
Mohammed H. Alsabawi1*, Ammar M. Atallah2, Saud H. Mohammed3
1C. A. B. P., Ibn sena hospital, Department of Pediatrics, Mosul, Iraq.
2D. C. H., Ibn sena hospital, Department of Pediatrics, Mosul, Iraq.
3F. I. C. M. S., Mosul General hospital, Department of Pediatrics, Mosul, Iraq.
*Corresponding Author: Mohammed H. Alsabawi, C. A. B. P., Ibn sena hospital, Department of Pediatrics, Mosul, Iraq.
Received: July 05, 2022
Accepted: July 28, 2022
Published: August 25, 2022
Citation: Mohammed H. Alsabawi, Ammar M. Atallah, Saud H. Mohammed (2022). “Bottle-feeding Mismanagement and its Management”, J Pediatrics and Child Health Issues, 3(5); DOI: http;//doi.org/03.2022/1.1050.
Copyright: © 2022 Mohammed H. Alsabawi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Introduction: Bottle-feeding is an important substitute of the breast feeding and many infants can grow well with formula feeding if done properly. In this research we discuss the skills of bottle-feeding and the mistakes that is done by many mothers (or care-givers) which have led to substantial number of specific organic diseases or other disorders that misinterpreted as an organic illnesses which led to many unnecessary investigations and treatment.
Methods: This research is done by a survey through a questionnaire of 1000 mothers (and care-givers) over about 1 year duration. The interview involves interrogation about the skills of bottle feeding and also giving advises to the mother about proper management for the mistakes when they present.
Results: It reveal a great majority of them have some sort of mismanagement during bottle-feeding.
Conclusion: Bottle-feeding mismanagement is a common problem that should be actively resolved by the pediatrician because it may cause serious harms to the baby.
Introduction
Bottle-feeding is an important substitute of the breast feeding and many infants can grow well with formula feeding if performed properly. Infant formula is indicated for infants whose intake of breast milk is contraindicated for infant factors (e.g. inborn errors of metabolism) or maternal factors. In addition, infant formula is used as a supplement to support inadequate weight gain in breastfed infants (1).
In this research we will not discuss the difference between the breast milk versus the formula milk, but rather we will discuss the skills of Bottle-feeding and the mistakes that is performed by the mother (or care-giver) which have led to substantial number of specific organic diseases; on the other hand, some of these disorders are misinterpreted as an organic disorders which led to many unnecessary investigations and treatment.
There are many articles that discuss this issue; but this research will discuss it in a specific manner and try to fulfill all the aspects of this issue along with advices about solutions of these mismanagements.
Method
This research is performed by a survey through a questionnaire of 1000 mother (or care-giver) over about 1 year duration (between 2021-2022). The survey is performed by direct interview with the mother in the hospitals, clinics, and community in Mosul city and by electronic survey in the internet. The interview involve also advises given to the mother about proper management for the mistakes when they present. The questionnaire involves the following 8 questions:-
Results
The results of the above questionnaire are as follow:-
Note: This question is only applicable for those with exclusive bottle-feeding.
The data above may be less than the real data because some mothers may cheat in their answers during interrogation due to the fear from criticism.
Discussion
After interrogation of the mothers (or care-givers) by the questionnaire during survey, it reveals that the great majority of them have some sort of mismanagement during bottle feeding.
These mismanagements are more common among uneducated, low IQ,, and young age mothers, mothers from rural areas, mother with first baby, and lack of experienced older woman in the family e.g. grandmother.
Now we will discuss each item of the above questionnaire separately:-
Note: Some formula manufacturers (e.g. Similac Neosure®) use double size scoop which necessitate double amount of water for mixing.
The concentrated milk will cause hypernatremic dehydration, colic, irritability, and constipation.
Some mothers put water more than the recommended amount either not intentionally or sometimes intentionally to save the amount of milk powder as much as possible due to economic issue e.g. poverty. This diluted milk may cause increase bowel motion (which is misdiagnosed as diarrhea), water intoxication, electrolyte disturbances (especially hyponatremia), and convulsion (2,4).
Note: If the inner barrier of the can of formula is inflated, this may be a clue that the milk is contaminated with gas forming microorganism, especially when the product is improperly stored in hot environment.
On contrary, some mothers feeds her baby too little amount of milk or less frequent feeds below the recommended amount and frequency of feeding. This will leads to poor weight gain and even failure to thrive (FTT) of the baby. See the table below for the recommended amount and frequency of feeding.
Recommendations
Breast feeding is the best for the infants because it is sterile, do not need preparation, and its contents are ideal for infants; however if the mother prefer to feed her baby with bottle-feeding, its management can be performed simply by the following solutions:-
When the mother decide to feed her baby with bottle, it is the job of pediatrician is to learn her about the skills of bottle-feeding (by the above recommendations), which should be emphasized at each visit to the pediatric clinic. In addition to that, communication media e.g. TV and social media can actively participate in this issue.
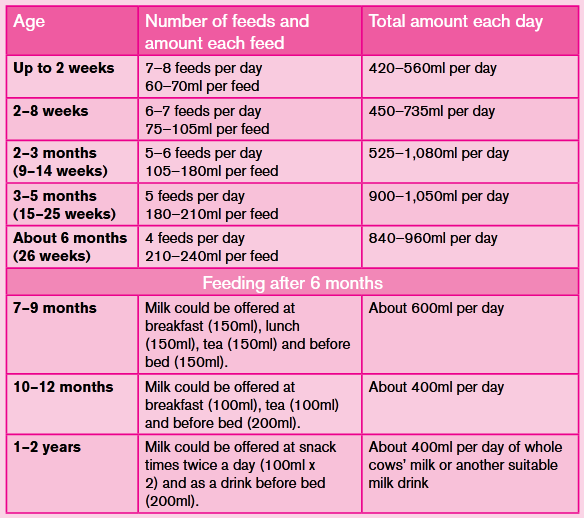
Table-1: shows the recommended amount and frequency of feeding according to age (with permission)
Conclusion
Bottle-feeding mismanagement is a common problem that should be actively resolved by the pediatrician because it may cause serious harms to the baby. However it can simply be managed by the above advices to the mother.
Authors' contributions:-
Mohammed H. Alsabawi contributed to data collection and study design.
Ammar M. Atallah contributed to data collection and the introduction.
Saud H. Mohammed contributed to data collection and the discussion.
Statement of Ethics: This study was performed in line with the principles of the Declaration of Helsinki. This study protocol was reviewed and approved by the committee of Nineveh health directorate no. 112 at 16th of march-2022.
Conflict of Interest Statement: The authors have no conflicts of interest to declare.
Funding sources: The authors have no relevant financial or non-financial interests to disclose.