Wisam Majdi Abuzaid
Orthopedic Surgery Faculty of Medicine - Misurata University.
*Corresponding Author: Wisam Majdi Abuzaid, Orthopedic Surgery Faculty of Medicine - Misurata University
Received date: May 23, 2023
Accepted date: June 29, 2023
Published date: October 17, 2023
Citation: Wisam Majdi Abuzaid (2023) “Using of Soft suture anchor in repair of Acute Ulnar collateral ligament injuries of the thumb in Misurata - LIBYA’’. J Orthopaedic Research and Surgery, 4(1); DOI: http;//doi.org/06.2023/1.1036.
Copyright: © 2023 Wisam Majdi Abuzaid. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Ulnar collateral ligament (UCL) injuries of the metacarpophalangeal (MCP) joint of the thumb are common. Complete rupture can be a debilitating injury, resulting in decreased grip and pinch strength. The current study aimed to investigate the functional outcomes and complications of surgical repair of ulnar collateral ligament of thumb through using soft suture anchor 1,8 mm. Material And Methods: This study included 14 patients with acute UCL injury who were operated with primary repair with Soft Anchor–1.8mm Mini between April 2016 and May 2020. All patients were operated on using the same anchor in Misurata Medical centre and Misurata private hospitals. We use dash score and vas score; pre- and post-operative pain, disability , function and any complication occur post operation. Results: The mean pre- and post-operative VAS scores were3.85, the mean pre- and post-operative dash scores were 23.85, so the pain is decreased and function is improved after surgery. Complication postoperatively is Sensory disturbance consisted of reduced sensation or paraesthesia on the ulnar border of the thumb – this resolved in all cases, No failures of repair occurred, one case complicated with slight thumb restriction of movement. Conclusions : Surgical repair using the Soft Anchor–1.8 mm is an effective treatment method for acute total ulnar collateral ligament (UCL) rupture ,with a low complication rate no failures is detected postoperatively. Pain & stiffness were commonly reported but patients were satisfied with their outcome were generally mild & non-limiting , All patients returned to work
soft suture anchor, Ulnar collateral ligament, thumb,
Introduction
Ulnar collateral ligament (UCL) injuries of the thumb are among the most common injuries in the hand. In some populations, the incidence is as high as 50 per 100,000 and they are 10 times more common than their radial version. Acute injuries, commonly referred to as skier’s thumb, have been known to occur in various sporting activities in addition to their namesake, but are also common in manual laborers. So-called gamekeeper’s thumb, the chronic form of UCL insufficiency, has also been well documented. A stable, pain-free thumb base is not only essential for various sports and hobbies but also for activities of daily living, gripping, and key pinch. (1)
Insufficiency can lead to compromised grip and pinch, pain, and ultimately osteoarthritis. This article summarizes the current concepts in the management of these injuries in their acute and chronic forms. (2)
Ulnar collateral ligament (UCL) is the most important stabilizer protecting the thumb against valgus stress , Its injuries are typically seen as a result of valgus overloading after falls on an open hand or sport trauma. Patients usually present to emergency department with pain and swelling on the ulnar aspect of the thumb (3).
The diagnosis is made by valgus loading, which demonstrates thumb angulation over 35° upon extension and over 15° upon 30° flexion compared to the contralateral side. Plain films are useful for differentiating bone avulsion accompanying the injury. Injuries most commonly occur from the level of proximal phalanx where the ligament has distal attachment (4).
“skier’s thumb” for the acute injuries occurring in skiers due to the hyperabduction trauma to the base of the thumb while holding their ski poles during the fall .Other mechanism of injury include fall on outstretched hand leading to forceful radial and palmar abduction ,fall from two wheeler/bicycle wherein the thumb gets stuck behind the handle bar, other sports associated with thumb UCL rupture are soccer, hockey and basket ball,In children these injuries are rare however due to the presence of immature skeleton a hyperabduction trauma leads to Salter Harris Grade 3 avulsion of UCL insertion and rarely a complete tear is visible . Other associated injuries with tears of ulnar collateral ligament include avulsion fractures ,dorsal capsular tears and volar plate tears.Patients commonly come to the hospital with pain, swelling and ecchymosis around the MCP joint and tenderness is present on the ulnar aspect of the MCP joint ,On clinical examination ,a prominent palpable lump(Stener lesion) is palpated which represents the ulnar collateral ligament being proximally and superficially placed by the interposed adductor aponeurosis.It is seen in 64% to 87% of all complete ruptures (5).
There is pathological rotation of the thumb. Incomplete tears of UCL are managed conservatively with spica cast for 4-6 weeks and thus differentiating these tears from the complete ones is necessary as the latter is almost always managed surgically (1).
Surgery is mostly recommended for avulsion injuries (Stener lesion) Various fixation techniques and materials such as suture anchor, Kirschner wires, and direct repair have been described for primary surgical repair of UCL. All these techniques have their own technical challenges and all are open to some form of complications (4).
Fixation of osseous avulsion fractures with K wires is complicated by pin track infections and osteomyelitis, and repair with anchors with a classical metal and biomaterial content may result in complications including foreign body reactions, migration, and chondrolysis (6).
The new generation all-soft anchors are suture based anchors entirely composed of polyethylene, which minimize the amount of foreign material in bone by leaving only suture material behind, and are therefore considered least prone to complications. By conducting this study we aimed to assess clinical functional outcomes and complications of acute UCL repair using an all-soft anchor, (Neosys – Turkey ) (7)
Pic. (1) : (Soft anchor screws neosys) (7)
MATERIAL AND METHODS
Eighteen patients (13 males and 5 female ) diagnosed via a physical examination and U/S or MRI investigation between April 2016 and May 2020 with a total collateral ligament rupture in the Metacarpophalengeal joint thumb and treated surgically were evaluated prospectively in Misurata Medical Centre and Misurata private hospitals. Informed consent was obtained from all patients before enrollment in the study .
Inclusion criteria
Exclusion criteria
Eleven patients presented with a history of fall on outstretched hand while working , whereas 2 of them had history of fall from two wheeler with thumb getting caught in the handle of the vehicle , 5 patients with twisting injury during RTA .
Patients had pain,tenderness and ecchymosis at the base of the thumb on the ulnar aspect while some patients also had palpable swelling over the base similar to Stener lesion (particularly in those patients presenting >3weeks ).All patients were subjected to valgus stress testing in 30o MCP flexion and in extension and standard anteroposterior ,lateral and oblique views were taken to visualise any avulsion fracture and subluxation/dislocation of the proximal phalanx. The presence of 30 degree valgus laxity and 15degree difference as compared to the normal side with absence of a firm end point is considered to be a complete UCL tear and is an indication for operative treatment .
Out of the 18 patients, 4 had firm end point on valgus stress test and thus were diagnosed with partial UCL tear and managed conservatively with thumb spica and the rest 14 had absence of firm end point and were diagnosed to be complete UCL tears and thus were included in the study and operated using this technique.In those patients whom the valgus stress testing was painful,a local injection of 2ml lignocaine 2% infiltrated into the MCP joint improved the testing as described by Cooper et al. In case of an undisplaced fracture ,it is assumed that if the initial trauma couldn’t displace the fracture the stress during valgus test is not sufficient to displace the fracture.
Early diagnosis is important in any hand injury to prevent possible long-term effects. In addition to a comprehensive history and review of symptoms, we perform a physical examination of both hands and may order imaging test to confirm diagnosis. (valgus stress test) in comparison to the opposite thumb to determine if there is any laxity. This may be done under local anesthetic since it can be very painful. X-rays are used to visualize the bones and rule-out possible fractures. MRI (magnetic resonance imaging) and ultrasound may be ordered to observe the severity of soft tissue damage.
If damage to the UCL is minor non-surgical treatment may be indicated. Ice packs may be used during the first few days after injury to soo the pain and reduce swelling. we immobilize the thumb in a cast or splint which is worn continuously form the first 3 weeks or so. After that time the splint may be removed to perform hand therapy and strength exercises only. Total time in thumb splint is usually about 4 – 6 weeks.
Surgical technique done in 14 cases
|
|
|
|
(pic 2): Identification of adductor aponeurosis) |
(Pic 3): aponeurosis and the joint capsule were opened) |
PIC 4-5-6-7: UCL was held with matrix sutures and fixed into the bone with the freed 3.0 sutures
PIC 8 – 9: Identification of adductor aponeurosis
PIC 10-11: UCL was held with matrix sutures and fixed into the bone with the freed 3.0 sutures
At the second week the splint was intermittently removed and MP joint flexion, extension, and adduction were allowed; and at the fourth week the splint was completely removed and finger abduction was allowed
RESULTS
Outcome assessment
Fig. (1) : Quick DASH score (8)
Table (1): graduation of quick dash score (9)
|
Interpretation |
Score |
|
Very good |
0-5 |
|
Good |
6-15 |
|
Satisfactory |
16-35 |
|
Poor |
> 35 |
Fig. (2) : VAS score (10)
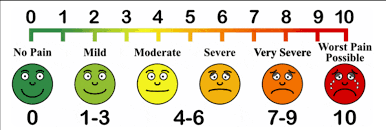
Table (1) : comparison Pre and postoperative VAS score and DASH score among studied patients
|
Case number |
Pre operative vas score |
Post operative vas score |
Pre operative dash score |
Post operative dash score |
|
1 |
6 |
2 |
38 |
15 |
|
2 |
7 |
2 |
41 |
15 |
|
3 |
8 |
3 |
39 |
14 |
|
4 |
5 |
2 |
36 |
11 |
|
5 |
5 |
1 |
36 |
11 |
|
6 |
6 |
2 |
8 |
14 |
|
7 |
5 |
0 |
34 |
11 |
|
8 |
5 |
1 |
38 |
13 |
|
9 |
4 |
2 |
37 |
13 |
|
10 |
5 |
2 |
38 |
11 |
|
11 |
7 |
2 |
39 |
11 |
|
12 |
6 |
1 |
37 |
12 |
|
13 |
7 |
2 |
37 |
11 |
|
14 |
5 |
2 |
36 |
12 |
|
Mean |
6 |
1.71 |
35.28 |
12.42 |
Fig. (3): Pre and postoperative VAS score among studied patients
Table (3): complications among studied patients
|
Complications |
Number of patients (in 1st six wks) |
% |
Number of patients (late after 6 wks) |
% |
|
Sensory disturbance |
4 |
28% |
1 |
7% |
|
Superficial infection |
1 |
7% |
0 |
0% |
|
Wound dehiscence |
2 |
14% |
0 |
0% |
|
Failure of UCL repair |
0 |
0% |
0 |
0% |
|
Thumb stiffness |
3 |
21% |
1 |
7% |
|
Hand and wrist stiffness |
3 |
21% |
0 |
0% |
Fig. (4): Early complications among studied patients
Fig. (5): Late complications among studied patients
DISCUSSION
Although some studies have reported conservative treatment methods to yield acceptable results for acute total UCL ruptures, Bowers et al. reported conservative treatment to have a failure rate of 50% for acute total UCL rupture (4).
Among 26 patients with total UCL rupture, Engel et al. (11) obtained satisfactory results for 16 patients treated surgically whereas 10 patients treated conservatively suffered from pain and instability. Persistent instability and associated arthritis following conservative therapy have made primary repair the preferred treatment modality for the management of acute total UCL ruptures. We did not observe persistent instability in any of our surgically managed cases.
Several repair techniques and materials have been reported for UCL ruptures, the major ones including Kirschner wires, intraosseous pull out sutures, suture anchors made of metal or various biomaterials, and suture - free Pushlock anchors (4)
Ali (12) compared conservative therapy and surgical repair of patients with collateral ligament injuries of the PIP joint. He discovered that surgical treatment offered superior results in those years. Unfortunately, it will take another 15 years for the first report on using suture anchors to repair the collateral ligament of the PIP joint.
Most reports in the literature concern thumb UCL rupture repair Furthermore, two author groups reported on the thumb RCL alone or with UCL repair Moreover, regarding PIP joint collateral ligament repair, few cohorts are reported in the literature (13)
Bui et al. (14) reported a systematic review of the literature concerning studies reporting the clinical results of the surgical repair of acute complete collateral ligament ruptures of PIP joints. They detected four studies reporting on 68 patients with acute ligament injuries of the PIP joint, 47 of whom underwent acute surgical repair ,Based on this systematic literature review, the surgical repair of an acute PIP joint collateral ligament rupture is feasible, although the published literature has both quantitative and qualitative flaws Compared with the existing literature regarding the clinical follow-up results of PIP joint collateral ligament rupture repair, our cohorts have the largest number of patients and longest follow-up period.
Sahin, (13) assessed 35 patients following the repair of an acutely ruptured UCL of the MCP thumb joint. He compared two suture materials. The first was a horizontal mattress suture using a 4/0 polybutylate- coated braided suture (nine patients), and the second method involved repairing with a prefashioned steel wire 16 patients). They concluded (after a mean 12.9 month follow-up) that both techniques were equally effective and using the more expensive steel wire, while technically satisfying and easy to perform, offers no clinical advantage over the simple suture.
Glickel et al. (15) described a technique of ligament(UCL of the MCP joint of the thumb) replacement for 26 chronic cases , They used a free tendon graft inserted through two holes at the base of the proximal phalanx and a single transverse hole in the metacarpal neck. The follow-up period averaged 4.5 years. They reported excellent results in 20 patients, good results in four, and fair results in two.
Landsman et al. (16) studied 40 patients with suspected complete ruptures who were treated with thumb immobilization for 8-12 weeks. They were followed up for an average of over 2 years. They reported that only 15% of patients did require surgical stabilization, whereas 85% of these patients had no signs of instability, pain, arthrosis, or stiffness.
Pichora et al. (17) also reported very good results with bracing, but three of the 32 patients at final follow-up reported failure of treatment with persistence of symptoms.
Gvozdenovic and Boeckstyns (18) described a new technique for reconstructing chronic lesions of the collateral ligaments of the MCP ligaments of the thumb, using a Bio-Tenodesis screw for the fixation of a tendon graft in a triangular manner with the proximal apex and allowing early mobilization, starting two weeks after the operation. The authors used this technique and reported a review of a consecutive series of 18 patients, and the mean follow-up period was 26 months. Their technique offers a short rehabilitation period with good functional results.
Katolik et al. (19) compared two 30-patient cohorts who had a complete rupture of the UCL of the MCP joint of the thumb [34].
The first group was treated with an intraosseous suture anchor followed by early mobilization, and the second group was treated with a pull-out suture tied over a button with cast immobilization. The mean follow-up time was 29 months. They concluded that both repair procedures were safe and effective for treating thumb UCL injuries.
Comparing to Dr William M. OLIVER study
|
|
Our study |
Dr William M. OLIVER |
|
Hospital and city |
Misurata medical centre assafwa private hospital (misurata – Libya) |
Royal Infirmary of Edinburgh( Edinburgh, UK) |
|
Number of patients |
14 |
34 |
|
mean of follow up |
6 months |
4 yrs |
|
Postoperative complications |
|
|
|
sensory disturbance |
4 - 1 |
3 |
|
superficial infection |
1 - 0 |
2 |
|
wound dehiscence |
2 - 0 |
1 |
|
failures of repair |
0 |
0 |
|
returned to work |
All patients |
All patients |
Limitation:
There are some limitations of our study. First, our study was conducted in a small sample size. Second, no comparison was made with other treatment methods.
On the other side, the strength of our study is that it is the first study to examine the efficacy of this fixation material in UCL injuries.
Conclusions
Surgical repair using the Soft Anchor–1.8 mm is an effective treatment method for acute total ulnar collateral ligament (UCL) rupture ,with a low complication rate no failures is detected postoperatively
Pain & stiffness were commonly reported but patients were satisfied with their outcome were generally mild & non-limiting, all patients returned to work. Larger studies are needed to compare this treatment method with other repair methods. (In the future).