Pharmacy and Drug Innovations
OPEN ACCESS | Volume 4 - Issue 1 - 2025
ISSN No: 2994-7022 | Journal DOI: 10.61148/2994-7022/PDI
Sudireddy Rajini1*, B.S.Venkateswarlu2 , R.Marget chandira3
1Research Scholar, Vinayaka Missions Research Foundation, Salem, Tamilnadu, India- 636008.
2Professor cum Principal, Department of Pharmaceutics, Vinayaka missions College of Pharmacy, Vinayaka Missions Research Foundation, Salem, Tamilnadu, India- 636008.
3Professor, Department of Pharmaceutics, Vinayaka missions College of Pharmacy, Vinayaka Missions Research Foundation, Salem, Tamilnadu, India- 636008
*Corresponding author: Sudireddy Rajini, Research Scholar, Vinayaka Missions Research Foundation, Salem, Tamilnadu, India- 636008.
Received: December 03, 2021
Accepted: December 14, 2021
Published: December 16, 2021
Citation: Sudireddy Rajini, B.S.Venkateswarlu, R.Marget chandira (2021) “Prospective Study of Antibiotics Utilization in Pulmonology Department”. J Pharmacy and Drug Innovations, 3(2); DOI: http;//doi.org/12.2020/1.1042.
Copyright: © 2021 Sudireddy Rajini. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Respiratory tract infections remain the major cause of morbidity from acute illness and most likely represent the single most common reason patients seek medical attention. This project focuses on bacterial infections involving the lower respiratory tract, which includes the larynx trachea bronchi and lung parenchyma. This study was prospective observational study in Pulmonology department Andhra Pradesh, India The study was conducted from October -2020 to March -2021 in Various hospitals in Andhra Pradesh. In our study, among 335 patients, 220 (65.67%) were Males and 115 (34.32%) were Females. The highest number of cases observed were Pulmonary Tuberculosis are 153 patients (45.67%), followed by COPD are 87 patients (25.9%), Pneumonia are 42 patients (12.53%), Pleural effusion cases are 39 patients (11.64%), and Bronchiectasis cases are 14 patients (4.17%).The results revealed that Therapeutic evaluation of various antibiotics from our case studies we could observe that the most frequently prescribed antibiotics are higher percentage of patients using Cephalosporin’s (51.14%) followed by Macrolides (17.09%), Metronidazole (12.58%), Penicillin’s (7.66%), Aminoglycosides (3.41%), Doxycycline (3.41%), Fluoroquinolones (3.27%), Carbapenems (1.30%) .LRTI usually causes minor illness, but may result in significant morbidity and mortality. Better lay and professional awareness of the often prolonged course of LRTI may improve understanding and appropriate use of antibiotics..In this study the Health care professionals are increase the awareness for improving quality of life in critically ill LRTIs patients and preventing further complications.
Introduction
Pneumonia is an infection of lungs affecting primarily the small air sacs known as alveoli, distal airways and inter stitium of lungs .It is usually caused by viruses or bacteria and less commonly by other micro-organisms, certain medications and conditions like autoimmune diseases. The alveoli fill with fluid or pus, making it difficult to breath. Pneumonia is an infection in one or both lungs. Bacterial pneumonia is the most common type in adults (Streptococcus pneumonia).
Classification on pneumonia based on the location acquired
1.Community acquired pneumonia
2.Hospital acquired pneumonia
3.Ventilator associated pneumonia
4.Other types of pneumonia: Aspiration pneumonia[Hospital or Community]Health care associated pneumonia
Community Acquired Pneumonia: The IDSA defines CAP as “an acute infection of the pulmonary parenchyma that is associated with at least some symptoms of acute infection, accompanied by the presence of an acute infiltrate on a chest radiograph or auscultatory findings consistent with pneumonia (such as altered breath sounds and/or localized roles), in a patient not hospitalized or residing in a long term care facility for more than 14 days before onset of symptoms.
Hospital acquired pneumonia:
Hospital acquired (or nosocomial) pneumonia (HAP) is pneumonia that occurs 48 hours or more after admission and did not appear to be incubating at the time of admission.
Ventilator Associated Pneumonia: Ventilator associated pneumonia (VAP) is a type of HAP that develops more than 48 to 72 hours after endotracheal intubation.
Aspiration Pneumonia: It refers to the pulmonary consequences resulting from the abnormal entry of fluid, particulate exogenous substances, or endogenous secretions into the lower airways.
There are usually two requirements to produce aspiration pneumonia:Compromise in the usual defenses that protect the lower airways including glottis closure, cough reflex, and other clear mechanisms.An inoculum deleterious to the lower airways by a direct toxic effect, stimulation of an inflammatory process from a large enough bacterial inoculum, or obstruction due to a sufficient volume of material or particulate matter.
Healthcare- Associated Pneumonia: Healthcare-associated pneumonia (HCAP) is defined as pneumonia that occurs in a non-hospitalized patient with extensive healthcare contact, as defined by one or more of the following: Intravenous therapy, wound care and chemotherapy within the prior 30 days. Residence in a nursing home or other long term care facility. Hospitalization in a hospital for two or more days within the prior 90 days.
Attendance at an acute care hospital or hem dialysis clinic within the prior 30days.
Epidemology: According to the Global Burden of Disease (GBD) 2015 study, Chronic Obstructive Pulmonary Disease (COPD) and Lower respiratory tract infections (LRTIs) represent the third and fourth most common cause of death, respectively after ischemic heart disease and cerebro vascular disease.
LRTIs is a broad terminology which includes different diseases including Acute Bronchitis, Pneumonia, and acute exacerbation of chronic lung diseases such as COPD or Bronchiectasis.
Pneumonia in India can be fatal to all, but is especially dangerous. According to the world health organization (WHO), one in three deaths in India is caused by pneumonia.
The world health organization (WHO) estimated that about 1.6 million deaths annually are reported in adults aged over 59 years. Indian Burden of Disease accounts for 23% of the global pneumonia burden and 36% of the WHO regional burden.
The rates differ based on the age, with higher incidence observed in Patients between 65 and 79 years of age and >80 years of age.
A study of blood cultures in CAP revealed that: Streptococcus pneumonia (35.3%) as the commonest isolate, followed by Streptococcus aureus (23.5%), Klebsiella pneumoniae (20.5%), and Haemophilus influenza (8.8%).
Pneumococcal Pneumonia is the most common cause of mortality due to lower respiratory infections.
According to the GBD 2015 study pneumococcal pneumonia is the most common cause of pneumonia responsible for over 15 lakh deaths across the world in 2015.
Community acquired pneumonia (CAP) and acute exacerbation of chronic bronchitis (AECB) are the two commonly encountered acute LRTIs. The annual incidence of CAP is about 5-11 per 1000 population with higher rates reported in the elderly population.
Methodology
Study Site: Government Fever Hospital, Guntur
Study Design: Single-centre, Prospective, Observational study.
Study Period: 6 Months
Study criteria:
Inclusion criteria:All adult in-patients of age >18 years diagnosed with lower respiratory tract infections.
Patients who are willing to participate in the study.
Exclusion criteria: Below 18 years of age and pregnant women.
Patients who are not willing to participate in the study.
Sample Size: 335
Sources Of Data: Inpatients records of the patients in male and female wards. Medical records department.
Data collection form contents:Patient’s demographic details
Chief complaints
Past medical history
Past medication history
Social history/habits
Breathing patterns
Adventious Sounds
Comorbid conditions
Chest X-ray
Complete blood count
Sputum test
Final diagnosis
Treatment plan
Study Method: Study was conducted by selecting patients who are diagnosed to have lower respiratory tract infections.As pulmonary tuberculosis is the most common reason for hospitalization so priority has been given to pulmonary tuberculosis rather than respiratory tract infections in general.Data collection form was designed.Data were reviewed from patient case sheets for therapeutic evaluation of various antibiotics, patient’s demographic details, Past medical history, Past medication history, Social history, Family history, Chief complaints, co-morbid conditions, Laboratory investigations such as complete blood picture, chest x-ray, sputum testing, pleural fluid, Bronchoscopy.
Results and Discussion
Gender distribution:
In our study, among 335 patients, 220 (65.67%) were Males and 115 (34.32%) were Females.
|
S.No |
Gender |
No. of Patients |
Percentage |
|
1. |
Male |
220 |
65.67% |
|
2. |
Female |
115 |
34.32% |
|
Total |
335 |
100% |
|
Table 6: Gender Distribution
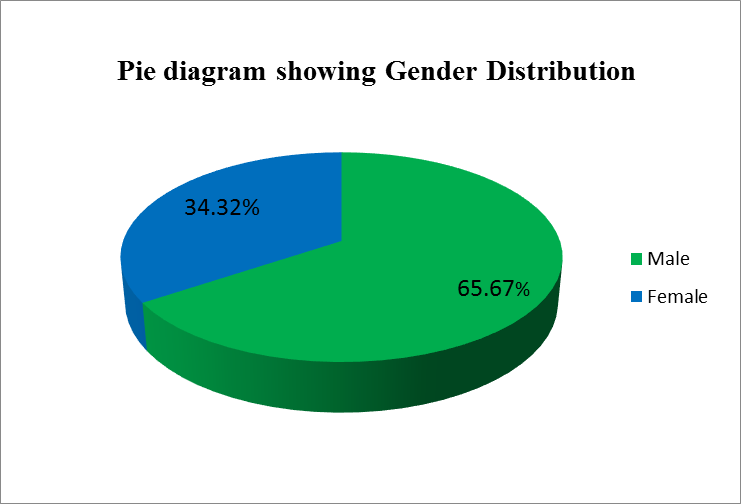
Figure 7: Gender Distribution of Patients
Age distribution with gender:
Higher percentage of our study population belonged to the age group of 41-65 years of age (54.62%), followed by 19-40 years of age (31.94%), and >65 years of age (13.43%).
|
S.No |
Age Group |
No. of patients |
Males |
Percentage |
Females |
Percentage |
|
1. |
19-40 |
107 (31.94%) |
55 |
16.41% |
52 |
15.52% |
|
2. |
41-65 |
183 (54.62%) |
133 |
39.70% |
50 |
14.92% |
|
3. |
> 65 |
45 (13.43%) |
32 |
9.55% |
13 |
3.88% |
Table 7: Age Distribution with Gender

Figure 8: Gender distribution of study population
Clinical Presentation of Patients:-
Among the Signs and Symptoms of Lower Respiratory Tract Infections (LRTIs) are Shortness of breath, Cough, Fever in majority patients followed by Chest pain, Hemoptysis.
|
S.NO |
Symptoms |
No. of Patients |
Percentage |
|
1. |
SOB |
265 |
33.3% |
|
2. |
Cough |
248 |
31.2% |
|
3. |
Fever |
148 |
18.6% |
|
4. |
Chest pain |
75 |
9.4% |
|
5. |
Hemoptysis |
36 |
4.5% |
|
6. |
Others |
18 |
2.2% |
Table 8: Clinical presentation of Patients
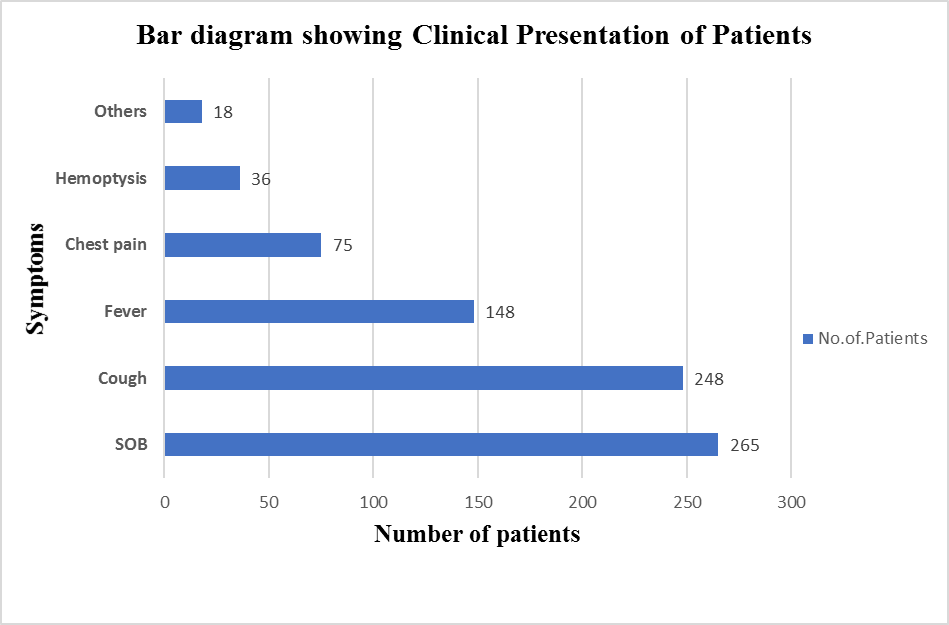
Figure 9: Clinical presentation of Patient
Lobar involvement based on chest x-ray:
In a majority of patients (42%) the Right lobe of the lung was involved.
|
S. No |
Chest x-ray Lobar involvement |
No. of patients |
Percentage |
|
1. |
Bilobar |
122 |
36.4% |
|
2. |
Right lobe |
141 |
42% |
|
3. |
Left lobe |
62 |
18.5% |
|
4. |
Normal |
10 |
2.9% |
Table 9: Lobar involvement based on chest x-ray
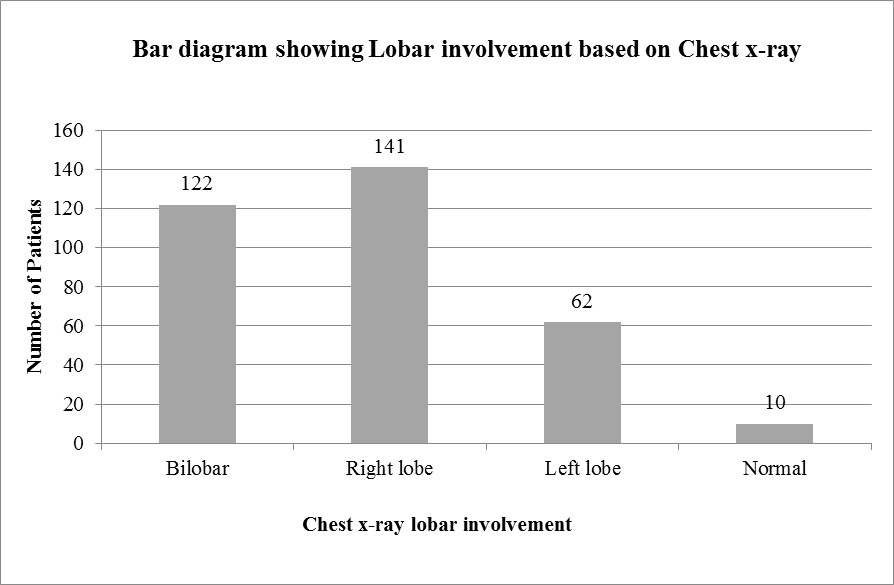
Figure 10: Lobar involvement based on chest x-ray
Sources of sample specimen:
|
Sample |
Sputum |
Pleural Fluid |
|
No of patients (n=335) |
296 |
39 |
Table 10: Sources of sample specimen
Figure 11: Sources of sample specimen
Types of diseases:
In our study population the total number of cases are 335. The highest number of cases observed were Pulmonary Tuberculosis are 153 patients (45.67%), followed by COPD are 87 patients (25.9%), Pneumonia are 42 patients (12.53%), Pleural effusion cases are 39 patients (11.64%), and Bronchiectasis cases are 14 patients (4.17%).
|
S.No. |
Types of infections |
No. of patients effected |
Percentage |
|
1 |
Pulmonary Tuberculosis |
153 |
45.67% |
|
2 |
Pneumonia |
42 |
12.53% |
|
3 |
Bronchiectasis |
14 |
4.17% |
|
4 |
COPD |
87 |
25.9% |
|
5 |
Pleural Effusion |
39 |
11.64% |
Table 11: Types of Diseases
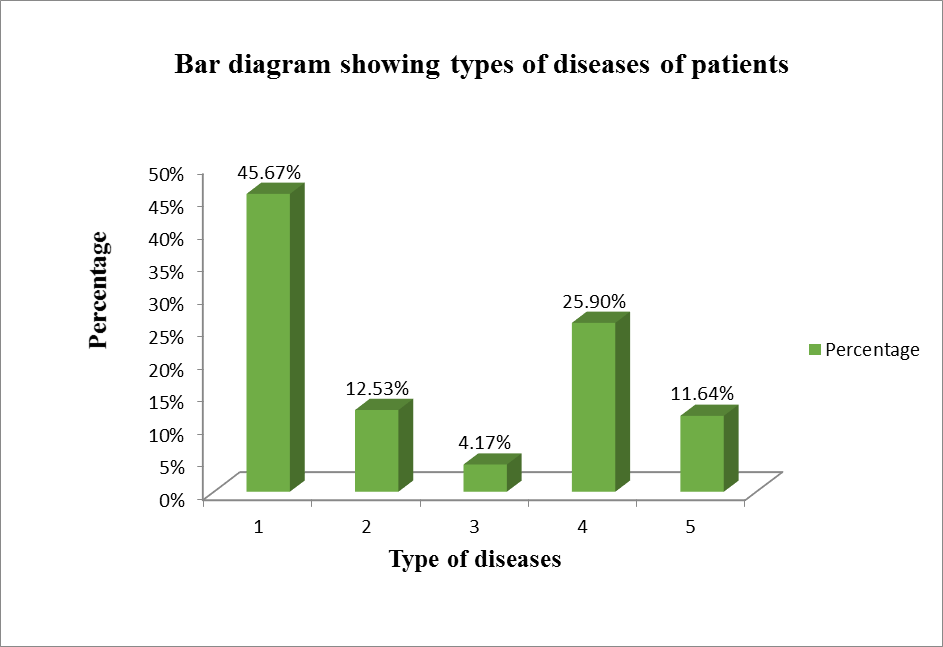 Figure 12: Types of diseases of patients
Figure 12: Types of diseases of patients
Life style of the study population:
Life style of the study population are listed in the below table. The results revealed that 29.55% of patients were having habit of both smoking and alcohol, 11.04% of patients were having habit of smoking alone, 5.97% of patients were having habit of alcohol alone, 53.43% of study population were found to be having none of these habits.
|
S.No |
Life Style |
Percentage (%) |
|
|
No addiction |
53.43% |
|
|
Smoke and alcohol |
29.55% |
|
|
Smoke alone |
11.04% |
|
|
Alcohol alone |
5.97% |
Table 12: Life style of study population
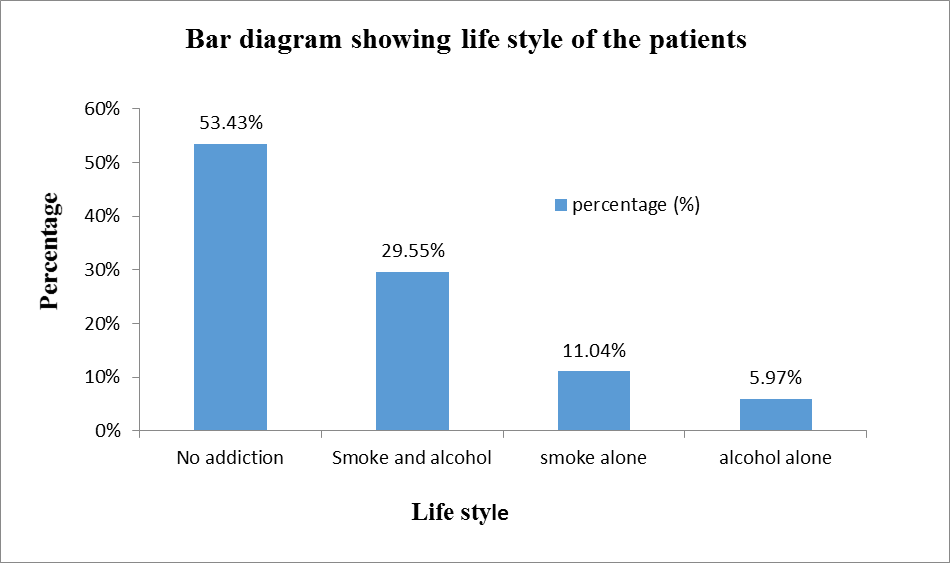
Figure 13: Life style of study population
Co-Morbid Conditions:-
The co-morbidities of study population are given in the above table. The results revealed that 13.43%
were HIV, 7.46% were Hypertension, 8.05% were Diabetes Mellitus, 4.17% were Asthma, 3.58%
were other comorbidities, and 63.28% were no comorbidities observed.
|
S.No |
Co-morbid conditions |
Number(n=335) |
Percentage (%) |
|
1. |
HIV |
45 |
13.43% |
|
2. |
Hypertension (HTN) |
25 |
7.46% |
|
3. |
Diabetes mellitus (DM) |
27 |
8.05% |
|
4. |
Asthma |
14 |
4.17% |
|
5. |
Other comorbidities |
12 |
3.58% |
|
6. |
No co-morbidities observed |
212 |
63.28% |
Table 13: Co-Morbid Conditions

Figure 14:- Co-morbidities of patients
List of antibiotics used:
|
Name of the Antibiotic |
No. of patients used |
Percentage |
|
Ceftazidime |
14 |
1.91 |
|
Metronidazole |
92 |
12.58 |
|
Ceftriaxone |
248 |
33.92 |
|
Cefixime |
102 |
13.95 |
|
Azithromycin |
125 |
17.09 |
|
Amoxiclav (Amoxicillin + Clavulanic Acid) |
56 |
7.66 |
|
Ciprofloxacin |
13 |
1.77 |
|
Doxycycline |
25 |
3.41 |
|
Cefotaxime |
10 |
1.36 |
|
Amikacin |
14 |
1.91 |
|
Meropenem |
10 |
1.30 |
|
Kanamycin |
11 |
1.50 |
|
Moxifloxacin |
11 |
1.50 |
Table 14: List of antibiotics used in LRTI’s
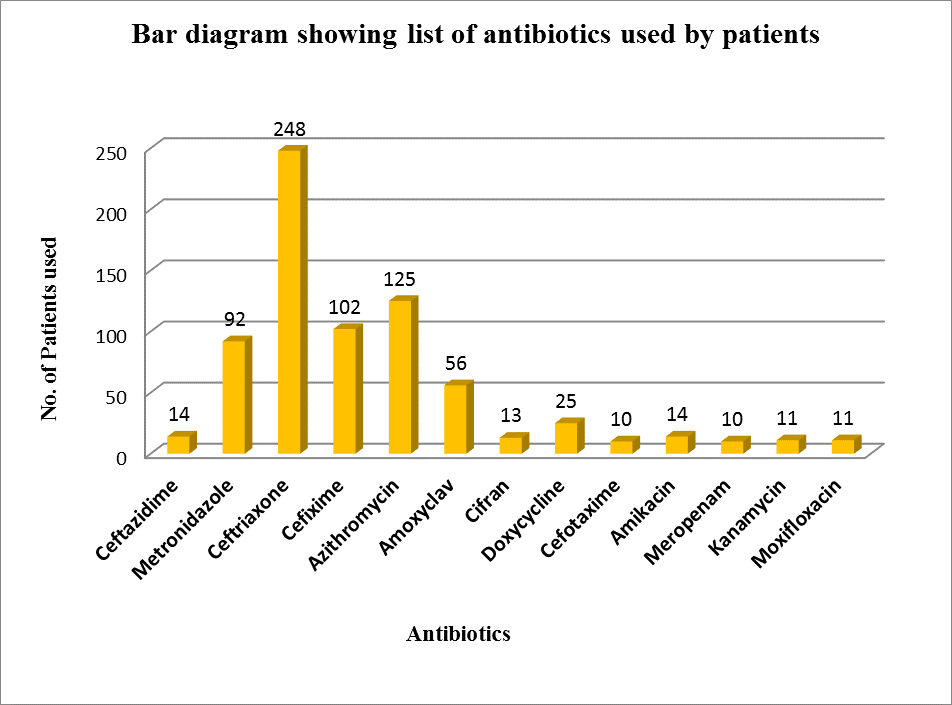
Figure 15:- List of antibiotics used by patients
|
|
Antibiotics |
Percentage |
||
|
Beta lactams
|
Penicillins |
Amoxiclav |
7.66% |
|
|
Cephalosporins |
Ceftriaxone |
51.14% |
||
|
Cefixime |
||||
|
Ceftazidime |
||||
|
Cefotaxime |
||||
|
Carbapenems |
Meropenem |
1.30% |
||
|
Macrolides |
Azithromycin |
17.09% |
||
|
Fluoroquinolones |
Ciprofloxacin |
3.27% |
||
|
Moxifloxacin |
||||
|
Aminoglycosides |
Amikacin |
3.41% |
||
|
Kanamycin |
||||
|
Others
|
Tetracycline |
Doxycycline |
3.41% |
|
|
Nitroimidazoles |
Metronidazole |
12.58% |
||
Table 15: Classification of antibiotics used by patients
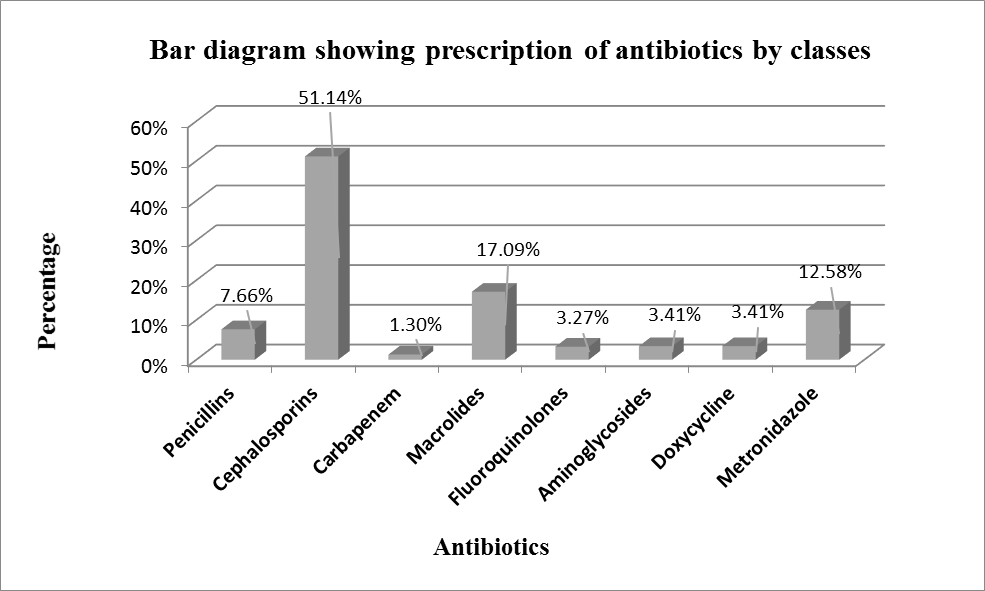
Figure 16:- Classification of antibiotics used by patients
|
Category of Treatment |
Name of the drug |
No of patients used |
|
Category I |
Isoniazid + Ethambutol |
153 |
|
Isoniazid + Rifampicin |
||
|
Rifampicin + Isoniazid + Ethambutol |
||
|
(AKT4) Rifampicin + Isoniazid + Pyrazinamide + Ethambutol |
||
|
Category II |
Rifampicin + Isoniazid + Pyrazinamide + Ethambutol + Streptomycin |
Table 16: Antibiotics used for Pulmonary Tuberculosis
Discussion:
Antibiotics continue to be widely prescribed for patients presenting with LRTI. Recommendations have been published advising against their use on the basis of increasing antimicrobial resistance in respiratory pathogens and lack of proven efficacy. A critical analysis of the published evidence for effectiveness of antibiotics reveals however a surprising paucity of data. For such a common, important and controversial area the studies informing evidence-based decision making are few, disparate and underpowered.Trends favoring improved outcomes were seen for these measures of efficacy, but statistical significance was not reached. A non-significant trends towards side effects was seen in the treatment group. The antibiotics were unlikely to alter the course of illness in most adult patients.In this study titled “A Study On Therapeutic Evaluation of Various Antibiotics in Lower Respiratory Tract Infections in Adult patients”. A total of 335 patients charts were reviewed, Out of 335 cases Males were 220 members (65.67%) and Females were 115 members (34.32%) as shown in fig 7.Higher percentage of the cases belonged to the age group of 41-65 are 54.62%, as it is known that risk of LRTIs is significantly higher in this age group. Followed by age group 19-40 are 31.94% and
The results revealed that Therapeutic evaluation of various antibiotics from our case studies we could observe that the most frequently prescribed antibiotics are higher percentage of patients using Cephalosporin’s (51.14%) followed by Macrolides (17.09%), Metronidazole (12.58%), Penicillin’s (7.66%), Aminoglycosides (3.41%), Doxycycline (3.41%), Fluoroquinolones (3.27%), Carbapenems (1.30%) as shown in fig 16. In our study 335 patients among them 153 patients are diagnosed with Pulmonary Tuberculosis. So they are using ATT Category-I and Category-II drugs respectively as shown in table 16.
Acknowledgment: Authors acknowledge sincere thanks to the management and Staff of Vinayaka Missions college of Pharmacy, VMU, Salem for the facilities granted, support for the successful completion of research work.