Francisco Novoa MS, Jayer Chung MD, Rachel Silverstein MD*, MBS, Aharon Z. Gladstein, MD
Texas Children's Hospital 6701 Fannin Street, Houston Texas 77030.
*Corresponding Author: Rachel Silverstein, Texas Children's Hospital 6701 Fannin Street, Houston Texas 77030.
Received date: October 27, 2021
Accepted date: November 05, 2021
Published date: March 10, 2022
Citation: Francisco Novoa MS, Jayer Chung, Rachel Silverstein, Aharon Z. Gladstein. “Delayed Diagnosis of Traumatic AV Fistula in the Setting of Closed Treatment of a Tibia Fracture’’. J Orthopaedic Research and Surgery, 2(4); DOI: http;//doi.org/03.2021/1.1022.
Copyright: © 2022 Rachel Silverstein. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Traumatic arteriovenous fistula is a rare delayed vascular complication of closed long bone fractures in the pediatric population. We present a case of a 14-year-old boy who developed a fistula between the posterior tibial artery and vein. This was diagnosed 1 year after cast treatment for a closed fracture of the mid shaft tibia. The fracture was treated by closed reduction and casting. After the diagnosis was made clinically and confirmed on sonography, the fistula was treated successfully with surgical ligation. Subsequent Doppler sonography confirmed the absence of recurrence of the fistulous tract and radiographs showed satisfactory healing of his fractures. The patient had resumed his usual activities without difficulty.
Introduction:
Arterio-venous fistula (AVF) is a rare injury among children. It is often associated with penetrating injuries or iatrogenic trauma. In contrast to acute ischemia, some vascular injuries associated with long bone fractures may not present acutely and it may take months to years for them to present [1]. Post-traumatic AVF, pseudoaneurysm and vascular thrombosis are the major delayed injuries associated with long bone fractures [2, 3]. AVF associated with closed fractures can be hard to detect, and may not yet be present, early in the course of treatment. Symptoms may be occult and can be limited to pain and edema, which may be attributed to the fracture itself [4]. High flow lower extremity AVF that are not appropriately treated may lead to venous hypertension. This is marked by limb edema, stasis dermatitis, and venous ulceration [1, 5, 6]. The treatment of an AVF of the extremity can involve image guided procedures such as embolization, or may involve operative intervention to ligate the fistula [7-9].
In this case report we present a case of AVF between the posterior tibial artery and vein which presented one year following closed treatment of a midshaft tibia fracture in a 14 year old boy.
Case report:
A 14-year-old boy with no past medical history presented to the emergency department with right leg pain after falling from his dirt bike. Examination showed abrasions over anteromedial aspect of his right leg. All compartments were firm but compressible. No pain with passive toe extension was noted. Dorsalis pedis and posterior tibial pulses were normal. Plain radiographs showed closed displaced fractures of the mid shaft tibia and fibula (Fig. 1). The leg was splinted temporarily to avoid any additional soft tissue injury. The patient was indicated for closed reduction and casting under general anesthesia in order to preserve alignment and allow for appropriate healing.


Figure 1: AP and lateral tib fib x rays at time of injury
In the operative Room (OR), A closed reduction was performed under general anesthesia. Fluoroscopy showed acceptable alignment with no angulation, minimal shortening, and 1/2 shaft width lateral displacement. (Fig. 2)


Figure 2: AP and lateral x rays at time of closed reduction
A long leg cast was placed with a varus mold at the fracture site. The cast was bivalved. The patient tolerated the procedure well with no complications. The patient was discharged, and a follow-up was scheduled after a week. Serial follow ups occurred at 1 week and 2 weeks showed unchanged alignment. At 6 weeks the long leg cast was removed, and short leg cast was applied. At 8 weeks, the radiographs showed fracture healing in good alignment (Fig. 3).


Figure 3: Healing fracture at 8 weeks post injury
Short leg cast was discontinued, and CAM boot was placed. Radiographs obtained at 16 weeks visit showed healing with excellent alignment. He was discharged from follow up at that time.
One year after the initial injury, he presented to the clinic complaining of a palpable vibration in his right distal tibia. Examination showed thrill at right posteromedial aspect of the tibia. Duplex ultrasound (US) was ordered and vascular surgery department was consulted. The Duplex US report demonstrated a right posterior tibial artery pseudoaneurysm with AV fistula. Computed tomography angiography (CTA) imaging was ordered for better planning of care. The CTA showed a 5 mm pseudoaneurysm arising from the dorsolateral aspect of the posterior tibial artery 13 cm distal to its origin. (Fig.4).

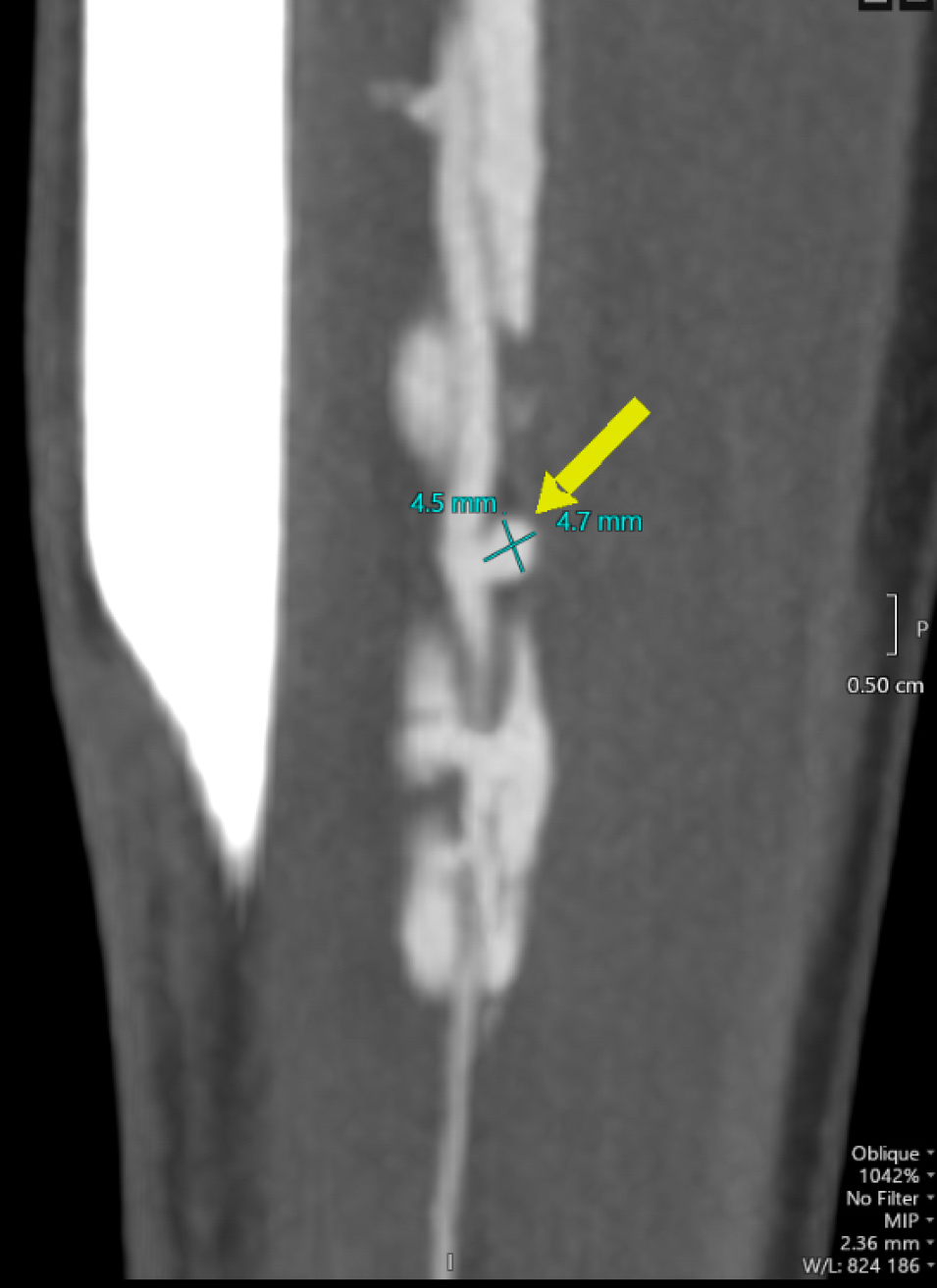
Figure 4: Selected CT angiographic cuts showing the AV fistula and pseudoaneurysm
There was a post-traumatic AV fistula at the same level from the medial aspect of the posterior tibial artery to the posterior tibial vein. Both the pseudoaneurysm and the AV fistula were just below the level of the tibial/fibular diaphyseal fractures. Surgical ligation was planned.
In the OR ultrasound was used to localize the area of the posterior tibial artery AVF. Longitudinal incision was made along the length of the distal half of the calf one fingerbreadth below the tibia. The gastrocnemius and soleus muscles were then mobilized of the tibia and the flexor digitorum longus and brevis were separated to find the posterior tibial artery and vein. The artery and vein were carefully dissected of one another, ligating all branches in-between until the fistula was identified. Confirmation of the fistula was carried out by clamping it and noting the disappearance of the thrill in the posterior tibial vein. The fistula was clamped, and a Cameron closure of the fistula with a running mattress suture was placed. This was supplemented by several other interrupted mattress sutures. (Fig.5)
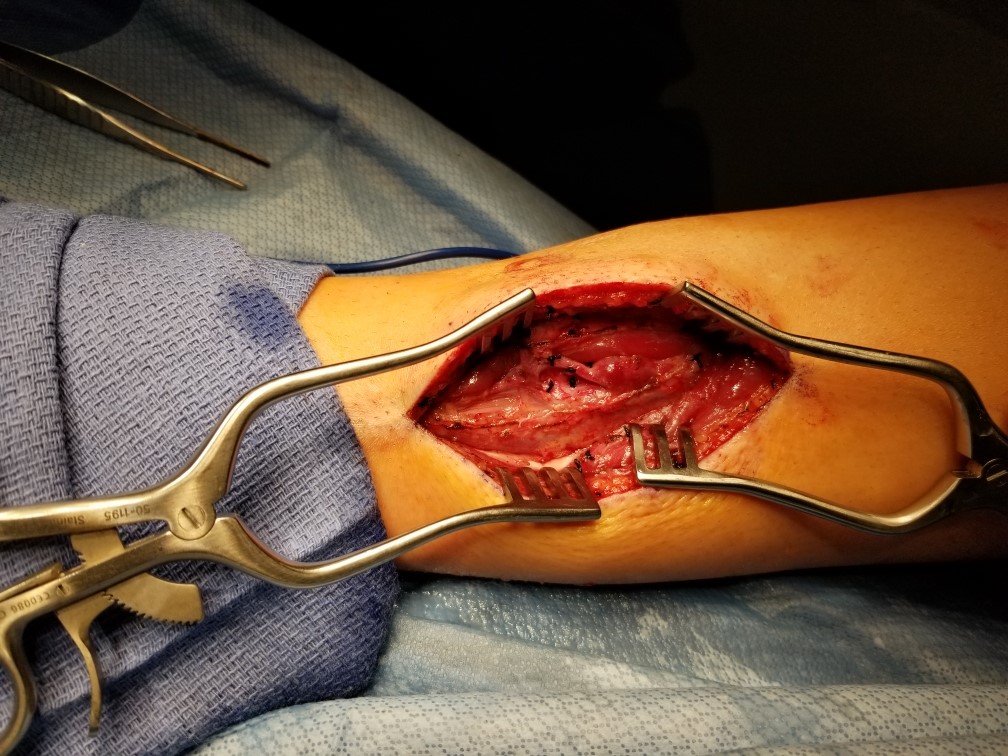
Fig.5 Showing final picture of after fistula ligation and good hemostasis.
Before closure, a doppler signal in the posterior tibial artery, disappearance of the thrill (palpable or by doppler) in the posterior tibial vein were confirmed. Incision was closed in layers.
On examination four weeks later, the incision was well-healed with no pain or tenderness. Doppler sonography confirmed the absence of recurrence of the fistulous tract and radiographs showed satisfactory healing of his fractures. The patient had resumed his usual activities without difficulty.
Discussion:
Post-traumatic AVF is a rare delayed complication of long bone fractures in the pediatric population [4]. They could result from blunt orthopaedic injuries that produces compression and injury to the vessels between the force of impact and the bone. The damaged vessels may develop a communication as they heal, resulting in AVF [10]. Diagnosis of an AVF is often delayed because the main attention is usually directed towards the primary injuries. Unfortunately, symptoms can either be partially or completely absent. Since swelling is common during trauma, it is not usually attributed to an AV fistula [11].
In the literature, few case reports could be found discussing this type of injuries. Bowers et al. [4] have reported 3 cases of traumatic lower extremity arteriovenous fistulae in children. One case was an 11-year child who developed AVF following distal tibia and fibula fracture treated with a single Kirschner wire and fasciotomies of the anterior and lateral compartments performed through a single anterolateral skin incision. The other two cases developed AVF following an in-situ pinning of a stable slipped capital femoral epiphysis, and four compartment fasciotomies for chronic exertional compartment syndrome respectively. All the 3 cases developed the AVF following operative interventions of different natures while our case developed AVF following a closed fracture treated non-operatively.
The case reported by Delaney et al. [12] resembles our case report with some differences. They reported an 11-years old boy who developed an AVF between anterior tibial artery and popliteal vein 12 weeks after closed fractures of the proximal tibia and fibula treated non -operatively. The AVF was presented much earlier than our case (12 weeks versus 1 year). The location of the AVF was more proximal (5.3 cm versus 13 cm from popliteal artery bifurcation to tibio-peroneal vessels) and different vessels were affected. The AVF was treated successfully by embolization with coils inserted through a microcatheter while in our case report it was treated with surgical ligation.
Peter et al. [10] also reported a case of post traumatic AVF originating from anterior tibial artery to the popliteal vein presented 11 weeks after closed fracture of proximal tibia and fibula treated with manipulation and casting in a 10 year old male patient.
This case report serves as reminder that the routine follow-up for fractures shouldn’t be taken casually but with continued consideration for the occult soft tissue injuries. The possibility of an AVF should be considered in case of persistent swelling after high-energy trauma of an extremity.