Clinical Cardiology Interventions
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2836-077X | Journal DOI: 10.61148/2836-077X/JCCI
Murat ÇAKIR* , Eftal Murat BAKIRCI, Hüsnü DEĞİRMENCİ
Erzincan Binali Yıldırım University, Faculty of Medicine, Department of Cardiology Erzincan/Turkey
*Corresponding Author: Murat Çakır, Erzincan Binali Yıldırım University, Faculty of Medicine, Department of Cardiology Erzincan/Turkey
Received date: April 15, 2021
Accepted date: April 20, 2021
published date: April 26, 2021
Citation: ÇAKIR M, Eftal M BAKIRCI, DEĞİRMENCİ H. (2021) “Current Approach to Coronary Artery Perforations.” J Clinical Cardiology Interventions, 2(3); DOI: http;//doi.org/04.2021/1.1015
Copyright: © 2021 Murat Çakır. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Percutaneous coronary intervention technique is widely used today in the treatment of acute coronary syndromes. The incidence of percutaneous coronary intervention complications is less than 1% in randomized studies. The high mortality and morbidity rates in percutaneous coronary interventions made it necessary to improve current treatment methods in the treatment of complications that may occur. In this article, we presented the current approach to coronary artery perforations.
Introduction
Coronary artery perforation is generally defined as a fistula involving all the intima, media and adventitia layers of the vessel wall after a mechanical trauma. Coronary perforation has been reported as 0.3-0.6% in current records(1,2). With the development of coronary intervention devices such as transluminal extraction coronary atheroctomy, directional coronary atherectomy, laser coronary angioplasty, and high-speed mechanical rotational atherectomy, these complications have become more common(3). Although coronary artery perforations are rare, they can cause fatal consequences if they are not acted quickly. Today, with advanced equipment and sufficient operator experience, the treatment and follow-up of coronary artery perforations can be done successfully.
Risk Factors
With the development of interventional techniques in coronary artery occlusions, methods such as extra-ionic coronary atheroctomy, laser coronary angioplasty, mechanical rotational atheroctomy, microcatater use, intravascular ultrasonography (IVUS) have been used frequently(3). With the use of these methods, an increase in the incidence of coronary perforations is observed. There are multiple parameters that increase the risk of coronary artery perforations. Other factors that increase the risk of coronary perforation; advanced age, female gender, Use of rigid and hydrophilic guidewires, rigid catheters, location of the lesion in the tortuous area of the vessel, chronic total occlusions, bifurcation lesions, complex lesions (ACC / AHA type B2 or C) and balloon / vessel diameter can be counted as having the rate above 1.1(4,5).
Coronary Perforations Types
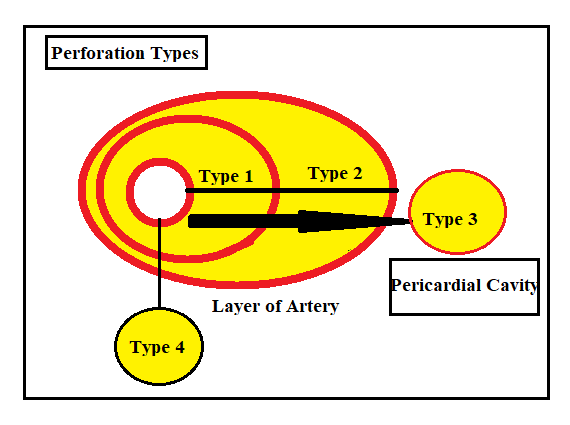
With the widespread use of coronary artery invasive interventions and the increase in the incidence of complications, there has been a need for a universal classification of coronary perforations(6). In the multicenter study conducted by Ellis et al, which included approximately 13,000 patients, coronary perforation types were evaluated in 3 groups. The type of Type 3, which is poured into the cavity as a subgroup later, has been revealed. This type, also called type 3 CS (cavity spilling) or type 4, is defined as the discharge of blood into the left ventricle, coronary sinus or other anatomical spaces. Type 5 is the type expressed as the perforation of the distal arteries seen with the widespread use of hydrophilic wires(7,8) (Figure 1,Figure 2)
Figure 1.
|
Types of coronary artery perforation-Ellis Classification(8) |
|
|
Type 1 |
Extraluminal crater formation in the vessel wall without extravasation |
|
Type 2 |
Contrast staining of epicardial fat tissue or myocardium without monitoring jet extravasation |
|
Type 3 |
Secondary to the coronary perforation, the contrast material > 1 mm more pericardial area. |
|
Type 4 - CS(cavity spilling) |
Contrast material draining into the left ventricle, coronary sinus or other anatomical spaces |
|
Type 5 |
Distal artery perforation |
Figure 2.
Prognosis and Management of Coronary Perforations
The prognosis of coronary perforations is particularly closely related to early diagnosis and treatment. With the attention and rapid movement of the operator, the amount of blood that goes out of the vein can be controlled.This makes a significant positive contribution to the patient's mortality and morbidity.
Another important factor in mortality during coronary interventions is the type of perforation. In type 1 and 2 perforations, local balloon applications and close transthoracic echocardiographic follow-up can spontaneously be limited within 24 hours, while type 3 perforations can become dramatic and death becomes inevitable if they are not treated early. While the incidence of cardiac tamponade and myocardial infarction in all types of perforation is 20.8% and 19.3%, this rate increases specifically in Type 3 coronary perforations and increases to 45.7% and 36.3%, respectively. Mortality rate is 21.2% in type 3 perforations(8,9).
In case of coronary perforation, the patient develops a hemodynamically unstable condition accompanied by hypotension and bradykadiia. With the rapid spread of blood from the vessel wall to the pericardial area, cardiac tamponade occurs in the patient. Later, this situation is followed by myocardial ischemia and cardiogenic shock and the patient is arrested within minutes or even seconds. There are differences in the treatment method and algorithm according to the coronary perforation type and location(10) (Figure 3).
In the treatment of coronary perforations, the type of perforation significantly affects the type of treatment to be chosen. As mentioned above, while perforation is self-limiting with balloon application in type 1 and type 2 perforations, other treatment methods such as graft-covered stent application, fat and spiral wire embolization, although less frequently, are required in type 3 perforations(10,11).
Another issue in determining the method and method of treatment is the location of the perforation. Graft-covered stent or double stent application may be considered in proximal vessel perforations, since it will be more difficult to limit itself.
In distal vessel perforations, it is the condition that is mostly caused by a guide wire, and perforation is self-limiting with balloon dilatation, fat embolization, autologous blood embolization, spiral wire embolization, microcoil, gelfoam and thrombin applications(12).
Figure 3.
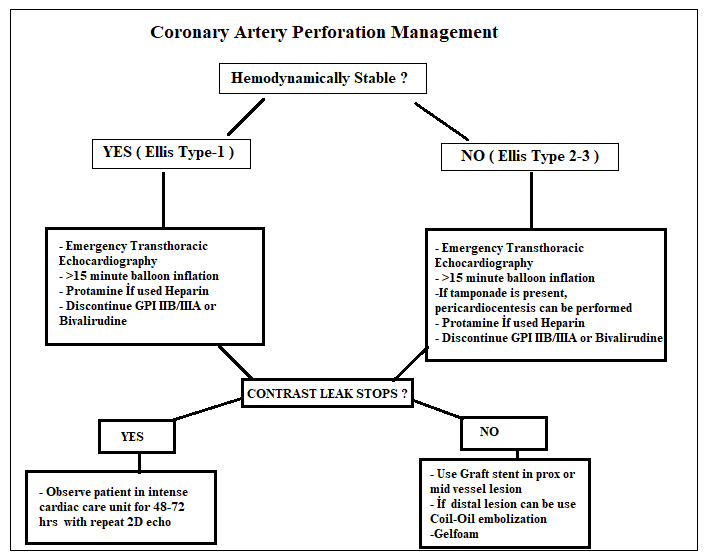
In type 1 perforations, the first thing to do is to determine the hemodynamics of the patient and to determine whether cardiac tamponade has developed or not. If cardiac tamponade has developed, inflation of the conventional balloon or perfusion balloon for 15 minutes using the antegrade route should be considered in order to limit the blood flow from the perforation area to the pericardial area. The balloon should be left in its place and the blood accumulated in the pericardial area should be drained by using the transthoracic echocardiography method and hemodynmic stabilization should be provided. The patient should be given a rapid intravenous fluid replacement and evaluated for red blood, fresh frozen plasma, and cryoprecipitate. During this period, anticoagulant drugs administered to the patient should be discontinued (glycoprotein 2b / 3a, iv heparin), in order to reduce and reverse the effect of heparin, protamine sulphate should be given intravenously at 1 mg per 100 units, and the activated clotting time should be closely monitored(3, 10-13).
Polytetrafluoroethylene (PTFE) stents may be preferred for type2 and type3, especially proximally located, suitable perforations. However, these stents contain difficulties in terms of use, especially due to early calcification, high risk of restenosis, occlusion of the side branch mouth, and the interventional need for a 7 French catheter. There are different types of graft covered stents and catheter widths for using these types. This is discussed in Figure 4.
A special method called ping-pong method is used for the application of graft covered stents and double layer stents. In this method, a 7F sheat should be opened through a femoral path separate from the current catheter path of the patient, then using this route, the 7F catheter is reached to the vein osteal, and a separate guide wire is passed under the inflated balloon at the perforation point. Afterwards, the balloon is inflated and the graft covered stent is loaded on the guide wire in the existing 2 guiding catheters and the stent is brought up to the area where the inflated balloon is located. Subsequently, the balloon is lowered for a short time and the graft-covered stent brought to the perforation area is inflated at high pressure to close the perforation area(3).
Both balloon and graft covered stents pass through the 8 French catheter. While graft covered stents are often recommended to be used in proximal and over 2 mm vascular perforations, there are case reports used in patient groups who do not benefit from other treatment methods in distal perforations. Fat embolization, autologous clot use, coil embolization and gelfloam should be considered in the foreground in perforations of less than 2 mm and distal vessels(3,11).
Figure 4.
|
CORONARY STENT GRAFT SYSTEM |
||||
|
Trade names |
Stent graft diameter (mm) |
Stent graft diameter (mm) |
Minimum deployment (nominal) and rated burst pressure |
Guide catheter |
|
Graftmaster Rx Coronary Stent Graft System (Abbott Vascular) |
2.8 3,5 4,0 4,5 4,8 |
16, 19, 26 16, 19, 26 16, 19, 26 16, 19, 26 16, 19, 26 |
15/16 ATM 15/16 ATM 15/16 ATM 15/16 ATM 15/16 ATM |
6 Fr 6 Fr 6 Fr 7Fr 7Fr |
|
Pk Papyrus |
2,5 3,0 3,5 4,0 4,5 5,0 |
15,20 15,20,26 15,20,26 15,20,26 15,20,26 15,20,26 |
8/16 ATM 8/16 ATM 8/16 ATM 8/16 ATM 8/16 ATM 8/16 ATM |
5Fr 5Fr 5Fr 5Fr 6 Fr 6 Fr
|
|
Jostent Coronary Stent Graft |
2,75-5,0 |
9-26 |
11/28 ATM |
6Fr <3,5 mm 7Fr > 3,5 mm |
|
Direct-Stent Insitu Technologies |
2.25–6.0 |
10–38 |
12/18 ATM |
6Fr, 7Fr |
|
Aneugraft Dx ITGI Medical |
2.5–4.0 |
13–27 |
10/16 ATM |
6Fr |
Conclusion
Increasing the frequency of use of interventional methods in complex coronary lesions resulted in similar complications. Although rare, coronary perforations can still result in high mortality rates today. Working to minimize the risk before the treatment of coronary perforations will help us in minimizing mortality. Especially, a comprehensive investigation of the patient's blood picture before the procedure, revealing of chronic diseases, reducing the use of hydrophilic wires in complex calcific tortuous lesions, determining the interventional techniques well and being prepared as equipment and personnel against possible complications will provide us great convenience in terms of preventing the potentially fatal outcome.