
Healy L 1, Fitzpatrick N 1, Jauvert G 1, Tahin T 1, Galvin J 1, Szeplaki G 1, O’Brien J 1*
1 Mater Private Hospital, Eccles St, Dublin, Ireland.
*Corresponding author: Jim O’Brien, Consultant Cardiologist and electrophysiologist Mater Private Hospital, Dublin, Ireland.
Received Date: February 07, 2024
Accepted Date: February 16, 2024
Published Date: February 21, 2024
Citation: Healy L, Fitzpatrick N, Jauvert G, Tahin T, Galvin J, Szeplaki G, O’Brien J. (2024) “Case Study: Cardiac Resynchronisation Device Far-Field Oversensing with Transvenous Pacing Device.” J Clinical Cardiology Interventions, 4(1); DOI: 0.61148/2836-077X/JCCI/046.
Copyright: © 2024 Jim O’Brien. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
.
.
Introduction
Transvenous pacing (TVP) is an important intervention in emergency settings. In a clinical setting where an active right ventricular (RV) lead is already in-situ during TVP placement, far-field oversensing can be a potential issue resulting in pacing inhibition. This could be a significant concern if a patient is completely pacing dependant with no reliable intrinsic rhythm. To our knowledge, there is no reported literature regarding a temporary pacing wire resulting in cardiac resynchronization therapy (CRT) pace-sense lead inhibition.
Clinical scenario
A 88 year-old male with a history of CRT-P presented to our institute with blood cultures positive for staphylococcus aureus, raised serum inflammatory markers, erythema and pain around site of CRT implant and purulent discharge from surgical skin incision. A multi-disciplinary decision was made for CRT extraction with later reimplantation. A TVP was placed prior to CRT extraction owing to 100% pacing dependence. CRT RV lead capture threshold was 0.8V @ 0.5ms and the device was programmed to a backup VVI pacing rate of 30bpm at a sensitivity of 2.0mV. During a TVP threshold test, sudden asystole was noted on decremental reduction in pacing output (fig 1. And fig 2.). Assessment of the TVP revealed no connection errors and a consistent capture threshold of 3.5mA. It ultimately became apparent that the TVP lead tip, in close proximity to the CRT RV pace-sense lead, was causing RV lead oversensing of the TVP bipolar pacing spikes when they had fallen below threshold outputs, thus causing CRT pacing inhibition and asystole. The CRT RV lead sensitivity was reduced from 2.0 to 4.0mV and the TVP tip was positioned further from the RV lead, preventing further oversensing. At repeat testing, CRT RV lead now continued to pace normally following loss of TVP capture without any further issues. An astute senior cardiac physiologist was later heard saying: “If you see asystole, turn off the temporary wire”!
Conclusion
This case is the first to report the potential hazard of cross-talk between two pacing devices in close proximity. Reducing sensitivity, programming a VOO backup mode or re-positioning of the leads should usually resolve the issue. Operators should be aware of this potential complication when placing a TVP near a pace-sense lead in patients who are 100% pacing dependent.
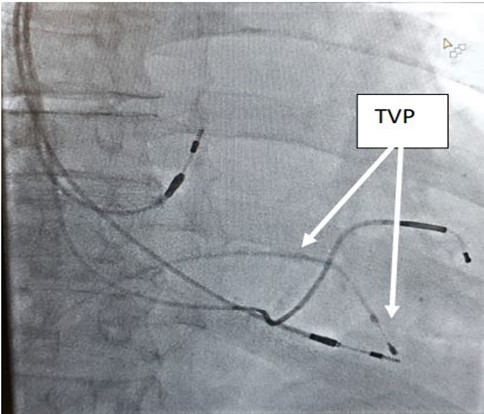
Figure 1. Close proximity of transvenous pacing wire (TVP) to distal electrode of CRT-RV lead (RAO projection)
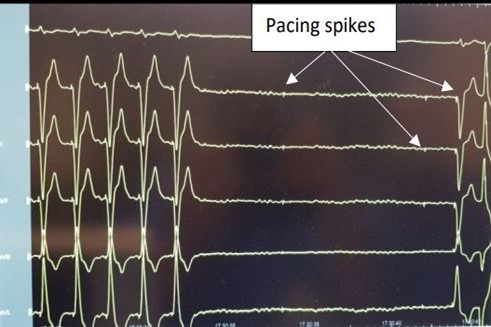
Figure 2. Asystole noted with decremental output during threshold testing from the TVP, note the pacing spikes of the TVP on the isoelectric line
.