of radiation exposure is far under the 1mSv guidelines threshold.
• In this article, we provide original guidelines for interventional cardiologists who choose to continue interventional cardiology during pregnancy.