Pediatrics and Child Health Issues
OPEN ACCESS | Volume 5 - Issue 2 - 2025
ISSN No: 2836-2802 | Journal DOI: 10.61148/2836-2802/JPCHI
Dimple Padawe1, Kshitija K Bansode2, Vilas Takate3, Kishor Dighe4, Gauri Vijaykumar Rathi5
1 Prof & HOD Dept Pediatric & Preventive Dentistry, Govt Dental College & Hospital, Mumbai, India.
2Post Graduate student Dept Pediatric & Preventive Dentistry,Govt Dental College & Hospital, Mumbai, India.
3Associate Professor Dept Pediatric & Preventive Dentistry, Govt Dental College & Hospital, Mumbai, India.
4Assistant Professor Dept Pediatric & Preventive Dentistry,Govt Dental College & Hospital, Mumbai, India.
5Post Graduate student Dept Pediatric & Preventive dentistry Government Dental College & Hospital, Mumbai, India.
*Corresponding Author: Kshitija K Bansode, Post Graduate student Dept Pediatric & Preventive Dentistry,Govt Dental College & Hospital, Mumbai, India.
Received: July 14, 2021
Accepted: July 23, 2021
Published: July 26, 2021
Citation: Dimple Padawe, Kshitija K Bansode, Vilas Takate, Kishor Dighe, Gauri Vijaykumar Rathi. “Prosthetic Rehabilitation with Complete Denture of a 6- year old Child with Hypohidrotic Ectodermal Dysplasia and Anodontia: a case report.”, J Pediatrics and Child Health Issues, 2(5); DOI: http;//doi.org/03.2021/1.1032.
Copyright: © 2021 Kshitija K Bansode. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Background: Ectodermal dysplasia (ED) represents a disease which is caused by abnormal growth of ectodermal derivatives. Prosthetic interventions are very important in the management of ED patients, as they solve problems related to functional, aesthetic, and psychological issues, and improve the quality of patient health.
Case report - A 6-year-old boy with ED along with complete anodontia was treated by fabrication of conventional maxillary and mandibular complete dentures.
Conclusion - The use of the removable prosthesis in children suffering from ectodermal dysplasia is one of the treatment modalities that helps to restore occlusion, masticatory function, aesthetics, and overall oral functions.
1. Introduction
Ectodermal dysplasia (ED) is a syndrome involving a diverse category of hereditary defects characterized by abnormalities in the growth of tissues derived from the embryonic ectoderm [1]. This disorder is rather uncommon (7 occurrences per 10,000 live births), mostly affecting males and its 150 subgroups are categorized either as Christ-Siemens-Touraine syndrome (hypohidrotic) or Clouston's syndrome (hidrotic) depending on the involvement of sweat glands [2,3]. Hypohidrotic ED is characterized by either absent or significant reduction in the number of sweat glands whereas hydrotic ED is associated with normal sweat glands. This syndrome can be transmitted as a sex-linked trait, an autosomal recessive trait, or an autosomal dominant trait [3]. Though Thurnam in 1848 was the first to report a patient with ED, it was not until 1929 that Weech AA coined the term ED [4].
Mutations in the ectodysplasin (EDA) gene induces X-linked recessive hypohidrotic ED, which produces the soluble protein, that triggers the JNK/c-fos/c-jun and NF-kappaB signaling pathways [5]. The transformations in the DL gene, that encodes the EDA-receptor, is reported to cause autosomal dominant and recessive hypohidrotic ED. [6]. The mutations in the EDARADD (ectodysplasin receptor associated death domain) gene, produces a protein that reacts with the receptor, leading to autosomal recessive hypohidrotic ED [7]. In a patient with hypohidrotic ED, a heterozygous mutation in the TRAF6 gene has been identified [8].
Extraoral features include protuberant lips, depressed nasal bridge, hypotrichosis, and frontal bossing. Intraoral manifestations include hypodontia or anodontia of the deciduous and/or permanent dentition, hypoplastic crown and underdeveloped alveolar crests with reduced vertical dimension. Several factors such as age of the patient, stage of growth & development, presence of malformed dentition, soft tissue defects, and psychological state needs to be considered in the treatment planning [9].
Early oral and prosthetic rehabilitation is necessary for ED patients not only to reestablish aesthetic appeal and masticatory function, but also to take care of psychological problems and enhance self-esteem. To ensure accurate diagnosis and provide the best care for patients and their relatives, a multidisciplinary approach is required. Prosthetic rehabilitation for such patients must be preferred to one to one basis, taking each patient's clinical features into account. Single unit crowns, removable partial prothesis, complete dentures, overdentures, fixed partial prothesis, and implant supported dentures have all been considered as treatment options. Children with ED are frequently treated with a removable denture until a more definitive prosthesis is delivered [10,11].
Hence, we are reporting a case of hypohidrotic ED with anodontia in a 6-year old child treated with conventional removable complete dentures.
2.Case Report
2.1 History and diagnosis
A 6-year old boy reported to department of Pediatric & Preventive Dentistry, Government Dental College and Hospital, Mumbai, with a chief complaint of inability to eat food and unaesthetic appearance. The patient’s parents gave a history of lack of perspiration, high body temperature and dry skin. These findings were also seen in his maternal uncle. Extraoral examination revealed sparse thin hair, thin eyebrows, saddle nose, dry, thick & everted lips, brittle nails, lower facial height and concave facile profile (Fig I). Dry oral mucosa, absence of saliva and absence of all maxillary and mandibular primary teeth were reported through intraoral examination. (Fig II) Panoramic radiograph revealed the absence of permanent maxillary and mandibular teeth (Fig III). Family history and clinical features confirmed the diagnosis of hypohidrotic ED. After reviewing Fisherman's [12] skeletal maturation indicators, it was discovered that the skeletal growth was not complete and hence no definitive prosthesis could be advised for another 10-11 years.
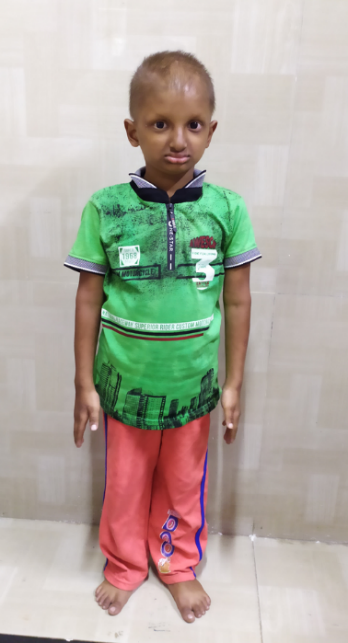
Figure I – Extraoral features: thin, sparse scalp hair, everted and thick lips, brittle nails, thin
eyebrows, saddle nose and concave facial profile.

Figure II – Complete edentulous maxillary and mandibular arch.

Figure III- Panoramic radiograph showing absence of teeth in maxillary and mandibular arch
2.2 Treatment
Removable complete dentures were designed to deliver quick aesthetic results, restore occlusion, and allow the patient to get accustomed with the removable prothesis before the definitive prosthesis was delivered [13]. Irreversible hydrocolloid impression material was used for primary impressions because it is comfortable and easy to remove from undercut areas. Type III dental stone was used to make the casts. After final impression with Zinc oxide eugenol impression paste, custom trays were fabricated and border moulding was performed with green stick compound. The master casts were mounted on a semi-adjustable articulator, and the maxillo-mandibular relation was recorded. A balanced occlusal scheme was used to arrange the teeth [14]. The maxillary and mandibular prostheses were fabricated in heat cure acrylic resin after a try-in and careful evaluation. After that, the prothesis were placed in the patient's mouth. (Fig IV)

Figure IV – Patient with removable maxillary and mandibular complete dentures.
2.3 Follow-up
The patient and his parents were taught how to properly insert and remove the prostheses, as well as how to maintain proper denture hygiene. After 24-hours, a recall was scheduled to make the necessary modifications. Follow-up visits were planned every 6 months to review the bone growth and to reline the dentures.
3.0 Discussion
Treating the pediatric patients with ED is a difficult task. As Nowak stated, ‘treating the pediatric patient with ED requires the clinicians to be knowledgeable in growth and development, behavior management, techniques in the fabrication of prothesis, the modification of existing teeth utilizing various restorative techniques, the ability to motivate the patients and parents for the use of prosthesis, and the long term follow-up, for the modification and/or replacement of the prosthesis [15].
Prosthodontic intervention at a young age assists the child in adjusting to the prosthesis and developing aesthetics, speech, chewing, and maintaining a proper temporomandibular joint function. During the growth spurts, the intraoral dentures can be easily altered. Aside from dental advantages, early intervention has psychological advantages too [16]. Removable complete dentures are a reversible treatment option for young patients that can suggestively enhance masticatory functions and aesthetics. Furthermore, it aids in the reduction of complications caused by tooth loss, such as resorbed alveolar ridges, reduced vertical height, and a predisposition for class III malocclusion. It also aids in boosting the patient's self-confidence and prevents psychological disturbance caused by tooth loss [17].
The primary treatment option for tooth replacement and masticatory function rehabilitation is implant-supported or retained dentures. Case reports have confirmed the efficacy of this treatment option in those with ED as well as healthy young individuals. However, implant therapy may fail due to a insufficient alveolar bone, implant’s dislocation or relocation due to jaw growth, leading to tooth germ trauma, ankylosis of teeth, and multifaceted craniofacial growth limitations [18]. Hence we preferred fabricating a removable complete denture in our present case.
A healthy temporomandibular joint and consistent mandibular movements are also aided by good occlusal support. It's important to remember that anodontia and masticatory incapacity are major causes of malnourishment and that the development of lifelong dietary patterns, ensues during childhood [19].
Following up with ED patients after they've received removable prostheses is crucial to ensuring a positive treatment outcome and avoiding complications. Existing teeth with anatomic and morphological abnormalities, as well as atrophic alveolar crests, may lead to poor prosthesis stability and retention. Another issue is gradual resorption of the alveolar bone, which occurs because of the edentulous ridge being, present at a young age. It is mandatory to educate the patient and their parents about potential problems and how to maintain any prosthesis. Periodic recalls are also necessary because continued growth and development will necessitate prothesis modification or replacement. In addition to fit adjustments, prosthesis occlusion must be monitored for ages due to jaw growth [20].
4.0 Conclusion
A multidisciplinary approach should apply to young patients with ED and be tailored to meet the needs of each patient. An early replacement of missing teeth, plays a huge role in restoring the chewing function, aesthetics and speech for the patient, thus improving the self-esteem, and the overall quality of life for the patient.