Orthopaedic Research and Surgery
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2994-8738 | Journal DOI: 10.61148/2994-8738/JORS
Noah Khan
Plastic and Reconstructive Surgery, Shifa International Hospital, Islamabad, PAK
*Corresponding Author: Noah Khan, Plastic and Reconstructive Surgery, Shifa International Hospital, Islamabad, PAK.
Received date: June 23, 2021
Accepted date: July 08, 2021
Published date: July 13, 2021
Citation: Noah Khan. “Long Term Results in The Treatment of Avascular Necrosis of Femoral Head With Free Vascularized Fibular Graft’’. J Orthopaedic Research and Surgery, 2(3); DOI: http;//doi.org/03.2021/1.1016.
Copyright: © 2021 Noah Khan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective:
The objective of this study is to evaluate outcomes of Vascularized fibula flap used for AVN of femoral head. Outcomes were recorded by post-operative Harris hip and radiological improvement of femoral head.
Study design:
Retrospective study design
Study settings and duration:
Study was conducted at Department of plastic surgery, Shifa International Hospital. Study duration was one year (January 2019-January 2020). Cases were recruited from 2005-2018 (SIH) performed by same orthopedic surgeon and plastic surgeon.
Material and methods:
Data of 30 patients was reviewed. Ethical approval and consent of patient was taken before utilization of their data. Data regarding age, gender, etiology, Steinberg classification, pre and post-operative Harris Hip scores, radiological improvement, re-exploration, flap loss, fractures, donor site complications, conversion to total hip replacement. SPSS version 24 was used for data processing. Fissure exact test and chi-square test was applied. P value ≤0.05 was considered significant in our study findings.
Results:
Total 30 patients were included in study. There were 27(90%) male and 3(10%) female. Mean age was 28.3 years±5.1SD. Pre-operative Harris Hip scores were fair in 17 (56.7%) and poor in 13(43.3%) patients while post operatively these scores were excellent in 10(33.3%), good in 18(60%) and fair in 2(6.7%). Radiological improvement was seen in 20(80%) patients, 8(23.3%) showed no change and 2(6.7%) went into progression. Radiological improvement showed significant association with etiology (p=0.004) and AVN HIP (p=0.007).
Post-operative Harris Hip scores showed significant association gender (p=0.000), etiology (p=0.002) and AVN HIP (p=0.001).
Conclusion:
Vascularized fibular graft is an effective treatment option for avascular necrosis of femoral head in terms of improved radiological outcomes and post-operative Harris Hip scores. Furthermore, it is a hip-salvaging procedure in early pre-collapse stages, and a time-buying one when the femoral head has collapsed in young population.
Introduction:
Femoral head avascular necrosis accounts for 10000-20000 new cases each year in United States [1]. It is a type of osteonecrosis and bone infarction that results after disruption of blood supply to femoral head. Incidence of femoral head avascular necrosis is 1.9/100000 individuals in Japan [2]. Etiology of Avascular necrosis of femoral head include femoral neck fractures, chronic alcohol and steroid use, congenital causes and coagulopathy.
Literature did not report any exact pathophysiological mechanism of avascular necrosis. Avascular necrosis of femoral head pathophysiology is multifactorial. During this necrosis bone marrow and osteocytes death is due to inadequate blood supply to proximal femur subchondral bone [3]. Cell death is associated with femoral head collapse and relevant osteoarthritis.
Management of femoral head avascular necrosis involves life style modifications and surgical treatment. Apart from pharmacological and surgical treatment, life style modifications are very important in overall treatment of avascular necrosis of femoral head. Life style modifications include alcohol cessation, pain control medications, restricted weight bearing, discontinuation of steroid therapy, physical therapy and targeted pharmacological therapy [4]. Surgical options include joint preservation and joint replacement. Joint preservation includes core decompression, osteotomy, bone grafts and use of biologics and cellular therapies. Narrowing of the joint space and acetabular involvement are contraindications to surgery which is designed to preserve the femoral head. Collapse of the femoral head and depression of more than 2 mm are relative contraindications for a free vascularized fibular graft.
Free vascularized fibular grafting (VFG) is a joint preserving surgical procedure with a midterm survival rate of 61 to 96% for 4-7 years. Berend et al. reported that survival rate of vascularized fibular graft is 67.4% for 2 years and 64.5% for 5 years in patients with femoral head osteonecrosis5. Kim et al. reported that vascularized fibular graft results in better clinical results and more effective for prevention of femoral head collapse with larger osteonecrotic lesion and Steinberg stage IIC6. The rationale for vascularized bone grafting is based on four concepts:
1.Decompression of the femoral head which may interrupt cycle of ischemia and interosseous hypertension that is believe to contribute to the disease.
2.Excision of sequestrum which may inhibit revascularization of the femur head.
3.Filling of the defect that is created with osteoinductive cancellous graft and a viable cortical strut to support the subchondrals surface and to enhance the revascularization process.
4. Protection of healing construct by a period of limited weight bearing.
Joint Replacement include Total Hip Replacement and is an excellent option in the older patient with collapse and deformity of the femoral head [7]. In younger patients, however, arthroplasty with its limited life-span and increased morbidity is a poorer option. Surgical alternatives for a young patient with a large osteonecrotic lesion are limited to femoral resurfacing arthroplasty and bipolar hemiarthroplasty.
Avascular necrosis is a debilitating disease commonly in young adults requiring vigilant attention of healthcare professionals [8]. Several studies discussed short and midterm results of fibular graft, however, data available of long term efficacy of graft is not enough to reach any conclusion. So, present study aims to determine frequency of radiological improvement and Harris Hip scores following free vascularized fibular graft in patients diagnosed with avascular necrosis of femoral head.
Material and Methods:
A retrospective study was conducted year from January 2019-January 2020 at department of plastic surgery, Shifa International Hospital. In this study 30 patients were recruited in which surgeries were performed by the same orthopedic and plastic surgeon over the period of 15 years. All patients had joint preservation surgeries with vascularized fibula.
Ethical approval was taken from respective institute (Ref # 295-785-2019) and consent of patients was taken before utilization of their data. Inclusion criteria was based upon patients age >16-40 years, both genders, diagnosed with femoral head avascular necrosis, Steinberg classification I-III, AVN Hip and patients treated with free vascularized fibular graft. Patient with previous hip replacement surgeries, collapsed joint, severe steroid dependency and, serious co-morbidities were excluded from the study. Mean follow up period was 5 years with minimum of 3 years and maximum of 10 years. Follow ups were done through radiographs and clinical evaluation at least after 6 months and then yearly. Radiographic images were advised yearly basis for a minimum of 3 years and then depending of the follow up of the patients there after as needed. Hospital records were looked for information’s like age, gender and etiology. Outcomes in terms of post-operative Harris Hip scores, and radiological improvement were analyzed and recorded. Post-surgical complications like wound infection, fracture, flap-survival and conversion to THR were assessed. Each patient had free vascularized fibular grafting for unilateral hips, even in those cases where disease was bilateral. In bilateral disease we have reconstructed one side of the fibula as those patients are living a good quality of life so far.
Harris Hip score
A thorough clinical examination was done and rated by using Harris hip scores in all patients. At the time of surgery and at each follow-up examination, the Harris hip score was used for clinical evaluation and outcome was graded as excellent when the Harris hip score was greater than 90 points, good when it was between 80 and 89 points, fair when it was between 70 and 79 points, and poor when it was less than 70 points.). HARRIS HIP SCORE (100 points) has four components i.e. PAIN 1 item (0-44), FUNCTION 7 item (0-47), Absence of deformity 1 item (4 points) and Range of motion items (5 points).
Steinberg's classification
Pre-operative radiological scans (X-ray hip/MRI) were done to stage the disease by Steinberg classification. This classification is based on the radiographic appearance and location of lesion by quantifying the involvement of femoral head. According to this classification, Stage 0: normal or non-diagnostic radiographs, MRI/ bone scan and is diagnosed on histology, stage I: normal radiograph, abnormal bone scan and/or MRI, with minimal pain, stage II: cystic and sclerotic radiographic changes in femoral head and stage III: Subchondral collapse (crescent finding) without collapse. These patients were radiologically assessed for the progression or regression of the necrotic lesion and changes in the contour of the femoral head by the radiologist. (1) Improved—Those cases in which the osteonecrosis had healed or was being replaced with new bone formation. For the Stage II lesion, the crescent had disappeared or the density of cystic lesion had increased with trabecular formation of the tip of the vascularized fibula. For the Stage III lesion, the collapsed lesion healed or became more rounded with trabecular formation of the tip of the vascularized fibula; (2) No change—compared with the preoperative status; and (3) Progressed—Those cases with progression observed based on stage or those with more than 3-mm of collapse.
Surgical technique:
All procedure received general anesthesia in spine position. Harvesting of vascularized fibula was done from ipsilateral leg (lateral approach) as mentioned by Urbaniak et al. A lateral approach (proximal thigh) was used for exposure of proximal part of femur from tensor fasciae latae and vastus lateralis. A guided pin was inserted (from sub-trochanteric region to necrotic lesion) in femoral head using fluoroscopic control. Reamers of size ranging from 8-19 cm in diameter were used for tunnel creation. Necrotic to subchondral bone was curetted using high speed burr under fluoroscopic image control. The average length of the harvested fibula usually ranged from 8 to 10 cm. Introduction of fibula was done through tunnel. Fibula was positioned under subchondral bone of femora head (within cancellous bone chip). Recipient vessel i.e. descending branch of lateral circumflex iliac artery were identified, ligated distally and retrieved from proximal thigh wound for anastomosis with peroneal vessels. Vascularization of graft was confirmed through fibular graft bleeding from the proximal end. A posterior below the knee cast was done in all patients for at least 2 weeks. Postoperative thromboembolic prophylaxis was given and pedicle was monitored on Doppler throughout the hospital stay. Passive range-of-motion exercises were encouraged after removal of suction drains on Day 3. Postoperative rehabilitation included complete non-weight-bearing (wheelchair-bound) for 1 week, minimal weight-bearing and ambulation with crutches for 10 weeks, followed by partial weight-bearing for a total of 6 months. Patients were encouraged to bear full weight after this period.
Data analysis was done using SPSS version 24. We calculated mean and standard deviation for age. However, categorical and nominal variables were analyzed using frequency and percentages. Fissure exact and Chi-square test was applied to measure association between dependent and independent variables. P value ≤0.05 was considered statistically effective in our results.
Results:
Total 30 patients were included in study. There were 27(90%) male and 3(10%) female. Mean age was 28.3 years±5.1SD. Etiology was idiopathic in 16(53.3%), steroid induced in 5(16.7%), post traumatic in 8(26.7%), alcoholic in 1(3.3%) patients. According to Steinberg classification 6(20%) in type 1, 13(43.3%) in type 2 and 10(33.3%) in type 3 category. Among 30 patients 18 patients were having a unilateral disease and 12 patients with bilateral disease. (table 1)
Table 1
Demographic data
|
Variables n |
|
Average patient age (years) 28.3 (range, 16-40 years) |
|
Male: female 27:3 |
|
Etiology |
|
Idiopathic 16 (53.3%) |
|
Alcoholic 1 (3.3%) |
|
Posttraumatic 8 (26.7%) |
|
Steroid-induced 5 (16.7%) |
|
Steinberg classification |
|
Stage 1 6 (20%) |
|
Stage II 13 (43.3%) |
|
Stage III 10 (36.7%) |
|
AVN HIP |
|
Unilateral 24(80%) |
|
Bilateral 6 (20%) |
Pre-operative Harris Hip scores were fair in 17 ( 56.7%) and poor in 13(43.3%) patients while post operatively these scores were excellent in 10(33.3%), good in 18(60%) and fair in 2(6.7%). Majority of males showed good post-operative Harris Hip scores as compared to female (56.7% vs 3.3 %, p=0.000) but the number of the female in this patient were very less. Patients with unilateral AVN HIP showed good post-operative Harris Hip scores as compared to bilateral AVN HIP (P=0.001). Etiology also showed significant association with post-operative Harris Hip scores (p=0.002). However, Steinberg classification (p=0.819) and fracture (p=0.075) showed insignificant association with post-operative Harris Hip Scores as shown in table 2.
|
|
Excellent (90-100 scores) |
Good
(80-89 scores) |
Fair (70-79 scores) |
|
|
|
|
Gender
Males |
8(26.7%) |
17(56.7%) |
2(6.7%) |
Total
27(90%) |
P value
0.000 |
|
|
Female |
2(6.7%) |
1(3.3%) |
0(0%) |
3(10%) |
|
|
|
Steinberg classification |
|
|
|
|
|
|
|
Type 1 |
4(13.3%) |
2(6.7%) |
0(0%) |
6(20%) |
0.819 |
|
|
Type 2 |
3(10%) |
9(30%) |
1(3.3%) |
13(43.3%) |
|
|
|
Type 3 |
3(10%) |
7(23.3%) |
1(3.3%) |
11(36.7%) |
|
|
|
Etiology Idiopathic |
6(20%) |
10(33.3%) |
0(0%) |
16(53.3%) |
0.002 |
|
|
Steroid induced |
2(6.7%) |
2.(6.7%) |
1(3.3%) |
5(16.7%) |
|
|
|
Post traumatic |
2(6.7%) |
6(20%) |
0(0%) |
8(26.7%) |
|
|
|
Alcoholic |
0(0%) |
0(0%) |
1(3.3%) |
1(3.3%) |
|
|
|
AVN HIP Unilateral |
7(23.3%) |
16(53.3%) |
1(3.3%) |
24(80%) |
0.001 |
|
|
Bilateral |
1(3.3%) |
1(3.3%) |
4(13.3%) |
6(20.0%) |
|
|
Table 2: Association between Post-operative Harris Hip scores and independent variables
Radiological improvement was seen in 20(80%) patients, 8(23.3%) showed no change and 2(6.7%)went into progression. Among all the patients who showed radiological improvement 12(40%) had idiopathic etiology while 8(26.7%) had post traumatic etiology. Similarly, among all those with no change in radiology, 4(13.3%) showed steroid induced etiology while 4(13.3%) showed idiopathic etiology. Among all those with progression, 1(3.3%) showed alcohol induced, 1(3.3%) steroid induced etiology (p=0.004). Patients with unilateral AVN HIP showed radiological improvement 17(56.7%), no change in 3(10%) and no progression , while patients with bilateral AVN showed 3(10%) improvement, 1(3.3%) no change and static in 2(6.7%) patients (p=0.007). Gender (p=0.111), Steinberg classification (p=0.944) and fracture (p=0.183) showed insignificant association with radiological improvement as shown in table 2.
|
|
Radiological Improvement at 5th year Improved No change Progression |
Total |
P value |
||
|
Gender
Males |
17(56.7%) |
8(26.7%) |
2(6.7%) |
27(90%) |
0.111 |
|
Female |
3(610%) |
0(0%) |
0(0%) |
3(10%) |
|
|
Steinberg classification
|
|
|
|
|
|
|
Type 1 |
5(16.7%) |
1(3.3%) |
0(0%) |
6(20%) |
0 .944 |
|
Type 2 |
10(33.3%) |
3(10%) |
0(0%) |
13(43.3%) |
|
|
Type 3 |
5 (16.7%) |
4(13.3%) |
2(6.7%) |
11(36.7%) |
|
|
Etiology Idiopathic |
12(40%) |
4(13.3%) |
0(0%) |
16(53.3%) |
0.004 |
|
Steroid induced |
0(0%) |
4(13.3%) |
1(3.3%) |
5(16.7%) |
|
|
Post traumatic |
8(26.7%) |
0(10%) |
0(0%) |
8(26.7%) |
|
|
Alcohol |
0(0%) |
0(0%) |
1(3.3) |
1(3.3%)
|
|
|
|
|
|
|
|
|
|
AVN HIP Unilateral |
17 (56.7%) |
7(23.3%) |
0(0%) |
24(80%) |
|
|
Bilateral |
3 (3.3%) |
01(3.3%) |
2(3.3%) |
6(20.0%) |
|
Table 2: Association between Radiological improvement and independent variables
There was no perioperative mortality, flap loss reported in our study. Among all the patients, 4(13.3%) showed superficial infection, fracture was reported in 2(6.7%) patient. Conversion to total hip replacement >10 years was in 5(16.7%) patients, 5-10 years in 3(10%) patients while no conversion in 22(73.3%) patients in less than 5 years.
|
Complications |
No of patients |
|
Superficial infection |
4(13.3%) |
|
Fracture |
2(6.7%) |
|
Conversion to Total Hip Replacement >10 years 5-10 years |
5 (16.7%) 3 (10%) |
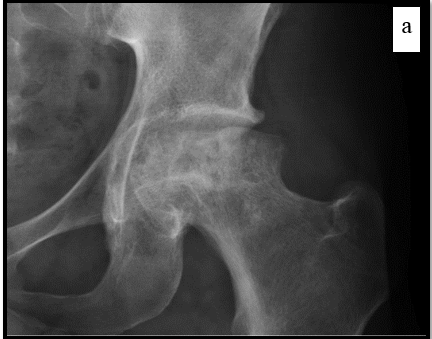


Young male presented with AVN of left femoral head and reconstruction done with vascularized fibular strut.a) xray of the hip showing subchondral cyst and irrefular contour of the femoral head.b,c) Over the period of 5 years the contour of the head improved and bone density in the sub chondral region has increased.
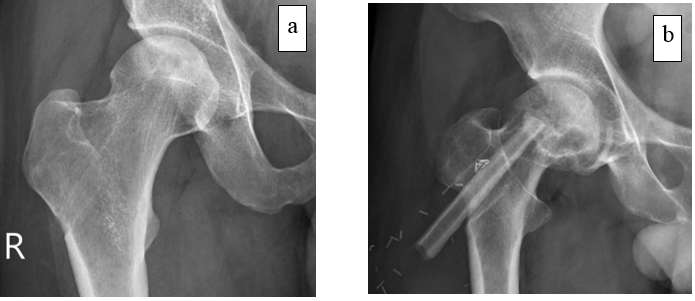

Figs. 2-A.: Anteroposterior radiographs of the right hip of a twenty-one-year-old man who had stage-2 disease.
Fig. 2-B: Post-operative radiograph obtained at 3 years shows adequate placement of the fibular graft.
Fig. 2-C: A radiograph taken 5 years after the operation showing no progression of the disease.
Fig 2 –D: The joint space is preserved and the patient remains asymptomatic 8 years after the reconstruction.
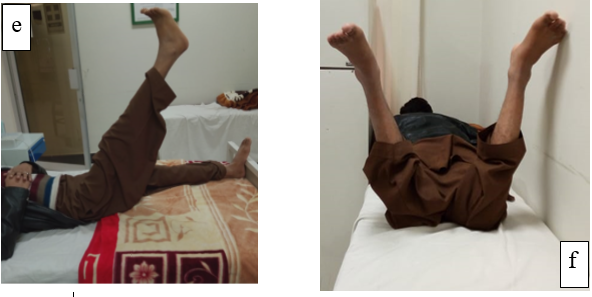
Figs. 3-e: Assessment of post op harris hip score which showed improved range of motion with no pain (flexion)
Fig. 3-f,g: Improved and pain free external and internal rotation of the hip
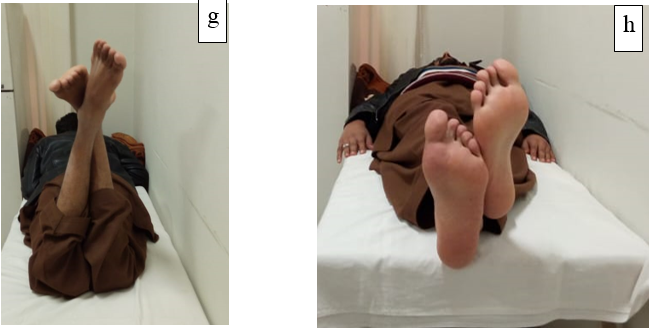
Fig. 3-h: no pain with adduction of the hi


Discussion:
Avascular necrosis of the femoral head is also known as osteonecrosis or bone infarct that most commonly affects younger adults [8]. The pathophysiology of AVN femoral head are not well understood. In AVN of femoral head the articular surface of the femoral head loses the support of the subchondral bone because of the blood disruption subchondral bone dies and without the underlying support of this bone, the arch of the femoral head can flatten and collapse. As the disease progresses, patients experience increased pain and dysfunction, often resulting in severe disability [9]. Once articular surface collapse begins, rapid development of arthrosis is imminent, further limiting the patient [10]. Osteonecrosis is associated with bone death leading towards collapse and cartilage destruction (secondary to development of degenerative changes [11].
The goal of all forms of treatment is to maintain the patient’s anatomy as long as possible, delaying the need for arthroplasty in this young patient population [12]. Treatment of the disease focuses on preservation or restoration of the femoral head blood supply and structural support within the femoral head. This in turn aims to arrest osteonecrosis and theoretically allow for return of normal bone metabolism
Phemister first described the use of bone graft for treatment of femoral head osteonecrosis in 1930[13]. Non-vascularized fibular bone graft was used to fill the space left behind after surgical removal of the necrotic bone and this bone graft would act as support for the femoral head articular surface and scaffolding for influx of progenitor cells and the laying down of new bone. Dr. JR Urbaniak reported 103 cases of hip treated with VFG in 1995. The advantage of vascularized bone graft is the inclusion of a new blood supply at the time of surgery and increasing the function of the graft beyond mere scaffolding for slow-moving creeping substitution. Direct revascularization of the bone allows for the invasion of osteoinductive progenitor cells, revitalizing the once necrotic zone, leading to restoration of a healthy subchondral plate. Improvement in outcome scores between vascularized and non-vascularized bone grafting is reported as 70 versus 35 %, and the rate of conversion to total hip replacement was nearly double in the non-vascularized group [14]
Conservative treatment is indicated in early stages of disease to the reduce risk of femoral head collapse i.e. decreased weight bearing, Statins and bisphosphonates and to reduce risk factors (e.g., smoking cessation, alcohol abstinence, reduce corticosteroid use if possible). Surgery is indicated if conservative treatment fails and/or when bone structure is compromised and frequently performed in early stages to improves prognosis.
There are a variety of hip-sparing management strategies for these patients including core decompression [15,16], nonvascularized bone grafts [17,18], free vascularized fibular grafts [19,20], stem cell injection [21], peritrochanteric osteotomies [22], electrical stimulation [23,24], and activity modification [25]. Regardless of the treatment, patients remain at a risk of further progression of disease and may ultimately require THA.
Joint Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant, that is, a hip prosthesis. Hip replacement surgery can be performed as a total replacement or a hemi (half) replacement. A total hip replacement (total hip arthroplasty or THA) consists of replacing both the acetabulum and the femoral head while hemi-arthroplasty generally only replaces the femoral head. Risks and complications in hip replacement are similar to those associated with all joint replacements. They include infection, dislocation, limb length inequality, loosening, impingement, osteolysis, metal sensitivity, nerve palsy, chronic pain. Hip replacement therapy is associated with increasing rate of revised surgery so greater than 50 years should be closely evaluated for total hip arthroplasty [26].

AVN usually affects young population so in our study mostly the patients were less than 40 years and underwent reconstruction with fibular graft. In Pakistan where most of the population is from middle class and can’t afford expensive implants that has to be revised in about 5-6 years as they have to go in average four to five joint replacement surgeries during their whole life span. By doing this procedure not only you delay the progression of the disease but you take them through their young age till the time thy would need THR. (chart 1)
In our study male’s ratio was more than female (90% vs 10%), affects male population more than female limiting our study. In the current study, clinical outcomes of steroid-induced and alcohol induced osteonecrosis contributed to poor outcomes. In our population idiopathic and post-traumatic were the main etiology of AVN femoral head but in western countries alcohol and steroid induced AVN is the main etiology [26,27]

In our study, 33.3% patients showed excellent and 60% good post-operative Harris Hip scores. The average Harris hip scores had improved at the latest follow-up evaluation, compared with the preoperative values (p =0.819). For the Stage-I hips, the average score improved from 75to 92 points; for the stage-II hips, from 69 to 85 points; for the stage-III hips, from 41 to 82 points. However, yoo et al. reported that `according to clinical evaluation patients showed 17% good, 7% showed fair and 2% showed poor outcomes. However, 71% were improved radio graphically and 11% showed worse radiographic results [28]. Kawate et al. reported that patients with small osteonecrosis in Steinberg stage I and II is an important indication for vascularized fibular graft. However, they reported large osteonecrosis with >300 degree and severe pre-operative collapse as major contraindication for fibular vascularized graft [29].
In this study radiographic improvement is associated with etiology (p=0.004). Berend et al reported there was statistical difference was found in treatment outcomes [30]. Weinstein et al. reported the apoptosis of osteocytes in the femoral of patients with steroid-induced osteonecrosis of the hip [31]. Similarly, another study reported that patients with alcohol related osteonecrosis and idiopathic hip etiology are more likely to have poor prognosis than corticosteroid induced osteonecrosis [32]. Unal et al. reported that findings similar to or study; they reported that clinical scores and outcomes were worse in steroid induced osteonecrosis as compared to other etiologies. Radiological improvement showed insignificant association with Steinberg classification [33]. Magnussen et al. reported that femoral head sparing surgical procedures are used to restore femoral head contour with advanced osteonecrosis. Steinberg stage IV was associated with 53% rate of radiographic progression with mild collapse and 75% associated with severe collapse [34]
In present study, Conversion to total hip replacement >10 years was in 16.7% patients and 5-10 years in 6.7% patients. Sotereanos et al. reported that 30% patients had high probability of total hip replacement after fibular vascular grafting of femoral head [35]. Another similar study reported that 44% patients underwent total hip replacement due to two negative factors including alcohol use and steroid induction therapy [36]. In preoperative collapse (Steinberg's stages I and II) is a major indication for free vascularized fibular grafting while steroid-induced osteonecrosis is relative contraindication, and large osteonecrosis with severe preoperative collapse is a major contraindication. Urbaniak and Harvey described an 83% survival of the fibular graft in 646 procedures after follow-up ranging from one to 17 years [37]
Limitation: small sample and retrospective study design limits generalizability of study
Conclusion:
Free vascularized fibula graft, especially in younger patients, is a salvaging procedure of the necrotic femoral head in early pre-collapse stages. In post-collapse osteonecrosis, the procedure appears to delay the need for total hip arthroplasty in the majority of patients. It is also very effective in terms of improved radiological outcomes and post-operative Harris Hip scores. There is Improved quality of life and yields extremely good results, particularly in pre-collapse stages of disease in young patients. Residual fibular defect of the donor site does not impair the functions of daily living.