Pediatrics and Child Health Issues
OPEN ACCESS | Volume 5 - Issue 2 - 2025
ISSN No: 2836-2802 | Journal DOI: 10.61148/2836-2802/JPCHI
Aamir Jalal Al-Mosawi
Advisor doctor in pediatrics and pediatric psychiatry, Baghdad Medical City and Iraqi Ministry of Health, Baghdad, Iraq
*Corresponding author: Aamir Jalal Al-Mosawi, Advisor doctor in pediatrics and pediatric psychiatry, Baghdad Medical City and Iraqi Ministry of Health, Baghdad, Iraq
Received: May 22, 2021
Accepted: June 14, 2021
Published: June 16, 2021
Citation: Aamir Jalal Al-Mosawi, “Cerebral Palsy, Autistic Features Associated with Periventricular White Matter Hyperintensity On Brain Magnetic Resonance Imaging: A Diagnostic Challenge”, J Pediatrics and Child Health Issues, 2(5); DOI: http;//doi.org/03.2021/1.1021.
Copyright: © 2021 Aamir Jalal Al-Mosawi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Background: Periventricular leukomalacia is the most common abnormalities seen in children with cerebral palsy especially of the spastic type. The reported brain imaging abnormalities in patients with autism disorders include arachnoid cyst, agenesis of the corpus callosum, evidence of vasculitis (In Heller syndrome), and brain imaging abnormalities related to a coexisting condition such as cerebral palsy. The association of periventricular white matter hyperintensity on brain magnetic resonance imaging with cerebral palsy and autistic features has not been reported before.
Patients and methods: A Palestinian doctor from the Western Bank consulted us about her 4-year old boy who had a diagnosis of cerebral palsy (mild spastic diplegia) and gross sensory motor delay with development of some autistic features. The rare occurrence of spastic cerebral palsy and autistic features with periventricular white matter hyperintensity on brain magnetic resonance imaging is described in this paper.
Results: The patient was born prematurely at 32 weeks gestation through emergency cesarean. His Apgar score at birth was 9 at 0 second, but he was intubated 9 hours after delivery due to acute respiratory distress syndrome and remained intensive care unit for 19 days. At the age of 18 months, he started to regress and become mute and started to show autistic features. Brain MRI showed bilateral leukodystrophy-like picture with bilateral periventricular zones of increased signal intensity. At the age of four years, he evidences of spastic cerebral palsy, and could walk without support for only few steps. He was not saying any word and was considered to have autistic features with impaired communication and delayed speech development.
Conclusion: This paper reports the very rate sporadic occurrence of periventricular white matter hyperintensity on brain magnetic resonance imaging with atypical neuropsychiatric manifestation including late onset (after the first year) non-progressive spastic cerebral palsy, and autistic features.
Introduction
Magnetic resonance imaging has become an important tool for the diagnosis of pediatric periventricular white matter brain disorders that may not be apparent on CT scans. Leukodystrophy is regarded as the typical example of progressive cerebral periventricular white matter brain disorders.
Magnetic resonance findings in leukodystrophy include T2 weighted (spin-echo) images showing prominent asymmetric involvement of brain white matter, particularly in the periventricular white matter and visual radiations. Calculated T1 values are elevated in the patients with leukodystrophy. Other conditions that can be associated with periventricular hyperintensity include multiple sclerosis, which is rarely observed early in life, and also hydrocephalus [1, 2].
In 1996 Kristjánsdóttir et al from Sweden studied 78 pediatric patients with white matter abnormalities on magnetic resonance imaging, 13 patients with an apparently leukodystrophy white matter had non-progressive poorly defined non-specific disorders [3].
Patients and methods
On the 4th of January 2021, a Palestinian doctor from the Western Bank consulted us about her 4-year old boy who had a diagnosis of cerebral palsy (mild spastic diplegia) and gross sensory motor delay with development of some autistic features. The rare occurrence of spastic cerebral palsy and autistic features with periventricular white matter hyperintensity on brain magnetic resonance imaging is described in this paper.
Results
The patient was born on 7th of November 2016 prematurely at 32 weeks gestation through emergency cesarean section He was a result of in vitro fertilization pregnancy. He is the 3rd between his siblings. His Apgar score at birth was 9 at 0 second, but he was intubated 9 hours after delivery due to acute respiratory distress syndrome and remained intensive care unit for 19 days. He was hypotonic on third day of delivery, but his tone improved thereafter. When he discharged from hospital, he didn’t have obvious complications, and all his initial and repeated investigations were normal. He was feeding both breast and bottle during infancy. His growth and development were considered acceptable until the age of 18 months, when he received MMR vaccine, within 10 hours, he became very sick and developed severe flu-like symptoms and lethargy. He lost 3 kg in one week. Thereafter, he started to regress and become mute and started to show autistic features.
There was no family history of a similar condition despite that all of his siblings were born prematurely, but without developing complications or neurological abnormality. He had a 20-year old sister, 17-year old sister who was born at 27th wk. of gestation, but she was totally doing well and was great, and a younger 2-year old healthy brother.
Brain MRI was performed at the age of two years and showed bilateral periventricular zones of white matter hyperintensity on the FLAIR and T2 weighted images appearing hypointense on T1 weighted images, more prominent at the posterior aspect of the lateral periventricular regions. The subcortical white matter, the basal ganglia, thalamus, the corpus callosum, the brainstem and cerebellum all had normal appearance.
MRI also showed cavum septum pellucidum with cavum verge which is a common anatomical variant
The boy had leukodystrophy like picture with bilateral periventricular zones of increased signal intensity on T2 and FLAIR images. The MRI report emphasized that a delayed myelination is less likely.
At the age of four years, he could walk without support for few steps, but was falling on his head several times. He was not saying any word and was considered to have impaired communication with others as he was not responding to his name most of the time. He was laughing out loud out of a sudden with no apparent reason. He was sometimes looking at his hand while waving with it. He was refusing solid food and accepting some soft puree food especially yogurt with jam and was preferring sweetie foods.
He was treated with vitamin D, l-carnosine, omega 3, phosphatidylcholine syrup, hyperbaric oxygen therapy, and physiotherapy, but without obvious response.
Discussion
Periventricular leukomalacia is the most common abnormalities seen in children with cerebral palsy especially of the spastic type [4, 5, 6]. Figure-1 shows periventricular leukomalacia seen on brain MRI of a 22 months girl with cerebral palsy.
However, we have previously reported a female with cerebral palsy who had more severely affected brother with spastic cerebral palsy and imaging study showing findings similar to the findings of leukodystrophy [4].
Autistic disorders are heterogeneous complex group of chronic disorders that are associated with significant early impairment in socialization, communication, and behavior. The association of Autism disorders with significant brain imaging abnormalities has been infrequently reported. However, we have previously reported that brain imaging abnormalities in patients with autism disorders include arachnoid cyst, agenesis of the corpus callosum, evidence of vasculitis (In Heller syndrome), and brain imaging abnormalities related to a coexisting condition such as cerebral palsy [7].

Figure-1A: Periventricular leukomalacia seen on brain MRI of a 22 months girl with cerebral palsy
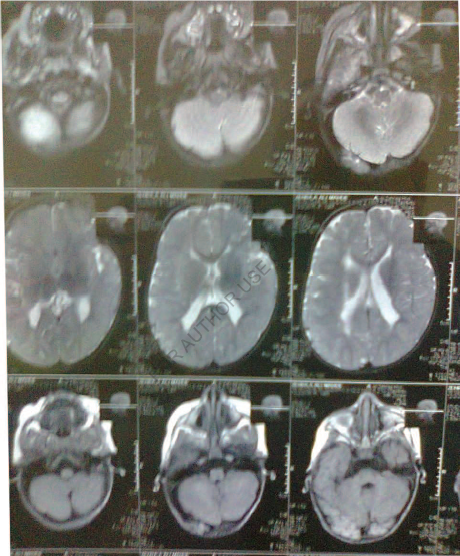
Figure-1B: Periventricular leukomalacia seen on brain MRI of a 22 months girl with cerebral palsy

Figure-1C: Periventricular leukomalacia seen on brain MRI of a 22 months girl with cerebral palsy
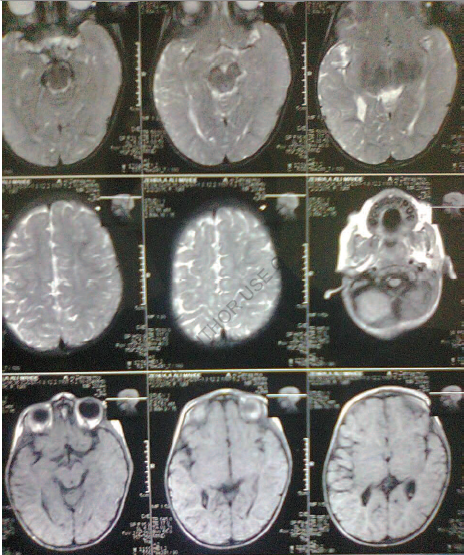
Figure-1D: Periventricular leukomalacia seen on brain MRI of a 22 months girl with cerebral palsy
In 2000, Kristjánsdóttir, Vibrant, and Wieland from Sweden described fifteen pediatric patients who had non-specific clinical neurological had leukodystrophy-like white matter abnormalities on brain MRI and had non-progressive clinical manifestations and course.
The patients of Kristjánsdóttir and colleagues had early onset of symptoms within the first year of life, most often presenting as general developmental delay and hypotonia. Later appearing signs were spasticity and ataxia and as a rule severe learning and motor disabilities. Serious ocular abnormalities were frequent [8].
The sporadic occurrence of periventricular white matter hyperintensity on brain magnetic resonance imaging in association with mental retardation, retinitis pigmentosa, and optic atrophy was reported in one boy only before [1,2].
Conclusion
This paper reports the very rate sporadic occurrence of periventricular white matter hyperintensity on brain magnetic resonance imaging with atypical neuropsychiatric manifestation including late onset (after the first year) non-progressive spastic cerebral palsy, and autistic features.