
Christopher Armenia MD1*, Venkat Manubolu MD2,3, Sion Roy MD2,3, Joseph L Thomas MD2,3
1Department of Medicine, Harbor-UCLA Medical Center, Torrance, CA, USA.
2Division of Cardiology, Harbor-UCLA Medical Center, Torrance, CA, USA.
3The Lundquist Institute for Biomedical Research at Harbor-UCLA, Torrance, CA, USA.
*Corresponding Author:Christopher Armenia, Harbor-UCLA Medical Center 1000 W. Carson St Box 400 Torrance, CA 90502, USA.
Received Date: January 12, 2024
Accepted Date: January 20, 2024
Published Date: February 12, 2024
Citation: Armenia C, Manubolu V; Roy S, Joseph L Thomas. (2024) “Computed Tomographic Angiography of LAD-Diagonal Bifurcation Lesions: A Case-Based Study.” J Clinical Cardiology Interventions, 4(1); DOI: 0.61148/2836-077X/JCCI/044
Copyright: © 2024 Christopher Armenia. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Coronary artery bifurcation lesions are present in 20% of percutaneous coronary interventions (PCI). Compared to non-bifurcations, they have a higher incidence of procedural complications, periprocedural adverse events and restenosis.
The V-RESOLVE score uses five characteristics (main branch plaque distribution, diameter stenosis of the bifurcation core, bifurcation angle, diameter ratio of the main branch and side branch, and main branch stenosis) assessible on coronary CT angiography (CCTA) to risk-stratify bifurcation lesions. However, some of these characteristics are difficult to obtain without advanced reconstruction analysis. Prior studies evaluating single characteristics to risk-stratify bifurcation lesions have found that smaller bifurcation angles are associated with procedural complications. A large portion of the published data involves left main coronary artery bifurcations. The data are lacking regarding single CCTA characteristics in bifurcation lesions involving the left anterior descending (LAD) and diagonal arteries.
We utilized three easily obtained V-RESOLVE characteristics (plaque distribution, bifurcation angle, and the degree of stenosis in the side branch) to analyze PCI complications in a series of ten patients with LAD-Diagonal bifurcation lesions.
The average bifurcation angle in this report was 31°. Four patients had the high-risk features of main vessel plaque on the wall adjacent to the side branch. Two patients had a side branch stenosis greater than 50%. Two patients had procedural complications. Both patients had a bifurcation angle less than the average and both had main branch plaque on the wall adjacent to the side branch ostium even though the diagonal branch stenosis was less than 50%.
This report demonstrates that additional characterization of CCTA information may help predict or reduce procedural complications in bifurcation PCI. Assessing CCTA data for bifurcation angle measurements and main branch plaque location may be useful prior to angiography and PCI involving the LAD-diagonal bifurcations.
coronary artery disease; bifurcation; coronary CT angiography
Introduction
Coronary artery bifurcation lesions occur at or near the division of a major coronary artery into two branches, termed the main branch (MB) and the side branch (SB).1 Bifurcation lesions are estimated to account for approximately 20% of lesions treated during percutaneous coronary intervention (PCI).1-3 Bifurcation lesions warrant great attention due to the technical complexity and incidence of procedural complications. SB occlusion after the stenting of the MB is associated with increased risk of myocardial infarction and death.4 The incidence of SB occlusion in bifurcation PCIs has been estimated to be between 8% and 19%.5
Two PCI strategies an be employed when treating treat bifurcation lesions: the provisional single-stent technique and the two-stent technique. Debate remains over when provisional or two-stent techniques are preferred. A meta-analysis of eight randomized control trials comprising of 2778 patients found that the single-stent technique was associated with a lower risk of all-cause mortality at an average follow-up of three years.6 Despite some data supporting a planned two-stent technique for true bifurcation lesions (defined as lesions with significant stenosis in both the MB and SB7), one consistent difference is that the two-stent technique is associated with longer fluoroscopy times and higher contrast loads.8 The totality of data suggests that the decision on performing a bifurcation PCI with one versus two stents should be made on a case-by-case basis depending on patient anatomy.9
Given the variability in technical approaches to bifurcation lesions and the risk of side branch occlusion, several methods have been developed to risk-stratify bifurcation lesions. The RESOLVE score risk-stratifies patients with bifurcation lesions by using six qualitative measurements (Table 1).10 A RESOLVE score greater than or equal to 10 was deemed to be high-risk, and it was found that 17.5% of these patients had a SB occlusion occur during the PCI to treat their lesions.10 The V-RESOLVE score, where the same characteristics (except for TIMI Flow) are visually estimated by coronary CT angiography (CCTA) has been shown to be just as accurate as the RESOLVE score.3
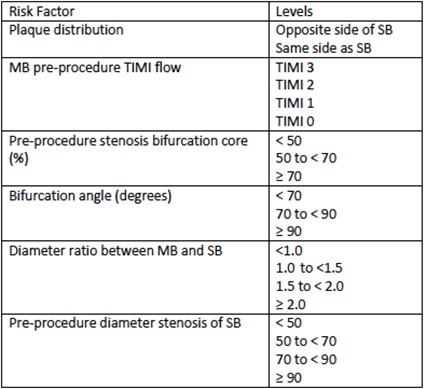
Table 1: Components of RESOLVE Score10 (MB = main branch; SB = side branch; TIMI = Thrombolysis in Myocardial Infarction)
Some of the parameters used in the V-RESOLVE score (e.g. the diameter stenosis of the bifurcation core) are difficult to obtain without advanced software which may limit availability of full evaluation in some centers. Studies have also looked for associations between individual CCTA characteristics, such as the takeoff angle, and the risk of complications. It should be noted, the takeoff angle is defined as the angle between the proximal main vessel and the side branch, whereas the bifurcation angle (which is the measurement used in the RESOLVE and V-RESOLVE scores) is defined as the angle between the distal main branch and the side vessel (Figure 1).11 One study showed that patients with a takeoff angle greater than 152 degrees between the left main (LM) artery and left anterior descending (LAD) artery had a greater incidence of target lesion failure following bifurcation PCI with the two-stent technique.5 A second study found that wider takeoff angles between the LM and left circumflex (LCX) arteries were associated with lumen loss at the ostium of the LCX during PCI.12
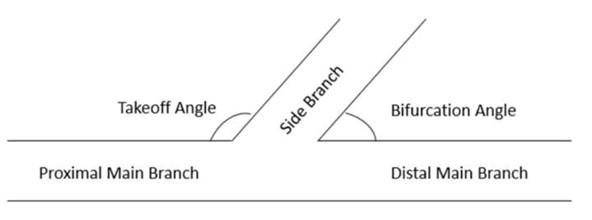
Figure 1: Diagram depicting takeoff and bifurcation angles.
Compared to the LM bifurcation, data using single lesion characteristics to predict outcomes in LAD-diagonal artery bifurcation PCIs are lacking. Here we present a case-based review of CCTA characterization of LAD-Diagonal bifurcation lesions and occurrence of complications during PCI.
Methods
In this study, we utilized three easily obtained CCTA characteristics (plaque distribution, bifurcation angle, and the degree of stenosis of the side branch) to predict the risk of complications in a case series of ten patients with LAD-diagonal artery bifurcation lesions. Images were analyzed by two authors (VM, SR) using AW 4.7 CCTA Workstation (GE Healthcare, Chicago, Illinois). Plaque distribution was defined as having plaque on either the same or opposite MB vessel wall as the SB ostium. Side branch stenosis was defined qualitatively as either a less than or greater than 50% stenosis. Patients with bifurcation lesions involving either the first diagonal artery (D1) or the second diagonal artery (D2) were included. Periprocedural complications reported included acute closure, plaque shift with severe stenosis or impaired flow in the SB following MB treatment or periprocedural myocardial infarction based on clinical documentation and angiographic data. Institutional review board approval for this retrospective study did not require individual informed consent.
Results
A summary of the cases is provided in Table 2 including bifurcation lesion characteristics and acute procedural complications. All cases were treated with provisional management of the bifurcation SB with the exception of Case 5 which was treated with an upfront two stent technique. Two patients experienced procedural complications. One (Case #4) was noted to have plaque shift with severe stenosis and TIMI II flow after MB stent deployment. This required provisional angioplasty of the D1 ostium. The second (Case #10) had a plaque shift into the ostium of D1 following MB stenting of the LAD. This required rewiring and conversion to a two-stent bifurcation strategy. Both cases with complications had narrow bifurcation angles (14 and 30 degrees, respectively) and MB plaque adjacent to the SB origin though SB stenosis was not severe.
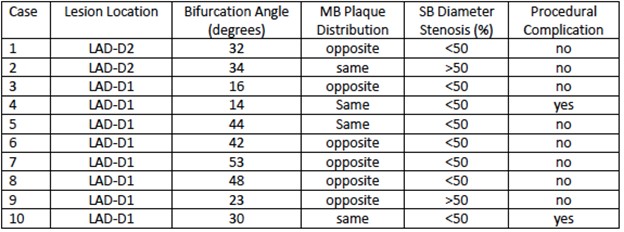
Table 2: Summary of case bifurcation lesion characteristics (LAD = left anterior descending; D1 = first diagonal; D2 = second diagonal; MB = main branch; SB = side branch).
Case 1: A 47 year-old patient with unstable angina and anterior T-wave inversions on electrocardiography (ECG) underwent CCTA demonstrating an LAD-D2 bifurcation lesion with 70-99% LAD stenosis and a less than 50% stenosis of the D2 artery. The LAD plaque was on the opposite vessel wall from the D2 ostium, and the LAD-D2 bifurcation angle was 32 degrees (Figure 2). Invasive angiography demonstrated concordant findings and the patient underwent MB stenting across the origin of D2 without complication.
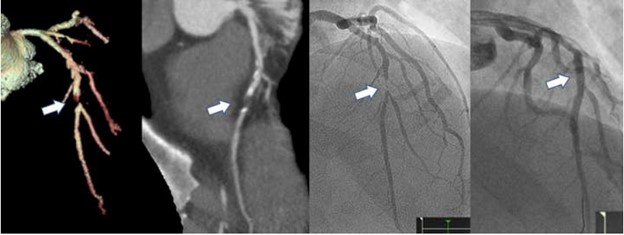
Figure 2: Select imaging from Case 1 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 2: A 74-year-old patient with unstable angina and ECG with anterolateral nonspecific changes underwent CCTA. Noninvasive imaging showed a LAD-D2 bifurcation showed an LAD-D2 bifurcation 50-70% stenosis in the mid LAD with a greater than 50% stenosis of the D2 ostium (Figure 3). The LAD plaque on the adjacent wall to the D2 ostium, and the LAD-D2 bifurcation angle was 34 degrees. Invasive angiography demonstrated the severe 70% mid LAD stenosis across the origin of D2 with only mild D2 disease. PCI of the mid LAD was performed with minimal plaque shift into the D2 branch without complication.

Figure 3: Select imaging from Case 2 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 3: A 52-year-old patient with limiting angina pectoris had CCTA imaging showing a LAD-D1 bifurcation lesion. There was 70% stenosis of the proximal LAD and mild stenosis (<50%) at the origin of the D1 branch. The LAD plaque was on the opposite vessel wall from the D1 ostium, and the LAD-D1 bifurcation angle was 16 degrees (Figure 4). The patient underwent a coronary catheterization, where a PCI was performed on the LAD with a 3.5 mm stent placed across D1. There were no periprocedural events and plaque shift at the D1 ostium and the branch retained normal flow.
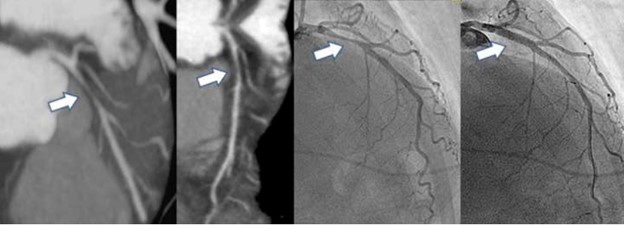
Figure 4: Select imaging from Case 3 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 4: A 56-year-old patient underwent an outpatient CCTA due to a several month history of exertional angina and dyspnea. CCTA showed an LAD-D1 bifurcation lesion with 70% stenosis of the LAD and a less than 50% stenosis of the ostial D1 artery (Figure 5). The LAD plaque was on the adjacent wall to the D1 ostium, and the LAD-D1 bifurcation angle was narrow (14 degrees). Invasive angiography demonstrated a diffuse 80% stenosis in the mid-LAD. After angioplasty, a 4.0 mm stent was deployed in the LAD across the D1 origin. There was a plaque shift resulting in a residual 80% ostial D1 stenosis with TIMI II flow, requiring angioplasty to restore normal flow and leaving a residual 30% stenosis.
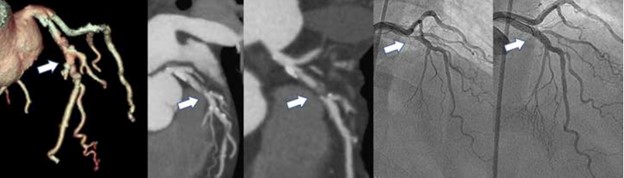
Figure 5: Select imaging from Case 4 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 5: A 58-year-old patient with cardiomyopathy underwent outpatient CCTA as part of the ischemic work-up. CCTA showed an LAD-D1 bifurcation lesion with 50-70% stenosis of the LAD and a less than 50% stenosis of the D1 artery (Figure 6). The LAD plaque was on the wall adjacent to the D1 ostium, and the LAD-D1 bifurcation angle was 44 degrees. Invasive angiography showed an 80% mid LAD stenosis with severe diffuse proximal disease involving origin of the D1 SB. The stenosis in the D1 SB was more severe than had been demonstrated on the CCTA. PCI was performed with angioplasty to the LAD, rotational atherectomy of the D1 branch and definitive bifurcation stenting using the DK-crush technique.
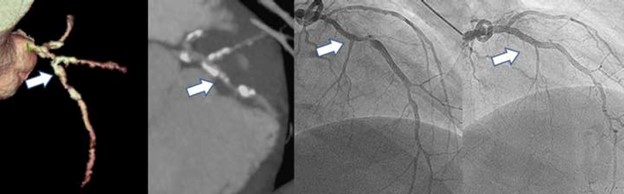
Figure 6: Select imaging from Case 5 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 6: A 60-year-old patient with severe heart failure underwent an outpatient CCTA for an ischemic evaluation of his cardiomyopathy. CCTA showed an LAD-D1 bifurcation lesion with a 70% stenosis of the LAD and a less than 50% stenosis of the D1 artery (Figure 7). The LAD plaque was on the opposite vessel wall from the D1 ostium, and the LAD-D1 bifurcation angle was 42 degrees. Invasive angiography demonstrated a diffuse 75% stenosis of a large LAD with mild disease of the D1 artery. PCI to the LAD was performed with angioplasty and deployment of a 4.0 x 18 mm stent from the origin of the D1 artery. The LAD had 0% residual stenosis and the diagonal SB was not compromised.
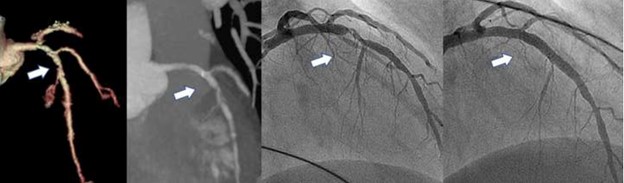
Figure 7: Select imaging from Case 6 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 7: A 58-year-old patient with longstanding heart failure (ejection fraction 25-30%) underwent an outpatient CCTA for an ischemic evaluation of her cardiomyopathy. CCTA showed a diffuse 50-70% stenosis LAD-D1 bifurcation lesion with less than 50% stenosis of proximal D1 artery (Figure 8). The LAD plaque was on the opposite vessel wall from the D1 ostium, and the LAD-D1 bifurcation angle was 53 degrees. Invasive angiography showed a diffuse subtotal stenosis in the mid LAD and mild disease of the D1 SB. The D1 sidebranch was wire-protected during LAD PCI and the lesion was treated provisionally with LAD stenting across the SB origin.
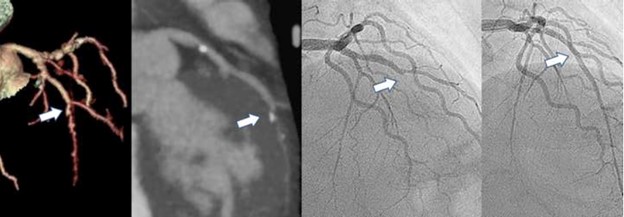
Figure 8: Select imaging from Case 7 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 8: A 54-year-old patient with severe cardiomyopathy and angina had CCTA imaging that showed an LAD-D1 bifurcation lesion with long proximal occlusion of the LAD and less than 50% stenosis of the D1 SB (Figure 9). The LAD plaque was on the opposite vessel wall from the D1 ostium, and the LAD-D1 bifurcation angle was 48 degrees. Invasive angiography demonstrated a long subtotal occlusion of the proximal LAD, a 20% stenosis of the distal left main coronary artery, and a 60% stenosis of the proximal ramus and a high-grade lesion of the RCA. The patient was deemed a poor surgical candidate, and underwent PCI to the LAD with antegrade wiring, atherectomy and stenting with provisional management of the D1 SB. The relatively small D1 had mild stenosis and normal flow after PCI.
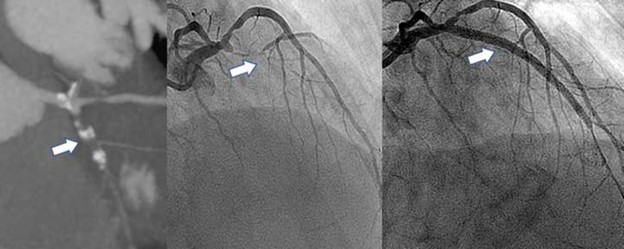
Figure 9: Select imaging from Case 8 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 9: A 54-year-old patient with cardiomyopathy and angina underwent CCTA that demonstrated an LAD-D1 bifurcation lesion with a 70-80% stenosis of the LAD and a greater than 50% stenosis of the D1 artery. The LAD plaque was on the opposite vessel wall from the D1 ostium, and the LAD-D1 bifurcation angle was 23 degrees (Figure 10). Invasive angiography showed a 70-80% proximal LAD stenosis adjacent to the origin of the severely diseased D1 SB. PCI was performed with angioplasty and stenting of the LAD with provisional management of the SB which had persistent 70% stenosis but retained normal flow.

Figure 10: Select imaging from Case 9 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Case 10: A 49-year-old patient with angina, peripheral arterial disease and mild cardiomyopathy was referred after CCTA showed an LAD-D1 bifurcation lesion with a 60-70% stenosis of the proximal to mid LAD and a less than 50% ostial stenosis of the D1 artery (Figure 11). The LAD plaque was on the same vessel wall as the D1 ostium, and the LAD-D1 bifurcation angle was 30 degrees. Angiography demonstrated a long 70% proximal LAD lesion extending past the take-off of the prominent D1 branch with had 30% ostial stenosis. The LAD was treated with PCI and stenting resulting in plaque shift into the D1 branch, a severe SB stenosis, chest pain and impaired flow. This required conversion to a two-stent strategy to restore flow in the D1 SB.

Figure 11: Select imaging from Case 10 CCTA, invasive angiography, and PCI (LAD bifurcation lesion denoted by arrow).
Discussion
In summary, these ten patients had LAD-diagonal bifurcation disease first characterized on CCTA prior to invasive angiography. Four patients had the high-risk feature of plaque in the LAD on the vessel wall adjacent to the ostium of the diagonal SB. Two patients had the high-risk feature of a greater than 50% stenosis of the diagonal SB origin. The average bifurcation angle of the diagonal branches was 31 degrees. Interestingly, all our patients had a bifurcation angle under 70 degrees on CCTA. Per the RESOLVE score, such bifurcation angles are associated with the lowest risk of procedural complications.10 This narrow bifurcation angle may facilitate PCI of LM bifurcations but, in fact, predispose to SB closure in the context of smaller diagonal branches where an upfront two-stent technique may not be desired.
Based on observations from our study, the data showing an association of larger takeoff angles (and smaller bifurcation angles) with complications in LM bifurcation lesions may be applicable to LAD-diagonal lesions identified on CCTA. The two patients who had procedural complications in our study (Case 4 and Case 10) had bifurcation angles of 14 and 30 degrees, respectively, which were both less than the mean bifurcation angle of 31 degrees. Since the takeoff angle and bifurcation angle are approximately supplementary angles to one another, the sum of a takeoff angle and bifurcation angle for any vessel bifurcation should equal approximately 180 degrees. Therefore, as a bifurcation takeoff angle increases, its bifurcation angle should decrease, and vice versa. Since Case #4 and Case #10 had smaller than average bifurcation angles, it can be inferred that they had larger than average takeoff angles. Therefore, it is reasonable to conclude that this data has similar applicability to LAD-diagonal bifurcations as it does to LM-LAD and LM-LCX bifurcations.
It is intuitive that LAD plaque on the opposite vessel wall from the diagonal artery ostium lowers the likelihood of plaque shift and procedural complications related to the SB. In this review, only patients with LAD plaques on the same vessel wall as the diagonal artery ostium experienced complications. Interestingly, when comparing how the three CCTA components we utilized are weighted in the RESOLVE Score, the plaque distribution had the least amount of weight, implying the least association with complications (one point for plaque present on the vessel wall adjacent to the SB ostium versus six points for a bifurcation angle greater than 90 degrees or four points for a 50-70% side vessel stenosis). It should be noted that neither of the two patients with greater than 50% stenosis of the diagonal arteries (Case 2 and Case 9) experienced procedural complications.
The three lesion characteristics included in this study are easily obtained from image reconstructions and reflect the substantial additive information obtained from CCTA prior to invasive angiography. Additional analysis can further add to procedural preparation. Incorporating plaque characteristics such as the presence of calcified or low attenuation plaque in the MB and SB have been reported to be additive to the RESOLVE score with regard to prediction of SB occlusion.13
There were several limitations to our study. The first limitation is the small number of cases we were able to report. Given that only ten patients were included and only two of them had angiographic complications, statistical analysis was not able to be performed to determine if these three variables alone can predict procedural outcomes. A second limitation is that the study only included patients undergoing PCI for stable coronary disease and unstable angina Thus, these findings may not be applicable to patients with acute myocardial infarctions, since none were included in our study (although, such patients generally do not undergo CCTA prior to invasive angiography). The non-emergent nature of these patients’ PCIs may have contributed to their relatively uncomplicated procedures and stable post-procedure courses. To this point, the previously mentioned study that determined a LM-LAD takeoff angle above 152 degrees is associated with procedural complications included patients presenting with STEMIs (6.3%), NSTEMIs (10.1%), unstable angina (47.4%), and only a minority of patients with stable disease.5
As utilization and availability of CCTA continue to increase, this modality will have a progressively more important gatekeeper role prior to invasive angiography. Detailed analysis of computed tomography is the standard for structural heart and complex electrophysiology procedures. In contrast, data from CCTA is not routinely leveraged beyond its use in the binary decision of whether to pursue invasive angiography.14 Pre-procedure CCTA-based fractional flow reserve of individual lesions, chronic total occlusion PCI planning, and assessment of lesion length or calcification have received increased attention. However, use of simple bifurcation lesion data to plan PCI or predict complications is not a routine part of the interventional workflow. There is now randomized data proving the value of pre-angiography CCTA in patients with prior coronary artery bypass grafting.15 Routine application of CCTA data into bifurcation PCI may provide similar patient- and procedure-level benefits.
Conclusions
This report demonstrates the application of three easily-obtainable lesion characteristics of LAD-diagonal bifurcations with a series of case examples. The incorporation of CCTA-derived plaque location, bifurcation angle and degree of diagonal branch stenosis into the interventional workflows may be useful in improving procedural efficiency and reducing complications related to SB occlusion.
Statement Regarding Ethics and Integrity Policies:
This data has not been published elsewhere. No outside funding was used for this study. None of the authors have any conflicts of interest to disclose. All patient information was anonymized. No material was reproduced from other sources. This case series was not a clinic trial, and thus there is no clinical trial registration.
Acknowledgements
Authorship:
Christopher Armenia MD: data gathering and analysis, drafting of the manuscript.
Venkat Manubolu MD: Critical revision, data gathering and analysis, image acquisition
Sion Roy MD: Study conception and design, critical revision.
Joseph Thomas MD: Study conception and design, image acquisition, critical revision.