
Alwaleed Al-Dairy1*, Mohannad Saleh2, Najwa Alhalaky 3, Jinait Mnairjy3
1Assistant Professor in Cardiac Surgery at Faculty of Medicine, Damascus University.
2 Cardiac surgeon at Faculty of Medicine, Damascus University.
3Medical student at Faculty of Medicine, Damascus University.
*Correspondence to: Alwaleed Al-Dairy, Assistant Professor in Cardiac Surgery at College of Medicine, Damascus University, and Cardiac Surgeon at Damascus University Cardiac Surgery Hospital. Damascus, Syria.
Received Date: November 20, 2023
Accepted Date: December 01, 2023
Published Date: December 12, 2023
Citation: Alwaleed A Dairy, Saleh M, Alhalaky N, Mnairjy J, (2023). “Aortic reimplantation of an anomalous left coronary artery arising from the pulmonary artery: A case report”. Pediatrics and Child Health Issues, 4(1); DOI: http;//doi.org/11.2023/1.1057.
Copyright: © (2023) Alwaleed Al-Dairy, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA), is a rare life-threatening congenital heart defect. Patients usually present in infancy with cardiomyopathy and congestive heart failure; however, they may survive to childhood or adulthood. Aggressive surgical repair is indicated regardless of age or symptoms. Aortic reimplantation to provide dual supply coronary system is the preferred surgical approach.
Case presentation: Herein, we report a case of a 5-year-old girl who present with exertional dyspnea and moderate left ventricular dysfunction. Surgical repair of ALCAPA by aortic reimplantation was performed successfully with significant improvement in left ventricular function postoperatively.
Conclusion: ALCAPA is a rare and life-threatening CHD that demands aggressive surgical repair. Aortic reimplantation to provide dual supply coronary system is the preferred surgical approach.
coronary artery; coronary anomalies; reimplantation of coronary artery: case report
Introduction:
Anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA), also known as Bland-White-Garland syndrome, is a rare congenital heart defect (CHD) with a prevalence of 1 in 300,000 live births (1). If left untreated, 90% of infants die within the first year of life (2). As the pulmonary vascular resistance and pulmonary arterial pressure decrease, there would be a retrograde flow in the left coronary artery towards pulmonary artery (coronary steal phenomenon) which leads to ischemia-induced left ventricular (LV) dysfunction and secondary mitral regurgitation (MR) (3). According to the degree of the development of collateral circulation between the right and the left coronary arteries, ALCAPA can be classified into two types. The first one is the infant type (with insufficient collateral circulation) in which infants present with cardiomyopathy and symptoms of congestive heart failure (CHF) early in life. The second is the adult type (with sufficient collateral circulation) in which children, or adults, may be asymptomatic, or they may suffer from exertional dyspnea, palpitation, and sudden death (4, 5). Early diagnosis and prompt surgical repair can result in gradual myocardial recovery. In this article, we report a case of a 5-year-old girl who underwent successful surgical repair of ALCAPA.
Case presentation:
A 5-year-old girl was presented to our hospital with complain of exertional dyspnea for three months. In her past medical history, the parents mentioned that she had been suffering from recurrent pulmonary infections and palpitation, and recently they noticed limitation in her physical activity. Physical examination was normal. Chest x-ray showed cardiomegaly for which transthoracic echocardiography (TTE) was requested. TTE revealed moderate left ventricular (LV) dysfunction with estimated ejection fraction (EF) of 40%, mild MR, and suspected the diagnosis of ALCAPA which was confirmed by diagnostic coronary angiography. Electrocardiography (ECG) showed T-wave inversion in leads V1-V4. The patient was scheduled for elective surgical repair. The operation was performed through median sternotomy with complete cardiopulmonary bypass (CPB). The left coronary artery (LCA) was seen on the lateral side of the main pulmonary artery (PA). The right and left pulmonary arteries were dissected and controlled. The aortic cross clamp was applied, and the heart was arrested by antegrade cold blood cardioplegic solution via both the ascending aorta and the main pulmonary artery after closing its branches. PA was transected above the sinotubular junction, and the orifice of the anomalous LCA was seen on the left posterior sinus of Valsalva (Figure 1). It was harvested as a coronary button and dissected to gain as much length as possible to reach the aorta for tension-free implantation. The LCA was reimplanted on an orifice made in the lateral side of the aorta, and the defect in PA was repaired by fresh autologous pericardium (Figure 2), and end-to-end anastomosis was performed. The aortic cross clamp was released, and the patient was weaned off the bypass uneventfully. She was extubated after 4 hours in the intensive care unit where she stayed for only 24 hours. Postoperative TTE showed improved normal LV function with EF of about 50%, and mild MR. The patient was discharged from the hospital on the fifth postoperative day. After a follow-up period of 6 months, the patient was asymptomatic with normal physical activity, and normal LV function with EF of 60%.
Discussion:
ALCAPA is a rare anomaly that represent only 0.25 to 0.5% of all congenital heart defects (6). It is potentially life threatening congenital coronary artery malformation with only 15-20% of patients survive their first year of life (1-4). Whenever the diagnosis is established, surgical correction of ALCAPA is indicated regardless of age, symptoms, or the degree of collateral circulation (7). Different surgical approaches have been described (simple ligation of the anomalous LCA with or without coronary artery bypass grafting, Takeuchi operation); however, aortic reimplantation of the anomalous LCA to ensure dual supply coronary system remains the gold standard treatment of ALCAPA (3, 7, 8). Significant improvement in both LV function and preoperative MR has been reported after successful repair of ALCAPA (5-8), and this was the case of our patient in whom EF of LV improved from 40% to 60% postoperatively. Follow-up will be necessary to ensure recovery of the LV function and the mitral valve.
Conclusion:
ALCAPA is a rare and life-threatening CHD that demands aggressive surgical repair to halt progression of myocardial ischemia, and to prevent fatal ventricular arrhythmias and sudden death. Aortic reimplantation to provide dual supply coronary system is the preferred surgical approach.
Figure legends:
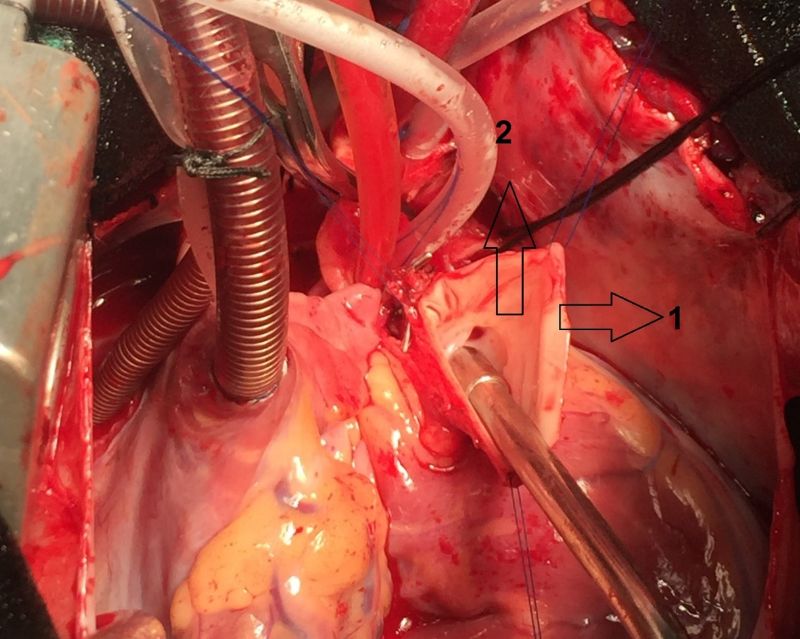
Figure 1: intraoperative image showing the orifice of the anomalous left coronary artery from the inside of the transected pulmonary artery. 1: the transected pulmonary artery, 2: the orifice of the anomalous left coronary artery. 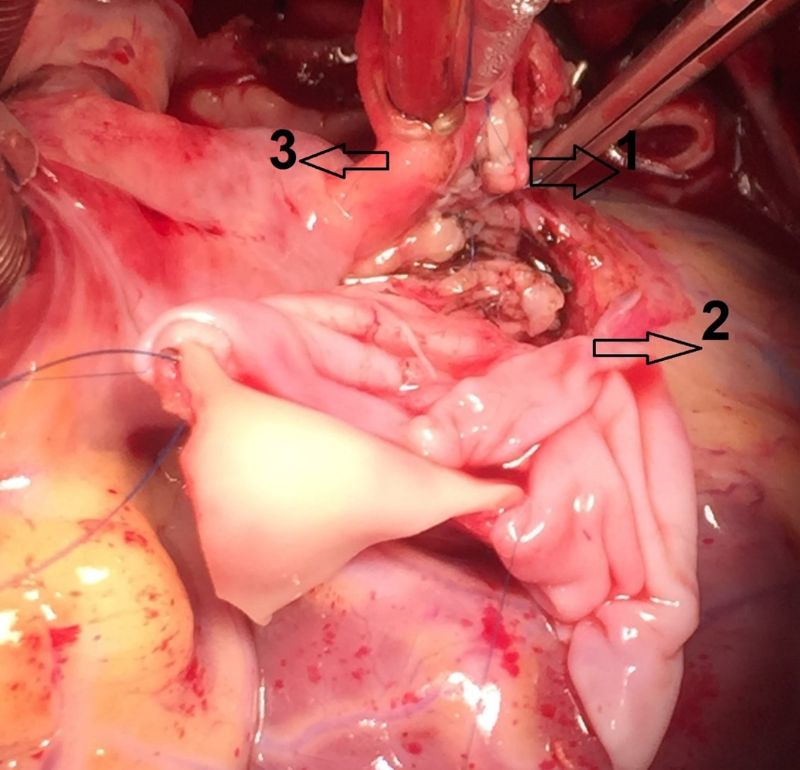
Figure 2: intraoperative image showing the implanted coronary button on the aorta. 1: the implanted coronary button, 2: the fresh autologous pericardial patch used to repair the defect in the pulmonary artery, 3: the ascending aorta.
Ethical Approval and Consent to participate: The manuscript was approved by ethics committee at Damascus University.
- Consent for publication: Written informed consent was obtained from the patient's legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
- Availability of supporting data: The data that support the findings of this study are available from the corresponding author, [A.A], upon reasonable request.
- Competing interests: The authors have no conflict of interest
- Funding: There is no funding resources for writing this manuscript.
- Authors' contribution
Alwaleed Al-Dairy: Planned and performed the work leading to the report. Wrote and reviewed successive versions and participated in their revisions.
Mohannad Saleh: Participated in writing the report and approved the final version.
Najwa Alhalaky: wrote and reviewed the successive versions and participated in their revisions.
Jinait Mnairjy: wrote and reviewed the successive versions and participated in their revisions.
- Acknowledgements: Not Applicable.
Author’s Declaration:
None of the authors listed on the manuscript are employed by a government agency that has a primary function other than research and/or education. Moreover, none of the authors are submitting this manuscript as an official representative or on behalf of the government.